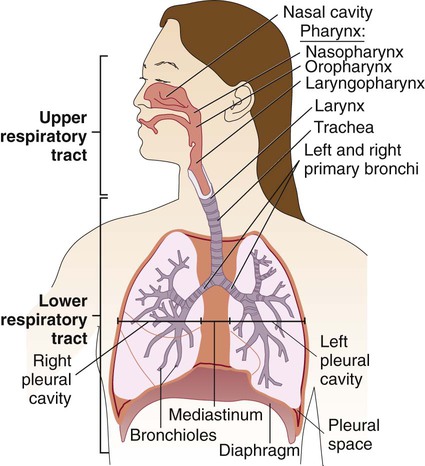
1. Define the trachea, bronchi, bronchioles, and alveoli, and explain the anatomic structure of the lower respiratory system. 2. List the most common etiologic agents responsible for lower respiratory disease and pneumonia in patients of various ages and categories: children <5 years of age, school-age children, young adults, older adults, and immunocompromised patients. 3. Describe the virulence factors found in bacteria and viruses associated with infection of the lower respiratory tract. 4. List the four possible routes of transmission or dissemination within the body that allow organisms to cause an infection in the lungs. 5. Name the most important decision for physicians regarding the treatment of pneumonia in older individuals, and list the three-step process used to guide them in this decision. 6. List the most prevalent cause of community-acquired pneumonia in adults. 7. Differentiate between community-acquired and hospital-acquired pneumonia. 8. State the factors anaerobic bacteria possess that enhance their ability to produce disease; explain how these anaerobes gain entrance to the lungs. 9. Define Lukens trap, and explain the type of patient or specimen associated with the method. 10. Describe the difference between early-onset or late-onset hospital- or ventilator-associated pneumonia. 11. List the etiologic agent of lung infections identified in cystic fibrosis patients. 12. Name the organisms most often associated with pneumo-opportunistic infection in HIV-positive individuals. 13. Explain the mechanisms that, because of the bacterial production of toxins, enable microorganisms to produce respiratory-associated disease. 14. Explain how the host immune system can contribute to microorganism growth in the respiratory disease process. 15. Explain why Mycobacterium tuberculosis is a classic representative of an intracellular pathogen. 16. Describe specimens collected for respiratory infections including determination of specimen quality and rejection criteria for the following: sputum, induced sputum, endotracheal suction, pleural fluid, bronchoalveolar lavage, bronchial washing, and bronchial brush sample. 17. Explain how the microbiologist would test for the less common causes of respiratory infection, including Pneumocystis jiroveci, Legionella spp., Chlamydophila pneumonia, Bordetella pertussis, Mycoplasma pneumonia, and Norcardia. The respiratory tract can be divided into two major areas: the upper respiratory tract consists of all structures above the larynx, whereas the lower respiratory tract follows airflow below the larynx through the trachea to the bronchi and bronchioles and then into the alveolar spaces where gas exchange occurs (Figure 69-1). The respiratory and gastrointestinal tracts are the two major connections between the interior of the body and the outside environment. The respiratory tract is the pathway through which the body acquires fresh oxygen and removes unneeded carbon dioxide. It begins with the nasal and oral passages, which humidify inspired air, and extends past the nasopharynx and oropharynx to the trachea and then into the lungs. The trachea divides into bronchi, which subdivide into bronchioles, the smallest branches that terminate in the alveoli. Some 300 million alveoli are estimated to be present in the lungs; these are the primary microscopic gas exchange structures of the respiratory tract. Familiarization with the anatomic structure of the thoracic cavity ensures proper specimen collection from various sites in the lower respiratory tract for processing by the laboratory. The thoracic cavity, which contains the heart and lungs, has three partitions separated from one another by pleura (see Figure 69-1). The lungs occupy the right and left pleural cavities, whereas the mediastinum (space between the lungs) is occupied mainly by the esophagus, trachea, large blood vessels, and heart. Microorganisms primarily cause disease by a limited number of pathogenic mechanisms (see Chapter 3). Because these mechanisms relate to respiratory tract infections, they are discussed briefly. Encounters between the human body and microorganisms occur many times each day. However, establishment of infection after such contact tends to be the exception rather than the rule. Whether an organism is successful in establishing an infection depends not only on the organism’s ability to cause disease (pathogenicity) but also on the human host’s ability to prevent the infection. In addition to these nonspecific host defenses, normal flora of the nasopharynx and oropharynx help prevent colonization by pathogenic organisms of the upper respiratory tract. Normal bacterial flora prevent the colonization by pathogens by competing for the same space and nutrients as well as production of bacteriocins and metabolic products that are toxic to invading organisms. Some of the bacteria that can be isolated as part of the indigenous flora of healthy hosts, as well as many species that may cause disease under certain circumstances and are often isolated from the respiratory tracts of healthy persons, are listed in Box 69-1. Under certain circumstances and for unknown reasons, these colonizing organisms can cause disease—perhaps because of previous damage by a viral infection, loss of some host immunity, or physical damage to the respiratory epithelium (e.g., from smoking). Differentiation of normal flora of the respiratory tract is important for determining the importance of an isolate in the clinical laboratory. Colonization does not always represent an infection. It is important to differentiate colonization from infection based on the specimen source, number of organisms present, and presence or quantity of white blood cells. (Organisms isolated from normally sterile sites in the respiratory tract by sterile methods that avoid contamination with normal flora should be definitively identified and reported to the clinician.) Certain microorganisms are almost always considered to be etiologic agents of disease if they are present in any numbers in the respiratory tract because they possess virulence factors that are expressed in every host. These organisms are listed in Box 69-2. The production of extracellular toxin was one of the first pathogenic mechanisms discovered among bacteria. Corynebacterium diphtheriae is a classic example of a bacterium that produces disease through the action of an extracellular toxin. Once the organism colonizes the upper respiratory epithelium, it produces a toxin that is disseminated systemically, adhering preferentially to central nervous system cells and muscle cells of the heart. Systemic disease is characterized by myocarditis, peripheral neuritis, and local disease that can lead to respiratory distress. Growth of C. diphtheriae causes necrosis and sloughing of the epithelial mucosa, producing a “diphtheritic (pseudo) membrane,” which may extend from the anterior nasal mucosa to the bronchi or may be limited to any area between—most often the tonsillar and peritonsillar areas. The membrane may cause sore throat and interfere with respiration and swallowing. Although nontoxic strains of C. diphtheriae can cause local disease, it is much milder than disease associated with toxigenic strains. The value of microbiologic studies to determine the cause of acute bronchitis in otherwise healthy individuals has not been established. Acute bronchitis is caused by viral agents, such as influenza and respiratory syncytial virus (RSV). The bacterium Bordetella pertussis is often associated with bronchitis in infants and preschool children (Table 69-1). The best specimen for diagnosis of pertussis is a deep nasopharyngeal specimen collected with a calcium alginate swab (see Chapter 37). TABLE 69-1 Major Causes of Acute Bronchitis Bronchiolitis, the inflammation of the smaller diameter bronchiolar epithelial surfaces, is an acute viral lower respiratory tract infection that primarily occurs during the first 2 years of life. Characteristic clinical manifestations include an acute onset of wheezing and hyperinflation as well as cough, rhinorrhea (runny nose), tachypnea (rapid breathing), and respiratory distress. The disease is primarily caused by viruses including a recently discovered virus, human metapneumovirus. RSV accounts for 40% to 80% of cases of bronchiolitis and demonstrates a marked seasonality; the etiologic agents of bronchiolitis are listed in Box 69-3. Like other viral infections, bronchiolitis shows a marked seasonality in temperate climates with a yearly increase in cases during winter to early spring. Initially, the virus replicates in the epithelium of the upper respiratory tract, but in the infant it rapidly spreads to the lower tract airways. Early inflammation of the bronchial epithelium progresses to necrosis. Symptoms such as wheezing may be related to the type of inflammatory response to the virus as well as other host factors. For the most part, patients are managed based on clinical parameters, with the laboratory having a role in cases that require hospitalization; a specific viral etiology can be identified in a large number of infants by viral isolation from respiratory secretions, preferably from a nasal wash (see Chapter 65). As previously mentioned, there are two major categories of pneumonias: those considered community-acquired pneumonias and hospital-, ventilator-, or health care–associated pneumonias. Because the epidemiology and etiologies can differ, these two categories are discussed separately. Pneumonia in the immunocompromised patient is addressed separately in this chapter. Emerging viral infections associated with severe acute respiratory syndrome (SARS) and influenza outbreaks (H1N1) are typically associated with upper respiratory infections but may lead to serious lower respiratory infections in the young, elderly, or immunocompromised patient. See Chapter 66 for detailed information related to these emerging viral infectious diseases and diagnostic recommendations.
Infections of the Lower Respiratory System
General Considerations
Anatomy
Pathogenesis of the Respiratory Tract: Basic Concepts
Host Factors
Microorganism Factors
Toxins.
Diseases of the Lower Respiratory Tract
Bronchitis
Acute
Bacteria
Viruses
Bordetella pertussis,
B. parapertussis,
Mycoplasma pneumoniae,
Chlamydia pneumoniae
Influenza virus, adenovirus, rhinovirus, coronavirus (other less common viruses: respiratory syncytial virus, human metapneumovirus, coxsackie A21 virus)
Bronchiolitis
Pneumonia
Epidemiology/Etiologic Agents