Integumentary System
The integumentary system, the largest and heaviest body system, includes the skin—the integument, or external covering of the body—and the epidermal appendages, including the hair, nails, and sebaceous, eccrine, and apocrine glands. It protects the body against injury and invasion of microorganisms, harmful substances, and radiation; regulates body temperature; serves as a reservoir for food and water; and synthesizes vitamin D. Emotional wellbeing, including one’s responses to the daily stresses of life, is reflected in the skin.
Skin
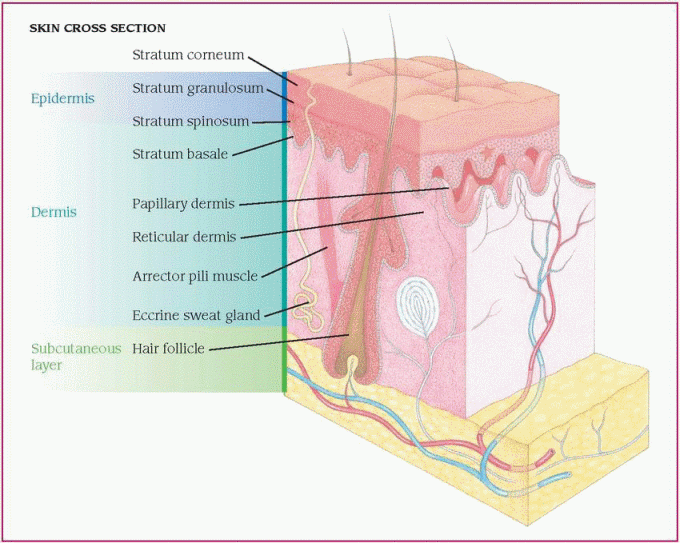
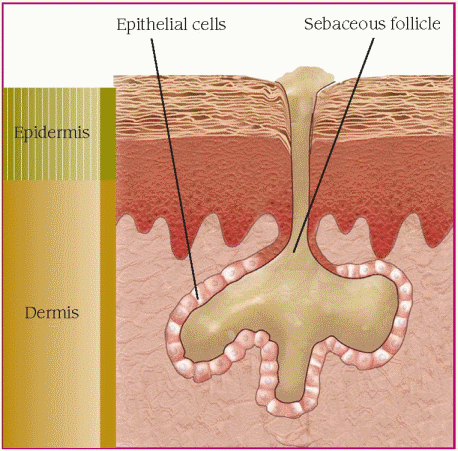
The skin is composed of three layers: the epidermis, dermis, and subcutaneous tissues. The epidermis—the outermost layer—is thin and contains sensory receptors for pain, temperature, touch, vibration, pressure detection, and itching sensation. The epidermal layer has no blood vessels and relies on the dermal layer for nutrition. The dermis contains connective tissue, the sebaceous glands, and some hair follicles. The subcutaneous tissue lies beneath the dermis; it contains fat and sweat glands and the rest of the hair follicles. The subcutaneous layer can store calories for future use in the body. (See Close-up view of the skin, page 558.)
Hair and nails
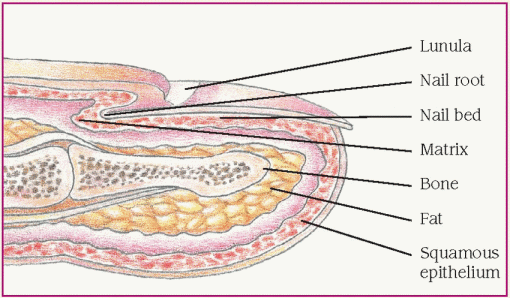
The hair and nails are considered appendages of the skin. Both have protective functions in addition to their cosmetic appeal. The cuticle of the nail, for example, functions as a seal, protecting the area between two portions of the nail from external hazards. (See Nail structure, page 558.)
Glands
The sebaceous glands, found on all areas of the skin except the palms and soles, produce sebum, a semifluid material composed of fat and epithelial cells. Sebum is secreted into the hair follicle and exits to the skin surface. It helps waterproof the hair and skin and promotes the absorption of fat-soluble substances into the dermis.
The eccrine glands produce sweat, an odorless, watery fluid. Glands in the palms and soles secrete sweat primarily in response to emotional stress. The other remaining eccrine glands respond mainly to thermal stress, effectively regulating body temperature.
Located mainly in the axillary and anogenital areas, apocrine glands have a coiled secretory portion that lies deeper in the dermis than the eccrine glands. These glands begin to function at puberty and have no known biological function. Bacterial decomposition of the apocrine fluid produced by these glands causes body odor.
Skin color depends on four pigments: melanin, carotene, oxyhemoglobin, and deoxyhemoglobin. Each pigment is unique in its function and effect on the skin. For example, melanin, the brownish pigment of the skin, is
genetically determined, although it can be altered by exposure to sunlight. Excessive dietary carotene (from carrots, sweet potatoes, and green, leafy vegetables) causes a yellowing of the skin. Excessive oxyhemoglobin in the blood causes a reddening of the skin, and excessive deoxyhemoglobin (not bound to oxygen) causes a bluish discoloration.
genetically determined, although it can be altered by exposure to sunlight. Excessive dietary carotene (from carrots, sweet potatoes, and green, leafy vegetables) causes a yellowing of the skin. Excessive oxyhemoglobin in the blood causes a reddening of the skin, and excessive deoxyhemoglobin (not bound to oxygen) causes a bluish discoloration.
Pathophysiologic changes
Clinical manifestations of skin dysfunction include the inflammatory reaction of the skin and the formation of lesions.
INFLAMMATORY REACTION
An inflammatory reaction occurs with injury to the skin. The reaction can occur only in living organisms. Although a beneficial response, it’s usually accompanied by some degree of discomfort at the site. Irritation changes the epidermal structure and consequent increase of immunoglobulin E activity. Other classic signs of inflammatory skin responses are erythema, edema, and warmth, due to bioamines released from the granules of tissue mast cells and basophils.
FORMATION OF LESIONS
Primary skin lesions appear on previously healthy skin in response to disease or external irritation. They’re classified by their appearance as macules, papules, plaques, patches, nodules, tumors, wheals, comedos, cysts, vesicles, pustules, or bullae.
Modified lesions are described as secondary skin lesions. These lesions occur as a result of rupture, mechanical irritation, extension, invasion, or normal or abnormal healing of primary lesions. These include atrophy, erosions, ulcers, scales, crusts, excoriation, fissures, lichenification, and scars.
Disorders
Trauma, abnormal cellular function, infection, and systemic disease may cause disruptions in skin integrity. Integumentary disorders include acne; burns; cellulitis; dermatitis; folliculitis, furuncles, and carbuncles; fungal infections; pressure ulcers; psoriasis; scleroderma; toxic epidermal necrolysis; and warts.
ACNE
Acne is a chronic inflammatory disease of the sebaceous glands. It’s usually associated with a high rate of sebum secretion and occurs on areas of the body that have sebaceous glands, such as the face, neck, chest, back, and shoulders.
 Acne occurs in both males and females. Acne vulgaris develops in 80% to 90% of adolescents or young adults, primarily between ages 15 and 18. Although the lesions can appear as early as age 8, acne primarily affects adolescents.
Acne occurs in both males and females. Acne vulgaris develops in 80% to 90% of adolescents or young adults, primarily between ages 15 and 18. Although the lesions can appear as early as age 8, acne primarily affects adolescents.Although the severity and overall incidence of acne is usually greater in males, it tends to start at an earlier age and lasts longer in females.
The prognosis varies and depends on the severity and underlying causes; with treatment, the prognosis is usually good.
Causes
The cause of acne is multifactorial. Diet isn’t believed to be a precipitating factor. Possible causes of acne include increased activity of sebaceous glands and blockage of the pilosebaceous ducts (hair follicles).
Factors that may predispose a patient to acne include:
♦ cobalt irradiation
♦ cosmetics
♦ drugs, including androgens, bromides, corticosteroids, corticotropin (ACTH), halothane, iodides, isoniazid (Laniazid), lithium (Eskalith), phenytoin (Dilantin), striadril (Stri-Vectin SD), and trimethadione
♦ emotional stress
♦ exposure to greases, heavy oils, or tars
♦ heredity
♦ hormonal contraceptive use (Many women experience acne flare-up during their first few menses after starting or discontinuing hormonal contraceptives.)
♦ hormones (A decreased estrogen level or an increased testosterone level can exacerbate acne outbreaks.)
♦ hyperalimentation
♦ trauma or rubbing from tight clothing
♦ tropical climate.
Pathophysiology
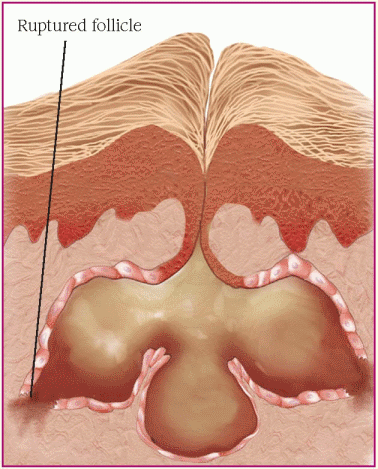
There are two types of acne: inflammatory, in which the hair follicle is blocked by sebum, causing bacteria to grow and eventually rupture the follicle; and noninflammatory, in which the follicle doesn’t rupture but remains dilated. (See Understanding acne, page 560.)
Signs and symptoms
The acne plug may appear as:
♦ a closed comedo, or whitehead (may be protruding from the follicle and covered by the epidermis)
The illustrations below show how acne lesions develop.
1. Excessive sebum production
Androgens stimulate sebaceous gland growth and the production of sebum, which is secreted into dilated hair follicles that contain bacteria.
 |
2. Increased shedding of epithelial cells
The bacteria, usually Propionibacterium acne and Staphylococcus epidermidis, are normal skin flora that secrete the enzyme lipase. This enzyme interacts with sebum to produce free fatty acids, which provoke inflammation.
 |
♦ an open comedo, or blackhead (protruding from the follicle and not covered by the epidermis; melanin or pigment of the follicle causes the black color).
Rupture or leakage of an enlarged plug into the epidermis produces inflammation, characteristic acne pustules, papules or, in severe forms, acne cysts or abscesses (chronic, recurring lesions producing acne scars).
In women, signs and symptoms may include increased severity just before or during menstruation when the estrogen level is at its lowest. Additionally, an increased testosterone level, which occurs in both males and females during puberty, may also trigger an acne outbreak.
Complications
♦ Acne conglobata
♦ Scarring (when acne is severe)
♦ Impaired self-esteem
♦ Abscesses or secondary bacterial infections
Diagnosis
Diagnosis of acne vulgaris is confirmed by characteristic acne lesions, especially in adolescents.
Treatment
Topical treatment for noninflammatory acne includes the application of retinoic acid (tretinoin) on open and closed comedones. For inflammatory acne, an antibacterial such as benzoyl peroxide is effective. Topical and systemic antibiotics and systemic retinoids help reduce the effects of acne.
Systemic therapy consists primarily of:
♦ an antibiotic, usually tetracycline, to decrease bacterial growth (Dosage is reduced for longterm maintenance when the acne in remission.)
♦ oral isotretinoin (Accutane) to inhibit sebaceous gland function and keratinization (A 16- to 20-week course of isotretinoin is limited to patients with severe papulopustular or cystic acne not responding to conventional therapy because of its severe adverse effects. Also, because this drug is known to cause birth defects, the manufacturer, with U.S. Food and Drug Administration approval, recommends the following precautions: pregnancy testing before dispensing; dispensing only a 30-day supply, repeat pregnancy testing throughout the treatment period, effective contraception during treatment, and informed consent. Finally, because of the drug’s effects on the liver, a serum triglyceride level should be drawn before and periodically during treatment.)
♦ for females, estrogens to inhibit androgen activity
♦ other treatments, including intralesional and oral corticosteroids, vitamin A and zinc supplements, exposure to ultraviolet light (although not when the patient is using a photosensitizing agent such as tretinoin), cryotherapy, and surgery.
Special considerations
The main focus of your care is teaching about the disorder, its treatment, and its prevention.
♦ Check the patient’s drug history because certain medications, such as hormonal contraceptives, may cause an acne flare-up.
♦ Try to identify predisposing factors that may be eliminated or modified.
♦ Try to identify eruption patterns (seasonal or monthly).
♦ Explain the causes of acne to the patient and his family. Make sure they understand that the prescribed treatment is more likely to improve acne than a strict diet and fanatical scrubbing with soap and water. Provide written instructions regarding treatment.
♦ Describe the importance of not picking lesions and practicing good personal hygiene to prevent secondary infections.
♦ Instruct the patient receiving tretinoin to apply it at least 30 minutes after washing his face and at least 1 hour before bedtime. Warn against using it around the eyes or lips. After treatments, the skin should look pink and dry. If it appears red or starts to peel, the preparation may have to be weakened or applied less often. Advise the patient to avoid exposure to sunlight or to use a sunscreen. If the prescribed regimen includes tretinoin and benzoyl peroxide, avoid skin irritation by using one preparation in the morning and the other at night.
♦ Instruct the patient to take tetracycline on an empty stomach and not to take it with an antacid or milk because both have metallic ions, and tetracycline interacts with these ions and is then poorly absorbed.
♦ Tell the patient who is taking isotretinoin to avoid vitamin A supplements, which can worsen any adverse reactions. Also, teach the patient how to deal with the dry skin and mucous membranes that usually occur during treatment. Tell the female patient about the severe risk of teratogenicity. Monitor liver enzyme and lipid levels.
♦ Inform the patient that acne takes a long time to clear—even years for complete resolution. Encourage continued local skin care even after
acne clears. Explain the adverse effects of all drugs.
acne clears. Explain the adverse effects of all drugs.
♦ Pay special attention to the patient’s perception of his physical appearance, and offer emotional support.
BURNS
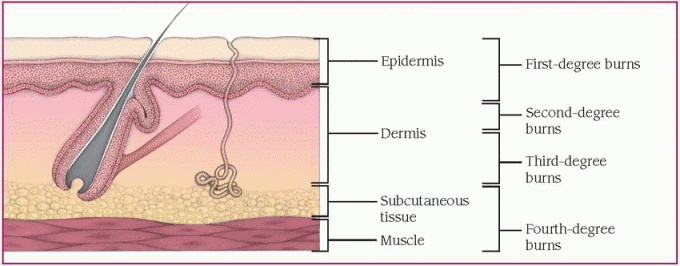
Burns are classified as first-degree, seconddegree superficial, second-degree deep partial thickness, third-degree full thickness, and fourth degree. A first-degree burn is limited to the epidermis. The most common example of a first-degree burn is sunburn, which results from overexposure to the sun. In a second-degree burn, the epidermis and part of the dermis are damaged. A third-degree burn damages the epidermis and dermis, and vessels and tissue are visible. In a fourth-degree burn, the damage extends through deeply charred subcutaneous tissue to muscle and bone. Severe burns require immediate pain management and commonly result in permanent disability, requiring lengthy periods of rehabilitation.
Each year in the United States, about 2.4 million persons receive burn injuries. Most significant burns occur in the home; home fires account for the highest burn fatality rate.
In victims younger than age 4 and older than age 60, there’s a higher incidence of complications and thus a higher mortality rate. Immediate, aggressive burn treatment increases the patient’s chance for survival. Supportive measures and strict sterile technique can minimize infection. Survival and recovery from a major burn are more likely once the burn wound is reduced to less than 20% of the total body surface area (BSA).
Causes
More than 75% of all burn injuries and those that result in death are preventable.
Thermal burns, the most common type, typically result from:
♦ automobile accidents
♦ clothes that have caught on fire
♦ improper handling of firecrackers and gasoline
♦ kitchen and scalding accidents (such as a child climbing on top of a stove or grabbing a hot iron)
♦ parental abuse (of children or elderly people)
♦ playing with matches
♦ residential fires.
Chemical burns result from contact, ingestion, inhalation, or injection of acids, alkalis, or vesicants.
Electrical burns usually result from contact with faulty electrical wiring or high-voltage power lines. Sometimes young children chew electrical cords.
Friction or abrasion burns occur when the skin rubs harshly against a coarse surface.
Sunburn results from excessive exposure to sunlight. Sunlamp use may also result in burns.
Pathophysiology
The injuring agent denatures cellular proteins. Some cells die because of traumatic or ischemic necrosis. Loss of collagen cross-linking also occurs with denaturation, creating abnormal osmotic and hydrostatic pressure gradients, which cause the movement of intravascular fluid into interstitial spaces. Cellular injury triggers the release of mediators of inflammation, contributing to local and, in the case of major burns, systemic increases in capillary permeability. Specific pathophysiologic events depend on the cause and classification of the burn. (See Classifications of burns.)
First-degree burns
A first-degree burn causes localized injury or destruction to the skin (epidermis only) by direct (such as chemical spill) or indirect (such as sunlight) contact. The barrier function of the skin remains intact, and these burns aren’t lifethreatening.
Second-degree superficial partial-thickness burns
Second-degree superficial partial-thickness burns involve destruction of the epidermis and some of dermis. Thin-walled, fluid-filled blisters develop within a few minutes of the injury. As these blisters break, the nerve endings become exposed to the air. Because pain and tactile responses remain intact, subsequent treatments are very painful. The barrier function of the skin is lost.
Second-degree deep partial-thickness burns
Second-degree deep partial-thickness burns involve destruction of the epidermis and dermis, producing blisters and mild to moderate edema and pain. The hair follicles are still intact, so hair will grow again. Compared with seconddegree superficial partial-thickness burns, there’s less pain sensation with this burn because the sensory neurons have undergone extensive destruction. The areas around the burn injury remain very sensitive to pain. The barrier function of the skin is lost.
Third- and fourth-degree full-thickness burns
A major burn affects every body system and organ. A third-degree burn extends through the epidermis and dermis and into the subcutaneous tissue layer. A fourth-degree burn involves muscle, bone, and interstitial tissues. Within only hours, fluids and protein shift from capillary to interstitial spaces, causing edema. There’s an immediate immunologic response to a burn injury, making burn wound sepsis a potential threat. Finally, an increase in calorie demand after a burn injury increases the metabolic rate. (See How burns affect the body, page 564.)
Signs and symptoms
Signs and symptoms depend on the type of burn and may include:
♦ localized pain and erythema, usually without blisters in the first 24 hours, caused by injury from direct or indirect contact with a burn source (first-degree burn)
♦ chills, headache, localized edema, and nausea and vomiting (more severe first-degree burn)
♦ thin-walled, fluid-filled blisters appearing within minutes of the injury, with mild to moderate edema and pain (second-degree superficial partial-thickness burn)
♦ white, waxy appearance to damaged area (second-degree deep partial-thickness burn)
♦ white, brown, or black leathery tissue and visible thrombosed vessels due to destruction of skin elasticity (dorsum of hand most common site of thrombosed veins), without blisters (third-degree burn)
♦ silver-colored, raised area, usually at the site of electrical contact (electrical burn)
♦ singed nasal hairs, mucosal burns, voice changes, coughing, wheezing, soot in mouth or nose, and darkened sputum (with smoke inhalation and pulmonary damage).
Complications
♦ Infection (signs and symptoms including fever, increased pain, redness, swelling, drainage, pus, lymphadenopathy, and red streaks from the burn site)
♦ Dehydration (signs and symptoms including thirst, dry skin, dizziness, headache, lightheadedness, and decreased urine output)
♦ Loss of function (burns to face, hands, feet, and genitalia)
♦ Total occlusion of circulation in extremity (due to edema from circumferential burns)
♦ Airway obstruction (neck burns) or restricted respiratory expansion (chest burns)
♦ Pulmonary injury (from smoke inhalation or pulmonary embolism)
♦ Acute respiratory distress syndrome (due to left-sided heart failure or a myocardial infarction)
♦ Greater damage than indicated by the surface burn (electrical and chemical burns) or internal tissue damage along the conduction pathway (electrical burns)
♦ Cardiac arrhythmias (due to electrical shock and fluid shifts)
Many changes occur as a result of a burn injury, affecting almost every body system. Multidisciplinary care can improve healing and maximize the patient’s return to normal functioning and appearance.
Cardiovascular system
♦ Burns may cause fluid shifts or directly injure the heart and blood vessels, leading to impaired circulation.
♦ The inflammatory response increases capillary permeability. As a result, intravascular fluid shifts to the interstitial spaces, leading to edema, decreased circulating fluid volume, and increased blood viscosity. This hemoconcentration places the patient at risk for thrombus formation.
Respiratory system
♦ Neck burns or swelling from heat and smoke exposure or chemical injury to the mucosa of the respiratory tract can lead to respiratory distress.
♦ Restricted respiratory expansion from chest burns or eschar formation can lead to respiratory distress.
♦ Smoke inhalation or inhalation of other caustic substances results in pulmonary injury, such as bronchitis or respiratory distress.
♦ Hypoxia may result from a decreased amount of oxygen circulating through the blood, which may be caused by inhalation of carbon monoxide, a by-product of combustion that displaces oxygen from hemoglobin molecules.
GI system
♦ As blood is shunted away from the abdominal area and GI tract, peristalsis is slowed or absent altogether.
♦ Gastric dilation and vomiting may occur, possibly increasing the risk of aspiration.
♦ Curling’s ulcers may result (stomach and intestinal ulcerations and hemorrhage).
Integumentary system
♦ Impaired skin integrity increases the risk of infection and causes hypothermia and rapid fluid losses.
♦ Contractures and impaired range-of-motion in extremities may result from hypertrophic scar formation.
♦ Edema associated with circumferential burns constricts underlying blood vessels, tissue, and muscle, impairing circulation to the affected area or extremity.
Immune and hematologic systems
♦ One theory suggests that burn cells release a toxin that interferes with the immune system’s ability to function properly. Subsequently, major burns may result in immunosuppression.
♦ Generalized sepsis is a common and serious complication—the larger the wound, the greater the risk of infection.
♦ More severe burn states may result in the development of disseminated intravascular coagulation.
Renal system
♦ Hemoconcentration and decreased intravascular volumes cause decreased renal perfusion and decreased urine output.
♦ Prolonged decreased renal perfusion leads to acute tubular necrosis and renal failure.
Collaborative management
If the burn involves a large surface area or critical body parts, it usually requires treatment at a specialized burn center. Surgeons may be needed to perform escharotomy and fasciotomy to remove burn tissue. Wound care specialists may be needed to prevent wound infections and complications and promote wound healing. Respiratory therapy is needed to maximize respiratory function in cases of inhalation injury.
As the patient improves, physical therapy is necessary to maintain or improve range-ofmotion and prevent contractures. Nutritional therapists can prescribe an optimal diet to promote wound healing. Referral to a therapist and a support group may help the patient deal with psychological effects of the traumatic injury. Similar referrals are needed if severe scarring or disfigurement is anticipated.
♦ Hypotension, secondary to shock or hypovolemia
♦ Stroke, heart attack, or pulmonary embolism (due to formation of blood clots resulting from slower blood flow)
♦ Burn shock (due to fluid shifts out of the vascular compartments, possibly leading to kidney damage and renal failure)
♦ Peptic ulcer disease or ileus (due to decreased blood supply in the abdominal area)
♦ Disseminated intravascular coagulation (more severe burn states)
♦ Added pain, depression, and financial burden (due to psychological component of disfigurement)
Diagnosis
Diagnosis involves determining the size and classifying the wound. The following methods are used to determine size:
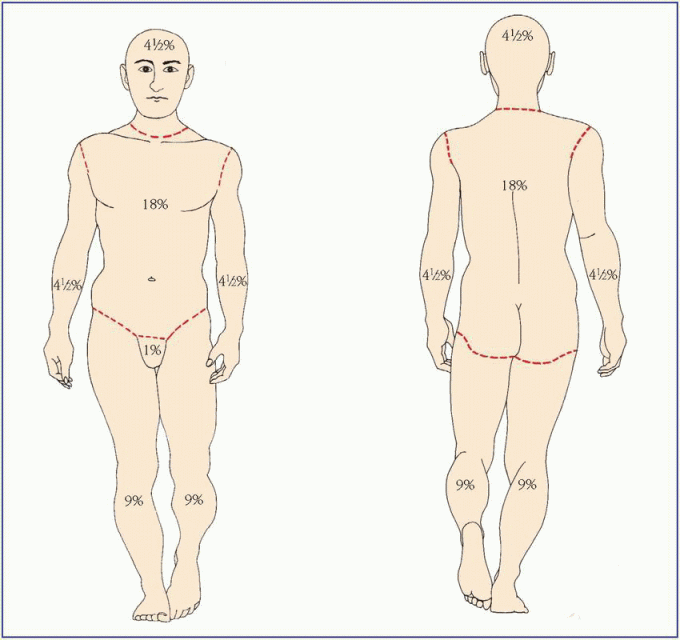
♦ percentage of BSA covered by the burn using the rule of nines chart
♦ Lund-Browder chart (more accurate because it allows BSA changes with age); correlation of the burn’s depth and size to estimate its severity. (See Using the Rule of Nines and the Lund-Browder chart, pages 566 and 567.)
Major burns are classified as:
♦ third-degree burns over more than 10% of BSA
♦ second-degree burns over more than 25% of adult BSA (over 20% in children)
♦ burns of hands, face, feet, or genitalia
♦ burns complicated by fractures or respiratory damage
♦ electrical burns
♦ all burns in poor-risk patients. Moderate burns are classified as:
♦ third-degree burns over 2% to 10% of BSA
♦ second-degree burns over 15% to 25% of adult BSA (10% to 20% in children). Minor burns are classified as:
♦ third-degree burns over less than 2% of BSA
♦ second-degree burns over less than 15% of adult BSA (10% in children).
Treatment
Initial burn treatments are based on the type of burn and may include:
♦ immersing the burned area in cool water (55°F [12.8°C]) or applying cool compresses (minor burns)
♦ administering pain medication, as needed, or an anti-inflammatory
♦ covering the area with an antimicrobial and a nonstick bulky dressing (after debridement); prophylactic tetanus injection as needed
♦ not disturbing blisters or dead skin (increases risk of infection)
♦ preventing hypoxia by maintaining an open airway; assessing airway, breathing, and circulation; checking for smoke inhalation immediately when the patient presents; assisting with endotracheal intubation; and giving 100% oxygen (first immediate treatment for moderate and major burns)
♦ controlling active bleeding
♦ covering partial-thickness burns over 30% of BSA or full-thickness burns over 5% of BSA with a clean, dry, sterile bedsheet (because of drastic reduction in body temperature, don’t cover large burns with saline-soaked dressings)
♦ removing smoldering clothing (first soaking the clothing in saline solution if it’s stuck to the patient’s skin), rings, and other constricting items
♦ immediate I.V. therapy to prevent hypovolemic shock and maintain cardiac output (lactated Ringer’s solution or a fluid replacement formula; additional I.V. lines may be needed)
♦ antimicrobial therapy (all patients with major burns)
♦ correction of electrolyte imbalances, transfusion and replacement blood products as indicated by laboratory results, and dialysis for renal failure or myoglobinuria
♦ closely monitoring intake and output, frequently checking vital signs (every 15 minutes), possibly inserting an indwelling urinary catheter
♦ nasogastric tube to decompress the stomach and avoid aspiration of stomach contents
♦ irrigating the wound with copious amounts of normal saline solution (chemical burns)
♦ surgical intervention, including skin grafts and more thorough surgical cleaning (major burns).
Special considerations
♦ Don’t treat the burn wound for a patient being transferred to a specialty facility within 4 hours. Maintain airway, breathing, and circulation. Wrap the patient in a sterile sheet and blanket for warmth, elevate the burned extremity, and prepare the patient for transport. Upon discharge or during prolonged care:
♦ Ensure increased caloric intake due to increased metabolic rate to promote healing and recovery.
♦ Give the patient complete discharge instructions, teaching him what he needs to know about home care; stress the importance of keeping the dressing clean and dry, elevating the burned extremity for the first 24 hours, and having the wound rechecked in 1 to 2 days. Also
stress the importance of taking pain medication as needed, especially before dressing changes.
stress the importance of taking pain medication as needed, especially before dressing changes.
Using the Rule of Nines and the Lund-Browder chart
You can quickly estimate the extent of an adult patient’s burn by using the Rule of Nines. This method divides an adult’s body surface area (BSA) into percentages. To use this method, mentally transfer your patient’s burns to the body chart shown below, then add up the corresponding percentages for each burned body section. The total, an estimate of the extent of your patient’s burns, enters into the formula to determine his initial fluid replacement needs.
You can’t use the Rule of Nines for infants and children because their body section percentages differ from those of adults. For example, an infant’s head accounts for about 17% at the total BSA compared with 7% for an adult. Instead, use the Lund-Browder chart.
 |
CELLULITIS
Cellulitis is an infection of the dermis or subcutaneous layer of the skin. It may follow damage to the skin, such as a bite or wound. As the cellulitis spreads, fever, erythema, and lymphangitis may occur.
If treated in a timely manner, the prognosis is usually good. Persons with other contributing health factors, such as diabetes, immunodeficiency, impaired circulation, or neuropathy, have an increased risk of developing or spreading cellulitis.
Causes
Possible causes of cellulitis are bacterial and fungal infections, commonly group A streptococcus and Staphylococcus aureus.
Pathophysiology
As the offending organism invades the compromised area, it overwhelms the defensive cells
(neutrophils, eosinophils, basophils, and mast cells) that break down the cellular components, which normally contain and localize the inflammation. As cellulitis progresses, the organism invades tissue around the initial wound site.
(neutrophils, eosinophils, basophils, and mast cells) that break down the cellular components, which normally contain and localize the inflammation. As cellulitis progresses, the organism invades tissue around the initial wound site.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree