Infection
The 20th century encompassed astonishing advances in treating and preventing infection, such as potent antibiotics, complex immunizations, and modern sanitation, yet infection remains the most common cause of human disease. Even in countries with advanced medical care, infectious disease remains a major cause of serious illness. In developing countries, infection is one of the most critical health problems.
Understanding infection
Infection is the invasion and multiplication of microorganisms in or on body tissue that produce signs and symptoms as well as an immune response. Such reproduction injures the host by causing cell damage from microorganismproduced toxins or from intracellular multiplication, or by competing with host metabolism. Infectious diseases range from relatively mild illnesses to debilitating and lethal conditions: from the common cold through chronic hepatitis to acquired immunodeficiency syndrome. The severity of the infection varies with the pathogenicity and number of the invading microorganisms and the strength of host defenses. The very young and the very old are especially susceptible.
For infection to be transmitted, these factors must be present: causative agent, infectious reservoir with a portal of exit, mode of transmission, a portal of entry into the host, and a susceptible host.
RISK FACTORS
A healthy person can usually ward off infections with the body’s own built-in defense mechanisms that include:
♦ intact skin
♦ normal flora that inhabit the skin and various organs (see How microbes interact with the body)
♦ lysozymes (enzymes that can kill microorganisms or microbes) secreted by eyes, nasal passages, glands, stomach, and genitourinary organs
♦ defensive structures, such as the cilia, that sweep foreign matter from the airways
♦ a healthy immune system.
However, if an imbalance develops, the potential for infection increases. Risk factors for the development of infection include weakened defense mechanisms, environmental and developmental factors, and pathogen characteristics.
WEAKENED DEFENSE MECHANISMS
The body has many defense mechanisms for resisting entry and multiplication of microbes. However, a weakened immune system makes it easier for these pathogens to invade the body and launch an infectious disease. This weakened state is referred to as immunodeficiency or immunocompromise.
Impaired function of white blood cells (WBCs) and low levels of T and B cells characterize immunodeficiencies. An immunodeficiency may be congenital (caused by a genetic defect and present at birth) or acquired (developed after birth). Acquired immunodeficiency may result from infection, malnutrition, chronic stress, or pregnancy. Diabetes, renal failure, and cirrhosis can suppress
the immune response, as can corticosteroids and chemotherapeutic drugs.
the immune response, as can corticosteroids and chemotherapeutic drugs.
Regardless of cause, the result of immunodeficiency is the same. The body’s ability to recognize and fight pathogens is impaired. People who are immunodeficient are more susceptible to all infections, are more acutely ill when they become infected, and require a much longer time to heal.
ENVIRONMENTAL FACTORS
Other conditions that may weaken a person’s immune defenses include poor hygiene, malnutrition, inadequate physical barriers, emotional and physical stressors, chronic diseases, medical and surgical treatments, and inadequate immunization.
Good hygiene promotes normal host defenses; poor hygiene increases the risk of infection. Unclean skin harbors microbes and offers an environment for them to colonize, and untended skin is more likely to allow invasion. Frequent washing removes surface microbes and maintains an intact barrier to infection, but it may damage the skin. To maintain skin integrity, lubricants and emollients may be used to prevent cracks and breaks.
The body needs a balanced diet to provide the nutrients, vitamins, and minerals that an effective immune system needs. Protein malnutrition inhibits the production of antibodies, without which the body can’t mount an effective attack against microbe invasion. Malnutrition is directly related to incidence of nosocomial infections. Along with a balanced diet, the body needs adequate vitamins and minerals to use ingested nutrients.
Dust can facilitate transportation of pathogens. For example, dust-borne spores of the fungus Aspergillus transmit the infection. If the inhaled spores become established in the lungs, they’re notoriously difficult to expel. Fortunately, persons with intact immune systems can usually resist infection with Aspergillus, which is usually dangerous only in the presence of severe immunosuppression.
DEVELOPMENTAL FACTORS
The very young and very old are at higher risk for infection. The immune system doesn’t fully develop until about age 6 months. An infant exposed to an infectious agent usually develops an infection. The most common type of infection in toddlers affects the respiratory tract. When young children put toys and other objects in their mouths, they increase their exposure to various pathogens.
Exposure to communicable diseases continues throughout childhood, as children progress from day-care facilities to schools. Skin diseases, such as impetigo and lice infestation, commonly pass from one child to the next at this age. Accidents are common in childhood as well, and broken or abraded skin opens the way for bacterial invasion. Lack of immunization also contributes to incidence of childhood diseases.
How microbes interact with the body
Microbes interact with their host in various ways.
Double benefit
Some of the microorganisms of the normal human flora interact with the body in ways that mutually benefit both parties. Escherichia coli organisms, part of the normal intestinal flora, obtain nutrients from the human host; in return, they secrete vitamin K, which the human body needs for blood clotting.
Single benefit
Other microbes of the normal flora have a commensal interaction with the human body—an interaction that benefits one party (in this case, the microbes) without affecting the other.
Parasitic interaction
Some pathogenic microbes, such as helminths (worms), are parasites, meaning that they harm the host while they benefit from their interaction with it.
Advancing age, on the other hand, is associated with a declining immune system, partly as a result of decreasing thymus function. Chronic diseases, such as diabetes and atherosclerosis, can weaken defenses by impairing blood flow and nutrient delivery to body systems.
PATHOGEN CHARACTERISTICS
A microbe must be present in sufficient quantities to cause a disease in a healthy human. The number needed to cause a disease varies from one microbe to the next and from host to host, and may be affected by the mode of transmission. The severity of an infection depends on several factors, including the microbe’s pathogenicity— that is, the likelihood that it will cause pathogenic changes or disease. Factors that affect pathogenicity include the microbe’s specificity, invasiveness, quantity, virulence, toxigenicity, adhesiveness, antigenicity, and viability. (See Chain of infection, pages 48 and 49.)
Chain of infection
An infection can occur only if the six components depicted below are present. Removing one link in the chain prevents infection.
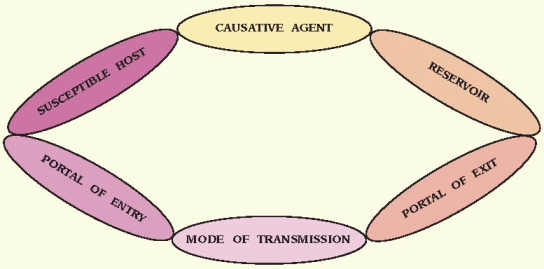 |
Causative agent
A causative agent for infection is any microbe that can produce disease.
Reservoir
The reservoir is the environment or object in or on which a microbe can survive and, in some cases, multiply. Inanimate objects, human beings, and other animals can all serve as reservoirs, providing the essential requirements for a microbe to survive at specific stages in its life cycle.
Portal of exit
The portal of exit is the path by which an infectious agent leaves its reservoir. Usually, this portal is the site where the organism grows. Common portals of exit associated with human reservoirs include the respiratory, genitourinary, and GI tracts; the skin and mucous membranes; and the placenta (in transplacental disease transmission from mother to fetus). Blood, sputum, vomitus, stool, urine, wound drainage, and genital secretions also serve as portals of exit. The portal of exit varies from one infectious agent to the next.
Mode of transmission
The mode of transmission is the means by which the infectious agent passes from the portal of exit in the reservoir to the susceptible host. Infections can be transmitted through one of four modes: contact, airborne, enteric, and vector-borne. Some organisms use more than one mode of transmission to get from the reservoir to a new host. As with portals of exit, the mode of transmission varies with the specific microbe.
Contact transmission is subdivided into direct contact, indirect contact, and droplet spread (contact with droplets that enter the environment).
Direct contact refers to person-to-person spread of organisms through physical contact.
Indirect contact occurs when a susceptible person comes in contact with a contaminated object.
Droplet transmission results from contact with contaminated respiratory secretions. It differs from airborne transmission in that the droplets don’t remain suspended in the air but settle on surfaces.
Airborne transmission occurs when fine microbial particles containing pathogens remain suspended in the air for a prolonged period, and then are spread widely by air currents and inhaled.
Enteric (oral-fecal) transmission occurs when infecting organisms found in stool are ingested by susceptible victims, in many cases, through fecally contaminated food or water.
Vector-borne transmission occurs when an intermediate carrier, or vector, such as a flea or a mosquito, transfers a microbe to another living organism. This type of transmission is of most concern in tropical areas, where insects commonly transmit disease.
Portal of entry
Portal of entry refers to the path by which an infectious agent invades a susceptible host. Usually, this path is the same as the portal of exit.
Susceptible host
A susceptible host is also required for the transmission of infection to occur. The human body has many defense mechanisms for resisting the entry and multiplication of pathogens. When these mechanisms function normally, infection doesn’t occur. However, in a weakened host, an infectious agent is more likely to invade the body and launch an infectious disease.
♦ Specificity is the range of hosts to which a microbe is attracted. Some microbes may be attracted to a wide range of humans and animals, whereas others select only human or only animal hosts.
♦ Invasiveness (sometimes called infectivity) is a microbe’s ability to invade and multiply in the host tissues. Some microbes can enter through intact skin; others can enter only if the skin or mucous membrane is broken. Some microbes produce enzymes that enhance their invasiveness.
♦ Quantity refers to the number of microbes that succeed in invading and reproducing in the body.
♦ Virulence is the severity of the disease a pathogen can produce. Virulence can vary depending on the host defenses; any infection can be life-threatening in an immunodeficient patient. Infection with a pathogen known to be particularly virulent requires early diagnosis and treatment.
♦ Toxigenicity is related to virulence. It describes a pathogen’s potential to damage host tissues by producing and releasing toxins.
♦ Adhesiveness is the ability of the pathogen to attach to host tissue. Some pathogens secrete a sticky substance that helps them adhere to tissue
while protecting them from the host’s defense mechanisms.
while protecting them from the host’s defense mechanisms.
♦ Antigenicity is the degree to which a pathogen can induce a specific immune response. Microbes that invade and localize in tissue initially stimulate a cellular response; those that disseminate quickly throughout the host’s body generate an antibody response.
♦ Viability is the ability of a pathogen to survive outside its host. Most microbes can’t live and multiply outside a reservoir.
Stages of infection
Development of an infection usually proceeds through four stages. The first stage, incubation, may be almost instantaneous or last for years. During this time, the pathogen is replicating, and the infected person is contagious and can transmit the disease. The prodromal stage (stage two) follows incubation, and the still-contagious host makes vague complaints of feeling unwell. In stage three, acute illness, microbes are actively destroying host cells and affecting specific host systems. The patient recognizes which area of the body is affected and voices complaints that are more specific. Finally, the convalescent stage (stage four) begins when the body’s defense mechanisms have confined the microbes and healing of damaged tissue is progressing.
Infection-causing microbes
Microorganisms that are responsible for infectious diseases include bacteria, viruses, fungi, parasites, mycoplasmas, rickettsia, and chlamydiae.
BACTERIA
Bacteria are simple one-celled microorganisms with a cell wall that protects them from many of the human body’s defense mechanisms. Although they lack a nucleus, bacteria possess all the other mechanisms they need to survive and rapidly reproduce.
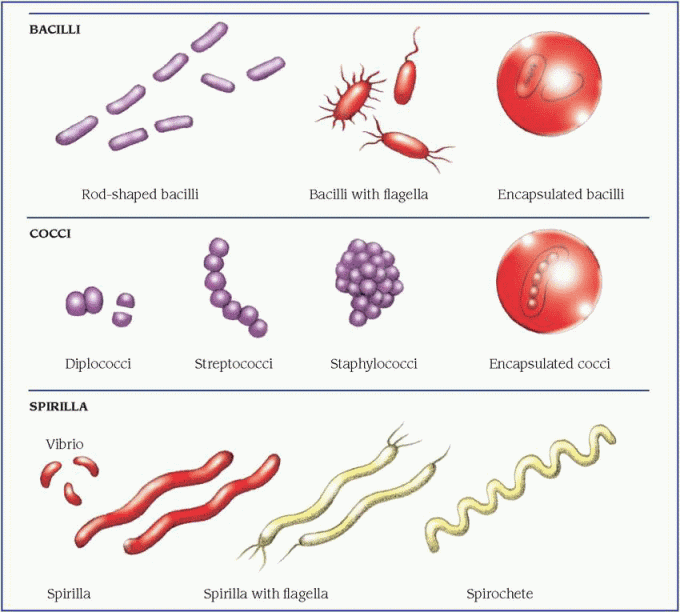
Bacteria can be classified according to shape—rod shaped bacilli, spherical cocci, and spiral-shaped spirilla. (See Comparing bacterial shapes, page 50.) Bacteria can also be classified according to their need for oxygen (aerobic or anaerobic), their mobility (motile or nonmotile), and their tendency to form protective capsules (encapsulated or nonencapsulated) or spores (sporulating or nonsporulating).
Bacteria damage body tissues by interfering with essential cell function or by releasing exotoxins or endotoxins, which cause cell damage. (See How bacteria damage tissue, page 51.) During bacterial growth, the cells release exotoxins, enzymes that damage the host cell, altering its function or killing it. Enterotoxins are a specific type of exotoxin secreted by bacteria that infect the GI tract; they affect the vomiting center of the brain and cause gastroenteritis. Exotoxins also can cause diffuse reactions in the host, such as inflammation, bleeding, clotting, and fever. Endotoxins are contained in the cell walls of gram-negative bacteria, and they’re released during lysis of the bacteria.
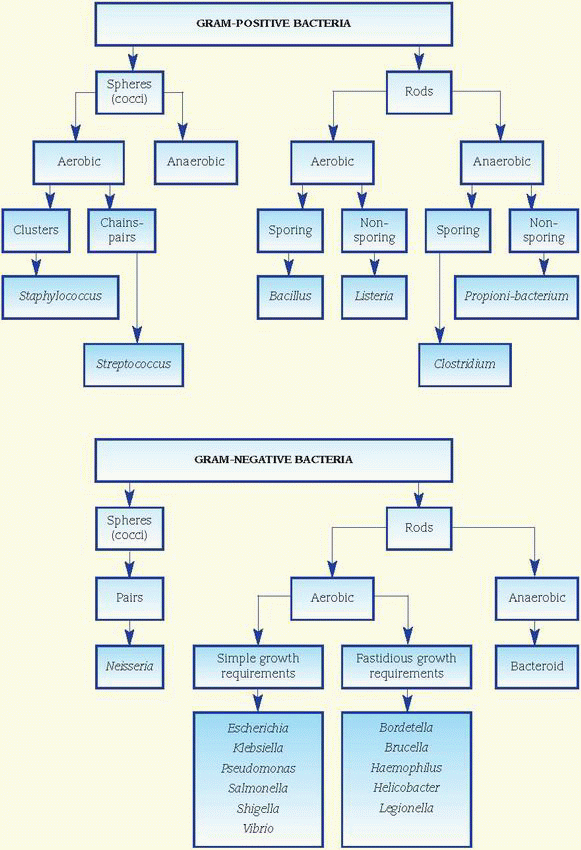
Examples of bacterial infection include staphylococcal wound infection, cholera, and streptococcal pneumonia. (See Gram-positive and gram-negative bacteria, page 52.)
VIRUSES
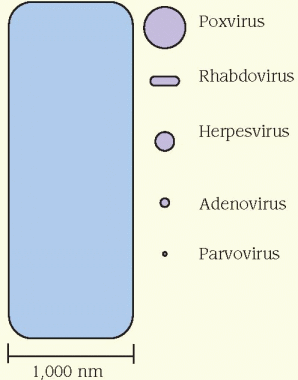
Viruses are subcellular organisms made up of only a ribonucleic acid (RNA) nucleus or a deoxyribonucleic acid (DNA) nucleus covered with proteins. They’re the smallest known organisms, so tiny that only an electron microscope can make them visible. (See How viruses size up, page 53.) Independent of the host cells, viruses can’t replicate. Rather, they invade a host cell and stimulate it to participate in forming additional virus particles. Some viruses destroy surrounding tissue and release toxins. (See Viral infection of a host cell, page 53.) Viruses lack the genes necessary for energy production. They depend on the ribosomes and nutrients of infected host cells for protein production. The estimated 400 viruses that infect humans are classified according to their size, shape, and means of transmission (respiratory, fecal, oral, sexual).
Most viruses enter the body through the respiratory, GI, and genital tracts. A few, such as human immunodeficiency virus (HIV), are transmitted through blood, broken skin, and mucous membranes. Viruses can produce a wide variety of illnesses, including the common cold, herpes simplex, herpes zoster, chickenpox, infectious mononucleosis, hepatitis B and C, and rubella. Signs and symptoms depend on the host cell’s status, the specific virus, and whether the intracellular environment provides good living conditions for the virus.
Retroviruses are a unique type of virus that carry their genetic code in RNA rather than in the more common carrier, DNA. These RNA viruses contain the enzyme reverse transcriptase,
which changes viral RNA into DNA. The host cell then incorporates the alien DNA into its own genetic material. The most notorious retrovirus today is HIV.
which changes viral RNA into DNA. The host cell then incorporates the alien DNA into its own genetic material. The most notorious retrovirus today is HIV.
Bacteria and other infectious organisms constantly infect the human body. Some, such as the intestinal bacteria that produce vitamins, are beneficial. Others are harmful, causing illnesses ranging from the common cold to life-threatening septic shock.
To infect a host, bacteria must first enter it. They do this by adhering to the mucosal surface and directly invading the host cell or by attaching to epithelial cells and producing toxins, which invade host cells. To survive and multiply within a host, bacteria or their toxins adversely affect biochemical reactions in cells. The result is a disruption of normal cell function or cell death (see illustration below). For example, the diphtheria toxin damages heart muscle by inhibiting protein synthesis. In addition, as some organisms multiply, they extend into deeper tissue and eventually gain access to the bloodstream.
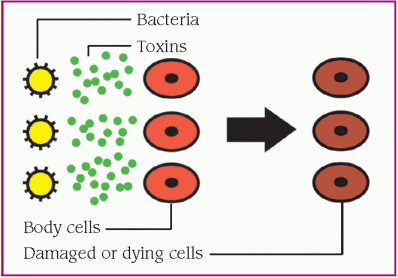 |
Some toxins cause blood to clot in small blood vessels. The tissues supplied by these vessels may be deprived of blood and damaged (see illustration below).
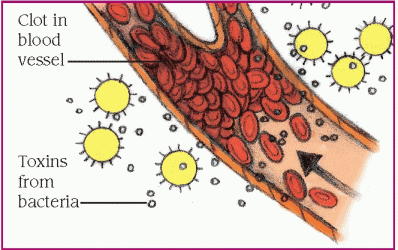 |
Other toxins can damage the cell walls of small blood vessels, causing leakage. This fluid loss results in decreased blood pressure, which in turn impairs the heart’s ability to pump enough blood to vital organs (see illustration below).
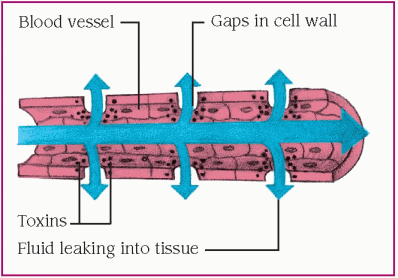 |
FUNGI
Fungi have rigid walls and nuclei that are enveloped by nuclear membranes. They occur as yeast (single-cell, oval-shaped organisms) or molds (organisms with hyphae, or branching filaments). Depending on the environment, some fungi may occur in both forms. Found almost everywhere on earth, fungi live on organic matter, in water and soil, on animals and plants, and on a wide variety of unlikely materials. They can live inside and outside their host. Superficial fungal infections cause athlete’s foot and vaginal infections. Candida albicans is part of the body’s normal flora but under certain circumstances it can cause yeast infections of virtually any part of the body but especially the mouth, skin, vagina, and GI tract. For example, antibiotic treatment or a change in the pH of the susceptible tissues (because of a disease such as diabetes, or use of certain drugs, such as hormonal contraceptives) can wipe out the normal bacteria that keep the yeast population in check.
PARASITES
Parasites are unicellular or multicellular organisms that live on or within another organism and obtain nourishment from the host. They take only the nutrients they need and usually don’t kill their hosts. Examples of parasites that
can produce an infection if they cause cellular damage to the host include helminths, such as pinworms and tapeworms, and arthropods, such as mites, fleas, and ticks. Helminths can infect the human gut; arthropods commonly cause skin and systemic disease.
can produce an infection if they cause cellular damage to the host include helminths, such as pinworms and tapeworms, and arthropods, such as mites, fleas, and ticks. Helminths can infect the human gut; arthropods commonly cause skin and systemic disease.
The virion (A) attaches to receptors on the host-cell membrane and releases enzymes (called absorption) (B) that weaken the membrane and enable the virion to penetrate the cell. The virion removes the protein coat that protects its genetic material (C), replicates (D), and matures, and then escapes from the cell by budding from the plasma membrane (E). The infection can then spread to other host cells.
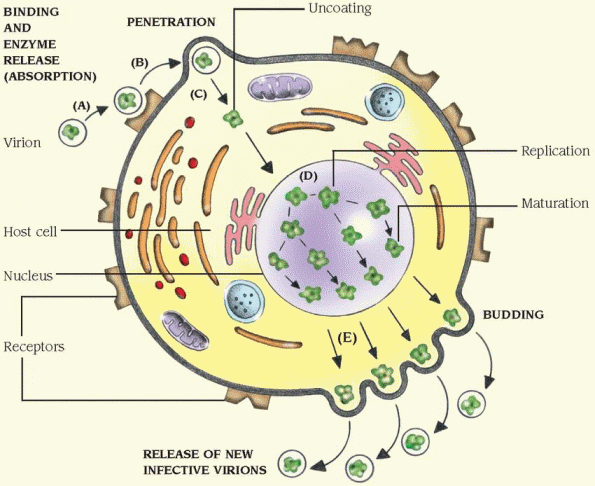 |
MYCOPLASMAS
Mycoplasmas are bacteria-like organisms, the smallest of the cellular microbes that can live outside a host cell, although some may be parasitic. Lacking cell walls, they can assume many different shapes ranging from coccoid to filamentous. The lack of a cell wall makes them resistant to penicillin and other antibiotics that work by inhibiting cell wall synthesis. Mycoplasmas can cause primary atypical pneumonia and many secondary infections.
RICKETTSIA
Rickettsia are small, gram-negative, bacteria-like organisms that can cause life-threatening illness. They may be coccoid, rod-shaped, or irregularly shaped. Because they’re live viruses, rickettsia require a host cell for replication. They have no cell wall, and their cell membranes are leaky; thus, they must live inside another, better protected cell. Rickettsia are transmitted by the bites of arthropod carriers, such as lice, fleas, and ticks, and through exposure to their waste products. Rickettsial infections that occur in the United States include Rocky Mountain spotted fever, typhus, and Q fever.
CHLAMYDIAE
Chlamydiae are smaller than rickettsia and bacteria but larger than viruses. They depend on host cells for replication and are susceptible to antibiotics. Chlamydiae are transmitted by direct contact, such as that which occurs during sexual activity. They’re a common cause of infections of the urethra, bladder, fallopian tubes, and prostate gland.
Pathophysiologic changes
Clinical expressions of infectious disease vary, depending on the pathogen involved and the organ system affected. Most of the signs and symptoms result from host responses, which may be similar or very different from host to host. During the prodromal stage, a person will complain of common, nonspecific signs and symptoms, such as fever, muscle aches, headache, and lethargy. In the acute stage, signs and symptoms that are more specific provide evidence of the microbe’s target. However, some illnesses remain asymptomatic and are discovered only by laboratory tests.
INFLAMMATION
The inflammatory response is a major reactive defense mechanism in the battle against infective agents. Inflammation may be the result of tissue injury, infection, or allergic reaction. Acute inflammation has two stages: vascular and cellular. In the vascular stage, arterioles at or near the injury’s site briefly constrict and then dilate, causing fluid pressure to increase in the capillaries. The consequent movement of plasma into the interstitial space causes edema. At the same time, inflammatory cells release histamine and bradykinin, which further increase capillary permeability. Red blood cells and fluid flow into the interstitial space, contributing to edema. The extra fluid arriving in the inflamed area dilutes microbial toxins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree