Intratubular Germ Cell Neoplasia
Steven S. Shen, MD, PhD
Mahul B. Amin, MD
Jae Y. Ro, MD, PhD
Key Facts
Terminology
Proliferation of uncommitted neoplastic germ cells within seminiferous tubules
Clinical Issues
Often present in association with malignant germ cell tumor
Microscopic Pathology
Intratubular proliferation of malignant germ cells distributed along periphery of tubules or filling tubules completely (seminoma in situ)
Large atypical cells with centrally located nuclei, thickened nuclear membrane, evenly distributed chromatin, and prominent nucleoli
Tumor cells with abundant clear to faintly eosinophilic cytoplasm
Pagetoid extension of ITGCN into rete testis may be seen; more frequent in nonseminomatous germ cell tumors than in seminoma
Ancillary Tests
Positive for PLAP, CD117, Podoplanin(D2-40), Oct3/4
Negative for cytokeratin, α-fetoprotein, CD30(BerH2) (may be positive in intratubular embryonal carcinoma)
Top Differential Diagnoses
Normal spermatogonia
Malignant lymphoma (intratubular)
Metastatic carcinoma or melanoma (intratubular)
ITGCN with microscopic invasive seminoma
Spermatocytic seminoma (intratubular)
TERMINOLOGY
Abbreviations
Intratubular germ cell neoplasia (ITGCN)
Synonyms
Carcinoma in situ; ITGCN, unclassified type
Definitions
Proliferation of uncommitted neoplastic germ cells within seminiferous tubules; usually aligned at periphery of tubules
CLINICAL ISSUES
Epidemiology
Incidence
Present in ipsilateral uninvolved testis in 80-95% of patients with malignant germ cell tumors
Present in contralateral testis in 5-8% of patients with malignant germ cell tumors
Presentation
In cryptorchid testis or in association with malignant germ cell tumor
Risk factors
Cryptorchidism
Microlithiasis
Gonadal dysgenesis with Y chromosome
Family history (1st-degree male relative)
Androgen insensitivity syndrome
Treatment
Surgical approaches
Unilateral ITGCN usually managed by active surveillance or orchiectomy
Bilateral ITGCN may be treated by orchiectomy
Radiation
May be used for bilateral ITGCN
Prognosis
May progress to seminomatous or nonseminomatous germ cell tumors in about 50% of cases within 5 years
IMAGE FINDINGS
General Features
Usually no abnormalities or microlithiasis on ultrasound
MACROSCOPIC FEATURES
General Features
No demonstrable testicular mass; testis size may be normal or smaller
MICROSCOPIC PATHOLOGY
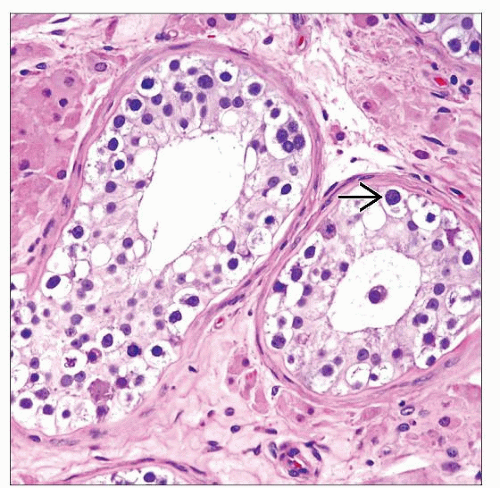
Histologic Features
Intratubular proliferation of malignant germ cells distributed along periphery of tubules
Seminiferous tubules may be atrophic, decreased in diameter, and may have thickened basement membrane
Large atypical cells with prominent cell borders, centrally located nuclei with enlarged nuclei, evenly distributed chromatin, and prominent nucleoli
Tumor cells with abundant clear to faintly eosinophilic cytoplasm
Tubules with decreased or absent spermatogenesis
May be associated with microlithiasis
Pagetoid extension of ITGCN into rete testis may be seen; more frequent in nonseminomatous germ cell tumor than in seminoma
Cytologic Features
Large atypical cells with abundant clear to faintly eosinophilic cytoplasm; mitoses may be seen
Predominant Pattern/Injury Type
Intratubular growth pattern, no mass formation
Predominant Cell/Compartment Type
Germ cells, uncommitted atypical germ cells, seminomatous/undifferentiated
ANCILLARY TESTS
Histochemistry
PAS-diastase
Reactivity: Positive but sensitive to diastase
Staining pattern
Cytoplasmic
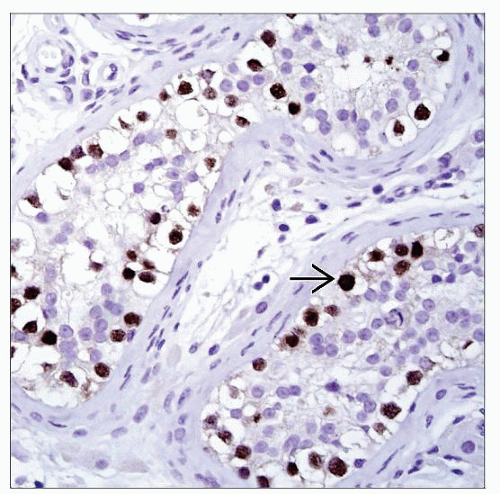
Immunohistochemistry
Positive for CD117, Podoplanin(D2-40), Oct3/4, and PLAP
Negative for cytokeratin, α-fetoprotein, and CD30(BerH2)
DIFFERENTIAL DIAGNOSIS
Normal Spermatogonia
Usually accompanied by mixture of spermatogonia, spermatocytes, spermatids, and spermatozoa
No tubular atrophy or thickening of peritubular tunica basement membrane
Lacks prominent nucleoli
Negative for CD117, Podoplanin(D2-40), Oct3/4, and PLAP
Malignant Lymphoma (Intratubular)
Usually associated with diffuse interstitial infiltrative growth
Positive for CD45(LCA), CD20, and CD3
Negative for germ cell tumor markers
Metastatic Carcinoma or Melanoma (Intratubular)
Metastatic carcinoma or melanoma may be intratubular; usually more pleomorphic with mitoses
Metastatic carcinoma positive for pankeratin, EMA/MUC1, and tissue-specific markers (TTF-1, PSA, etc.)
Melanoma positive for S100 and HMB-45
ITGCN with Microscopic Invasive Seminoma
Lymphoplasmacytic infiltrate in interstitium
Atypical tumor cells may be scattered among lymphocytes
Spermatocytic Seminoma (Intratubular)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree