Infectious Mononucleosis Syndromes
Carla S. Wilson, MD, PhD
Key Facts
Terminology
IM is an acute illness
Mainly due to EBV infection
˜ 20% of cases due to CMV or other viral infection
Clinical Issues
EBV: Clinical triad of sore throat, fever, and lymphadenopathy
CMV: Persistent fever often predominates
Pharyngitis and tonsillitis are rare
Microscopic Pathology
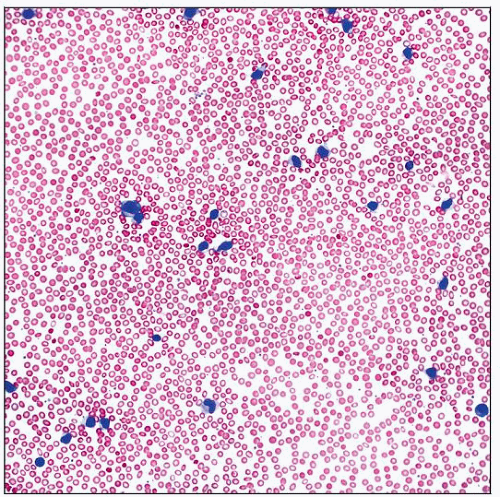
Hallmark is peripheral blood findings
Lymphocytes and monocytes are > 50% of leukocytes
> 10% are atypical lymphocytes
Marked lymphocyte heterogeneity
EBV infection
Downey type II and III cells common
Autoimmune hemolytic anemia, primarily anti-i antibodies
CMV infection
Circulating infected endothelial cells in immunosuppressed individuals are diagnostic
Bone marrow evaluation usually not required
Nonspecific reactive changes: Lymphocytosis, plasmacytosis, granulomatous infiltrates
Transient bone marrow suppression
CMV-infected cells may appear normal or have “owl’s eye” viral inclusions
Ancillary Tests
Immunohistochemistry or in situ hybridization for EBV or CMV are confirmatory
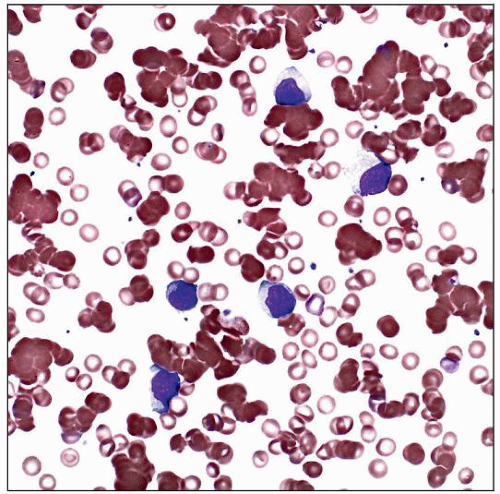
 A prominent lymphocytic reaction is present in this peripheral blood smear from a 16-year-old female with infectious mononucleosis and EBV-positive serology. |
TERMINOLOGY
Abbreviations
Infectious mononucleosis (IM)
Definitions
IM is an acute illness
Caused by primary viral infection
80-90% Epstein-Barr virus (EBV)
7-10% cytomegalovirus (CMV)
Other viruses
ETIOLOGY/PATHOGENESIS
Herpesvirus Family
Double-stranded DNA viruses
Envelope derived from host cell membrane
Symptomatic disease associated with lytic virus replication
Latent infection after recovery from acute infection
EBV
Gamma-1 herpes virus
Infects B cells
Receptors are CD21, MHC class II
Majority of infected B cells are rapidly cleared from circulation in immunocompetent individuals
Elicits T-cell and early natural killer (NK) cell response
Latency established in lymphoid cells or fibroblasts
EBV genome circularizes in nucleus of B lymphocytes and is replicated as an episome
Memory B cells remain quiescently infected and serve as reservoir for lifelong infection
CMV
Beta herpes virus
Infects epithelial cells, endothelial cells, neuronal cells, smooth muscle cells, fibroblasts, monocytes, macrophages, and T cells
Infects cells by endocytosis
Does not infect B cells
Cell-mediated immunity plays primary role in controlling infection
Individuals may develop primary or secondary infection
Primary infection occurs in seronegative individuals who were never previously infected
Secondary infection is activation of previously latent infection or reinfection by different CMV strain
CLINICAL ISSUES
Epidemiology
Incidence
Clinically apparent IM
More common in populations with delayed primary EBV or CMV exposure
EBV-associated IM: 45.2 cases per 100,000 people per year in USA
May have primary EBV/CMV coinfection or mixed infection with other organism
Clinically silent infection
Usually infants or children
Frequently negative for heterophile antibody
CMV infection in immunosuppressed individuals
Most common viral opportunistic infection in AIDS; often multiple CMV strains
Reactivation of virus common in stem cell or solid organ transplant patients
Infection occurs 1-3 months after transplant if no prophylaxis, 4-8 months if failed prophylaxis treatment
CMV viremia seen in 30% of at-risk pediatric lung transplant patients
Age
Older age suggests CMV rather than EBV infection
EBV-associated IM is most prevalent in 15-24 year olds in the United States
CMV-associated IM usually affects 20-30 year olds; age range is 18-66 years
Age has significant impact on clinical expression
In young children, EBV is often asymptomatic or expressed as rashes, neutropenia, or pneumonia
Primary CMV in pregnant women may lead to congenital infection of neonate
Ethnicity
EBV-associated IM is 30x more frequent in whites than blacks
Presentation
EBV and CMV are spread through intimate contact
Often by asymptomatic shedders of virus to susceptible individuals
Spread through kissing, sharing of food, other intimate contact
Transmitted by blood transfusions and open heart surgery
Risk increases with increased volume of blood transfused
CMV also transmitted with leukocyte transfusions
Risk reduced when blood is screened for antibodies or with use of leukocyte-filtered/-reduced products
Symptoms of IM
EBV
Triad of sore throat, fever, lymphadenopathy
Symmetrical, slightly tender lymphadenopathy, especially posterior cervical region in adolescents
Hepatosplenomegaly, jaundice, rash
Malaise, headache, myalgias, chills, nausea
Studies suggest incubation period of 30-50 days
CMV
Systemic symptoms (typhoidal)
Persistent fever may predominate (average duration ~ 19 days)
Pharyngitis and tonsillitis are rare
Often mild asymptomatic hepatitis
Lymphadenopathy or splenomegaly is uncommon but may occur
Interstitial pneumonia is a rare complication, especially in stem cell recipients
Laboratory Tests
CBC and peripheral blood smear
Peripheral blood smear findings often precede heterophile antibody positivity in EBV infection
Morphologic findings help in making diagnosis
Confirmation of EBV infection is required in heterophile negative cases
Diagnosis of CMV infection requires laboratory confirmation
Heterophile antibody (monospot) test
Positive
Majority of EBV-associated IM
90% of adolescents, 80% of children > 4 years of age
EBV-specific serology unnecessary to make diagnosis
Occasional patients with lymphoma or hepatitis are positive
Negative
50% of young children with symptomatic EBV infection
EBV-specific antibody test by indirect immunofluorescence
Acute EBV infection
Elevated IgM antibody to anti-viral capsid antigens (VCAs) detected in 80% of children > 4 years
Anti-early antigens (anti-EAs)
Antibody to EBV nuclear antigen (EBNA) 3-4 weeks after onset
EBV viral load
EBV DNA quantitated with real-time PCR
Not usually necessary for diagnosis of IM
Helpful for evaluation of other EBV-associated diseases
CMV testing
CMV pp65 antigenemia assay
Detects CMV-infected leukocytes in blood
Results generally available within 24 hours
Molecular tests for active infection
Quantitative PCR for viral load
Hybridization capture assay using RNA probes for CMV DNA
Shell viral cultures using monoclonal probes to early antigens
Liver function tests
Abnormal in almost all cases
Maximum elevation in 2nd week of illness
Immunologic findings possible with EBV or CMV
Cryoproteins or cold agglutinins
Slightly increased in 90-95% of patients with EBV infection
Rheumatoid factor
Antinuclear antibodies
Anti-complement antibodies
Natural History
Most patients with IM recover without complications
EBV IM spontaneously resolves in 2-3 weeks
Complications of EBV
Autoimmune hemolytic anemia (< 3% of patients)
IgM-type cold agglutinin
Anti-i specificity in 20-70% of cases
Splenic rupture
Death
Rare; secondary to neurologic complications, splenic rupture, upper airway obstruction
CMV infection in immunocompetent individuals
Infection is usually self-limiting with low mortality
CMV infection in immunosuppressed individuals
Development of CMV pneumonia after transplantation or chemotherapy; may be life-threatening
Complications of secondary CMV infection
Interstitial pneumonitis, hepatitis, Guillain-Barré syndrome, encephalitis, retinitis
Gastrointestinal infections, pericarditis, myocarditis, myeloradiculopathy
Treatment
Supportive therapy is sufficient in most cases
Corticosteroids for EBV-associated complications
Tonsillar enlargement with compromised airway
Autoimmune hemolytic anemia
Aplastic anemia
Antiviral therapy for CMV in immunocompromised patients
Ganciclovir, foscarnet, cidofovir
MICROSCOPIC PATHOLOGY
EBV-Associated Peripheral Blood Findings
Mild to moderate leukocytosis (10-20 × 109/L)
Lymphocytosis ~ 1 week after initiation of symptoms
Peaks at 2-3 weeks
Persists up to 8 weeks
Atypical lymphocytes with marked heterogeneity
Most common type is Downey type II cells
Next most common type is Downey type III cells
Frequently, cells intermediate between Downey type II and III cells are seen
Downey type I cells are most common in young children with EBV and other reactive causes
Plasma cells are infrequent
Mild thrombocytopenia (< 150 × 109/L)
1/3-1/2 of cases
Autoimmune hemolytic anemia
Autoantibodies present (primarily anti-i)
Spherocytes and polychromasia
Red blood cell clumping
Cold agglutinin
Neutropenia is rare
Usually mild and self-limiting
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree