Introduction: Prognostic and Predictive Factors
TERMINOLOGY
Definitions
Prognostic factors
Predict patient clinical course in terms of risk of disease recurrence and death
Provide information about patient outcome based on
Patient-related factors: Age, menopausal status, performance status, comorbidities
Tumor-related factors: Lymph node staging, tumor size, grade, histologic type, lymph-vascular invasion
Extensively clinically validated as useful in determining probability of local &/or distant disease recurrence
Basis for clinical risk assessment and decisions on the need for adjuvant systemic therapy
Prognostic factors are robust in terms of their ability to predict disease recurrence
Prognostic factors are less accurate/successful at predicting patient response to systemic adjuvant therapy
Prognostic factors are important whether evaluated prior to therapy or after neoadjuvant therapy
After treatment, response to treatment and amount of residual disease are important prognostic factors
AJCC staging both before and after treatment provide significant prognostic information, especially in combination
Prognostic factors are clinically most useful in helping to identify a subset of patients with small (< 2 cm), node-negative cancer who may benefit from systemic therapy
Predictive factors
Predict the likelihood that patient will benefit from adjuvant treatment regimens including
Hormonal therapy
Chemotherapy
Biologic and targeted therapies
Provide information on the likely outcome following a specific treatment regimen
Development of new treatment regimens and novel targeted agents has led to a shift from risk assessment to treatment responsiveness
Better patient selection for specific treatments
Improved patient response rate
Reduction of toxicity from therapies that will be unlikely to be of benefit
Some factors, including ER, PR, and HER2, are both prognostic factors and predictive factors
CLINICAL IMPLICATIONS
Major Pathologic Prognostic Factors
Used for AJCC/UICC TNM staging (7th edition, 2010)
Used to combine patients into groups with similar likelihood of survival
Majority of factors are determined by readily available standard techniques
Useful to compare patients over time and in diverse locations
Essential for grouping patients for clinical trials and other studies
Include local extent of cancer in the breast, regional lymph node metastasis, and distant metastasis
Staging is prognostically important for carcinomas prior to treatment and after neoadjuvant treatment
Patients are divided into 5 stages with different survival rates at 10 years
Stage 0: DCIS; > 95% survival
Without screening, this group is very small (< 5% of breast cancers)
In screened populations, 20-30% of carcinomas are DCIS
Stage I: Invasive carcinomas < 2 cm with negative nodes or only micrometastases; > 90% survival
Approximately 50% of patients with invasive carcinoma
Incidence has increased with screening
Stage II: Invasive carcinoma up to 5 cm with 1-3 lymph node metastases or carcinoma > 5 cm with negative nodes; ˜ 60% survival
Approximately 30% of patients with invasive carcinoma
Incidence has decreased with screening
Stage III: Locally advanced disease (skin ulceration or chest wall invasion or inflammatory carcinoma) ± lymph node metastases or metastases in ≥ 10 lymph nodes; ˜ 40% survival
Only 5-10% of patients
Incidence has decreased due to greater awareness and earlier detection
Stage IV: Distant metastases; < 10% survival
Only 5-10% of patients
Incidence has not changed substantially over time
Likely a subset of carcinomas that metastasize early prior to possible detection by screening
Size of invasive carcinoma (AJCC T1-3)
Size of an invasive carcinoma is an independent prognostic factor
Does not include associated carcinoma in situ
Correlated with likelihood of lymph node metastasis
Clinical, radiologic, gross, and microscopic information should be used to determine best size for T classification
Palpable carcinomas have worse prognosis compared with nonpalpable carcinomas, detected by screening, of same size
Tumor size directly correlates with number of involved lymph nodes and an increased risk of recurrence
For node-negative patients, tumor size is routinely used to make adjuvant treatment decisions
Patients with carcinomas ≤ 1 cm have an excellent prognosis, and selected patients have little benefit from systemic therapy
AJCC T classification separates majority of carcinomas by size
T1 carcinomas are ≤ 2 cm in size
T1mi: ≤ 0.1 cm (microinvasion)
T1a: > 0.1 cm but ≤ 0.5 cm
T1b: > 0.5 cm but ≤ 1 cm
T1c: > 1 cm but ≤ 2 cm
T2: > 2 cm but ≤ 5 cm
T3: > 5 cm
T4: Tumor of any size with direct extension to chest wall or skin involvement or inflammatory carcinoma
Regional lymph nodes (AJCC N1-3)
Prognosis diminishes with each additional lymph node metastasis
N0: Negative nodes, 82.8% 5-year survival
N1a: 1-3 positive nodes, 73% 5-year survival
N2a: 4-9 positive nodes, 45.7% 5-year survival
N3a: 10 or more positive nodes, 28.4% 5-year survival
Prognosis is dependent on size of the metastasis
Macrometastases measure > 2 mm and have prognostic significance
Isolated tumor cells (< 0.2 cm or < 200 cells) & micrometastases (between isolated tumor cells & macrometastases) have very small effect on prognosis compared to node-negative women
Total number of positive nodes includes macrometastases and micrometastases but not isolated tumor cells
Patients with only micrometastases are classified as stage I in AJCC 7th edition manual
Subset (10-30%) of node-negative patients eventually develop distant metastases
Some of these carcinomas may metastasize to nodal basins that are generally not sampled (e.g., internal mammary nodes)
Other carcinomas may metastasize primarily via blood vessels (e.g., spindle cell carcinomas)
Lymph nodes are removed or sampled primarily for prognostication
Removal of positive lymph nodes has little or no effect on survival
Distant metastases (AJCC M1)
Generally detected clinically or radiologically
Patients with indeterminant findings may undergo biopsy for confirmation
M1 metastases are detected by clinical or radiologic means &/or are pathologically shown to be > 0.2 mm
M0 (i+) metastases are detected by microscopy or other tests and are ≤ 0.2 mm; are not evident clinically or radiologically or by symptoms or signs
Patients with M1 (stage IV) disease have a poor prognosis, < 10% survival at 10 years
Patients who present with distant metastases at a long interval after diagnosis have a better prognosis
Indicative of a carcinoma with a slower growth rate
Most common sites of metastasis are bone, lung, brain, and liver
Bone is most common site and, in ER-positive cancers, may occur many years after diagnosis
Brain metastases are relatively more common in HER2-positive cancers and triple negative cancers
Pathologic M0 can only be defined at autopsy
For living patients, only clinical M0 is applicable
MX was eliminated as a term in the AJCC 7th edition
Skin involvement, chest wall involvement, or inflammatory carcinoma (AJCC T4)
Extensive skin &/or chest wall involvement originally identified in patients with very large locally advanced carcinomas who would not benefit from surgery
Current prognosis is improved with better surgical and adjuvant treatment
Difficult to study as these patients are now quite uncommon
T4a: Extension to chest wall
Does not include adherence to or invasion of pectoralis muscle
T4b: Skin involvement
Ulceration of skin: Does not include ulceration due to a prior surgical procedure or Paget disease of the nipple
Small superficial carcinomas with ulceration are unlikely to have the poor prognosis associated with large ulcerating carcinomas (but do have increased likelihood of lymph node metastases)
Satellite skin nodules: Invasive carcinoma in skin not contiguous with the main carcinoma; generally due to extensive lymph-vascular invasion
Edema (including peau d’orange) is not sufficient for diagnosis of inflammatory carcinoma; this finding cannot be determined in surgical excisions and is rarely used for staging
T4c: Features of both T4a and T4b
T4d: Inflammatory carcinoma
Defined by clinical sign of diffuse erythema and edema (peau d’orange) involving 1/3 or more of skin of the breast
Correlates with a type of carcinoma characterized by extensive dermal lymph-vascular invasion
Pathologic finding of dermal lymph-vascular invasion has a poor prognosis, but in absence of clinical signs is insufficient for classification as inflammatory carcinoma
Additional Pathologic Prognostic Factors
Important for prognosis but not currently incorporated into AJCC staging
Histologic grade
Used to stratify breast cancer patients into favorable (well-differentiated) and less favorable (poorly differentiated) outcome groups
A number of different breast cancer grading systems have been clinically validated
Nottingham combined histologic grade (Elston-Ellis modification of Scarff-Bloom-Richardson grading system) is recommended by the College of American Pathologists, the American Joint Commission on Cancer, and the European Working Group on Breast Screening Pathology
Grade is based on evaluation of glandular (acinar)/tubular differentiation, nuclear score, and mitotic score
Adherence to strict morphologic criteria is needed for reproducibility so that grade is reliably useful as a prognostic factor
Grade 2 cancers may be a mixture of grade 1 and 3 cancers
Proliferative rate may be used to reclassify grade 2 cancers
Extensive necrosis (> 1 high-power field) identifies grade 3 cancers with a particularly poor prognosis
Necrosis is predictive of a good response to chemotherapy
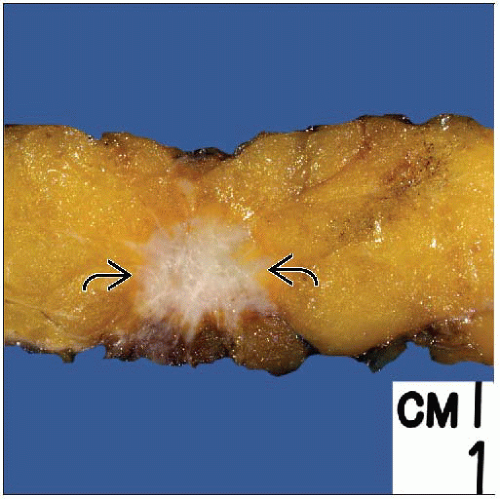
Lymph-vascular invasion (LVI)
Peritumoral LVI has prognostic significance for risk of local and distant recurrence
Recurrence for stage I disease with LVI is ˜ 38% compared with 22% in its absence
Closely associated with lymph node metastases but is an independent factor
Prognosis is diminished if both LVI and nodal metastases are present
Currently unnecessary to distinguish small capillaries from lymphatics using IHC markers
Both have prognostic significance
Special histologic types of invasive carcinoma
Some histologic types of breast cancer have a generally better prognosis compared with carcinomas of no special type (“ductal carcinomas”)
Strict criteria in diagnosis of these special types of breast cancer are important to maintain prognostic significance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree