DRUG CLASSES
Hematopoietic factors for bleeding and infection
Hematopoietic factors for anemia
PHARMACOLOGY IN PRACTICE

Mr. Phillip, age 72 years, has chronic kidney disease. He had a friend who was on dialysis about 5 years ago and complained of being tired all the time. They gave him “shots” to perk him up but instead he had a heart attack. Mr. Phillip is concerned about his kidney disease progressing and having to start dialysis, and wonders if the same thing could happen to him.
An immunostimulant is an agent that stimulates the immune system. In Chapter 49, vaccines (that stimulate us to make specific antibodies) were presented. Two other classes used to boost the immune system are the interferons and the interleukins. Interferons modulate the response of the immune system to viruses, bacteria, cancer, and other foreign substances that invade the body. Interferons do not kill viral or cancer cells; they boost the immune system response and reduce the growth by controlling cellular proteins controlling growth. There are basically three types of interferons: (1) interferon-alpha (α) is used for treating cancers and viral infections, (2) interferon-beta (β) is used for treating multiple sclerosis, and (3) interferon-gamma (γ) is used for treating hereditary immune system disorders. Interleukins are a group of chemicals called cytokines. The white blood cells normally make interleukins. Different interleukins help the body’s immune system respond to inflammation.
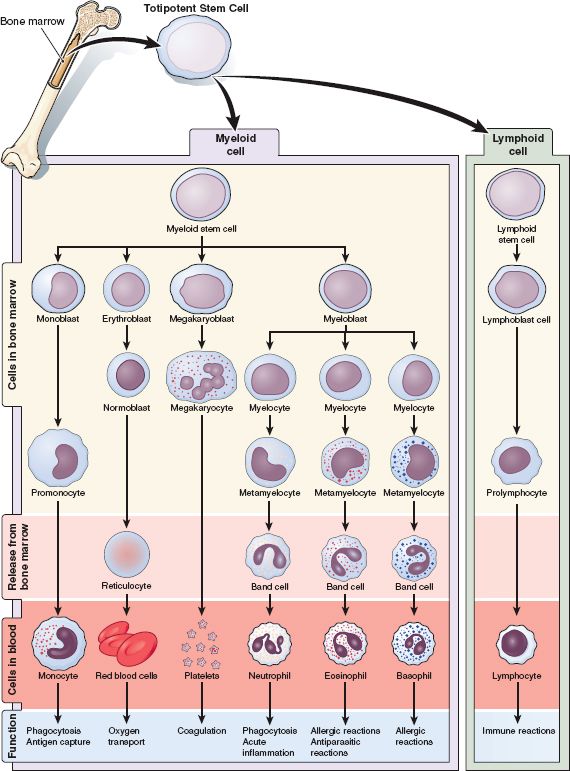
This chapter focuses on the colony-stimulating factors (CSFs), a group of immunostimulants used in cancer treatment and chronic renal failure to support the hematopoietic system. The hematopoietic system is composed of fluids and particles that are known as blood. Blood is a complex fluid that circulates continuously through the heart and blood vessels and to the outermost cells of our body tissues. Three distinct cells circulate in the blood:
• Red blood cells (RBCs, erythrocytes) that supply our cells with oxygen from the lungs to the tissues
• White blood cells (WBCs, leukocytes) that protect our bodies from dangerous microorganisms
• Platelets (megakaryocytes) that control the bleeding from microscopic to major tears in our tissues
Chronic diseases such as chronic kidney disease or medical treatments such as chemotherapy can cause a hematologic failure. When this happens, inadequate numbers of cells are produced. As a result, the body can no longer meet the demands for oxygen transportation, blood coagulation, or prevention of invasion of microorganisms. Anemia, bleeding, and infection can result.
The goal for treating these hematologic problems is to stimulate the body to make more of the specific blood cells. This process is called hematopoiesis. During this process, undifferentiated stem cells in the bone marrow are signaled to multiply and differentiate into erythrocytes, leukocytes, or megakaryocytes (Fig. 51.1). Hematopoietic drugs help to enhance this process and are used to treat anemia, bleeding, and infection.
HEMATOPOIETIC DRUGS USED IN TREATING POTENTIAL BLEEDING OR INFECTION
There are a number of different WBCs that protect the body from microbial invasion and infection. The WBC known as the neutrophil is one of the major cells in the line of defense from infection. Neutropenia is the term for the condition that results when the neutrophil level in the blood is low. Infection is likely to occur when a patient is neutropenic. Neutrophils have an extremely short lifespan (6 to 8 hours), meaning that they rapidly grow and divide. Because of their rapid growth cycle, the neutrophil is a target of the cancer chemotherapy drugs, as well as the cancer cells themselves. Chemotherapy-induced neutropenia is a major reason that cancer treatments may be delayed or cancelled. When this happens, the patient is at a greater risk for continued growth of the cancer or illness from the treatment. CSFs are drugs used to stimulate the growth and production of WBCs to help fight off infection.
Platelets are important to normal blood clotting. They are formed from megakaryocytes in the blood. The megakaryocyte is a large blood cell that can divide into many platelets. A low platelet count is a condition called thrombocytopenia. Decreased platelet production can also be caused by anemia. The interleukin drug oprelvekin is used when sufficient platelets are not made to meet the body’s needs. Sometimes the body does not make enough platelets due to unknown causes; this is termed idiopathic (or immune) thrombocytopenic purpura or ITP. Drugs to treat this disorder are appearing in the drug market.
COLONY-STIMULATING FACTORS
Actions and Uses
CSFs are glycoproteins that act on the hematopoietic cells to stimulate proliferation, differentiation, and maturation of WBCs. CSFs are used to treat or prevent infection (by minimizing neutropenia) associated with the following:
• Chemotherapy-induced neutropenia during solid tumor cancer treatment
• Neutropenia during bone marrow transplantation (BMT)
• Production of stem cells for harvest before bone marrow transplant
• Neutropenia in those susceptible to symptomatic chronic infection
Injections of the CSF filgrastim are started at least 24 hours after the completion of a cycle of chemotherapy. The absolute neutrophil count (ANC) is monitored and therapy is continued until an ANC count of at least 10,000/mm3 is achieved. It is not recommended to use the drug for longer than 2 weeks, and treatment is discontinued at least 1 day before the next chemotherapy cycle is to begin. Special instruction is needed in cases of bone marrow transplant or stem cell harvest.
Pegfilgrastim is similar to filgrastim but is given as a single dose between chemotherapy cycles. Sargramostim is used following BMT, following induction chemotherapy used with leukemia, and to stimulate stem cells for harvest.
Adverse Reactions
General System Reactions
• Bone pain
• Hypertension
• Nausea and vomiting
• Alopecia
• Hypersensitivity or allergic reactions
See the Summary Drug Table: Immunostimulant Drugs for more information on these drugs.
Contraindications, Precautions, and Interactions
CSFs are contraindicated in patients with known hypersensitivity to the drug or any component of the drug. Filgrastim is used cautiously in patients with hypothyroid disease. The CSFs are pregnancy category C drugs, and caution is used when the patient is breastfeeding. Pegfilgrastim can cause a sickle cell crisis in those with the disease. CSFs can cause hypersensitive reactions and should be treated with antihistamines, steroids, and bronchodilators to maintain their use. These drugs can stimulate cancer cell growth in cancer types that are stimulated by growth factors. An even higher increase in neutrophil count can occur when these drugs are taken with lithium, a drug used for the manic phase of mood disorders. The CSFs are currently in study phases to assess safety in children.
Figure 51.1 Hematopoiesis. (From McConnell, T. H. [2007]. The nature of disease pathology for the health professions. Philadelphia: Lippincott Williams & Wilkins.)
DRUGS USED TO TREAT THROMBOCYTOPENIA
Actions and Uses
Oprelvekin is a drug that stimulates thrombopoiesis. Thrombopoiesis is the process of making platelets. The drug is used to prevent severe thrombocytopenia and reduces the need for multiple platelet transfusions. Oprelvekin is used to treat or prevent thrombocytopenia associated with chemotherapy for solid tumor cancer treatment.
Injections are started at least 6 hours after the completion of a chemotherapy cycle. Platelet counts are monitored and therapy is continued until a count of at least 50,000/mcL is achieved. It is not recommended for use for more than 21 days; treatment is discontinued at least 2 days before the next chemotherapy cycle is to begin.
ITP can be an acute or chronic bleeding disorder. Sometimes it is associated with other diseases. It is typically diagnosed by signs of bleeding (purple areas on the skin) or fatigue. If it does not resolve on its own, then a course of corticosteroids (see Chapter 43) or removal of the spleen may help. Two products are now available should these treatments prove unsuccessful: eltrombopag and romiplostim. Both of these drugs are used only for ITP and are not to be used to increase platelet count associated with immunosuppression during chemotherapy.
Adverse Reactions
General System Reactions
• Fluid retention
• Peripheral edema
• Dyspnea
• Syncope
• Fever
• Allergic reactions
Cardiovascular System Reactions
• Tachycardia
• Palpitations
• Atrial fibrillation
• Arrhythmias resulting in stroke and pulmonary edema
• Capillary leak syndrome
Eltrombopag can be toxic to the liver. Liver function studies are done prior to starting the drug and every 2 weeks while on drug therapy. See the Summary Drug Table: Immunostimulant Drugs for more information on these drugs.
Contraindications, Precautions, and Interactions
Thrombopoietin drugs are contraindicated in patients with known hypersensitivity to the drug or any component of the drug. Oprelvekin should not be used in patients receiving chemotherapy that is extremely myelosuppressive. These drugs are used cautiously in patients with renal failure, heart failure, or atrial arrhythmias. Severe hypokalemia (low potassium levels) can occur if the patient is receiving the cancer chemotherapy agent ifosfamide. It is a pregnancy category C drug and lactating patients should stop breastfeeding when oprelvekin is prescribed. Safety in children has not been established.
Oprelvekin can cause anaphylactic-type reactions and should be permanently discontinued if these occur. Discontinuing either eltrombopag or romiplostim may result in platelet counts lower than the original diagnosed counts.
HEMATOPOIETIC DRUGS USED IN TREATING ANEMIA
Anemia is a condition caused by an insufficient amount of hemoglobin delivering oxygen to the tissues. Causes of anemia include a decrease in the number of RBCs, a decrease in the amount of hemoglobin in RBCs, or both. There are various types and causes of anemia. For example, anemia can result from blood loss, excessive destruction of RBCs, inadequate production of RBCs, and deficits in various nutrients, as in iron deficiency anemia. Once the type and cause have been identified, the primary health care provider selects a method of treatment.
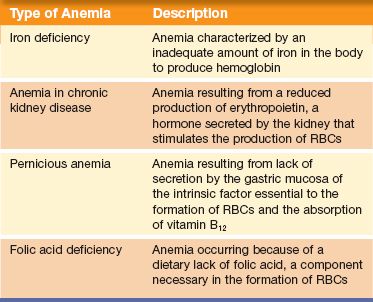
The anemias discussed in this chapter include anemia in patients with chronic illness such as renal disease or caused by treatment, iron deficiency anemia, pernicious anemia, and anemia resulting from a folic acid deficiency. Table 51.1 defines these anemias.
Table 51.1 Anemias
DRUGS USED IN TREATING ANEMIA ASSOCIATED WITH CHRONIC ILLNESS
Anemia may occur in patients with chronic illness as a result of disease treatment. Cancer and chronic kidney disease are two diseases that produce disease- or treatment-related anemia. Erythropoiesis-stimulating agents (ESAs) are glycoproteins that stimulate and regulate the production of erythrocytes. Chronic kidney disease reduces the kidney’s ability to produce erythropoietin, which stimulates the production of RBCs. Cancer treatment reduces the bone marrow’s ability to produce RBCs. Two examples of drugs used to treat anemia associated with chronic illness are epoetin alfa (Epogen) and darbepoetin alfa (Aranesp).
Actions and Uses
ESAs are drugs that, like natural erythropoietin, stimulate erythropoiesis, the process of making RBCs. ESAs are used to treat anemia associated with the following:
• Chronic kidney disease
• Chemotherapy for cancer treatment
• Zidovudine (AZT) therapy for human immunodeficiency virus (HIV) infection
• Postsurgical blood replacement in place of allogeneic transfusions
Darbepoetin alfa and methoxy polyethylene–epoetin β are erythropoiesis-stimulating proteins used to treat anemia associated with chronic kidney disease in patients receiving dialysis, as well as in patients who are not receiving dialysis. These drugs elevate or maintain RBC levels and decrease the need for transfusions.
Adverse Reactions
Epoetin alfa (erythropoietin; EPO), darbepoetin alfa, and methoxy polyethylene are usually well tolerated when used to maintain a hemoglobin no higher than 12g/dL. The most common adverse reactions include:
• Hypertension
• Headache
• Nausea, vomiting, diarrhea
• Rashes
• Fatigue
• Arthralgia, and skin reaction at the injection site
See the Summary Drug Table: Immunostimulant Drugs for more information on these drugs.
Contraindications and Precautions
Epoetin alfa is contraindicated in patients with uncontrolled hypertension, those needing an emergency transfusion, and those with a hypersensitivity to human albumin. Darbepoetin alfa (Aranesp) is contraindicated in patients with uncontrolled hypertension or in those allergic to the drug. Polycythemia (an overload of RBCs in the circulation) can occur if the hemoglobin is not carefully monitored and the dosage is too high. This can result in increased mortality, serious cardio or thromboembolic events in any patient, and possible tumor progression in cancer patients.
Epoetin alfa and darbepoetin alfa are used with caution in patients with hypertension, heart disease, congestive heart failure, or a history of seizures. Both of these drugs are pregnancy category C drugs and are used cautiously during pregnancy and lactation.
DRUGS USED IN TREATING IRON DEFICIENCY ANEMIA
When the body does not have enough iron to supply its own needs, the resulting condition is called iron deficiency anemia. Iron is the component in hemoglobin that picks up oxygen from the lungs and carries it to the body tissues. Iron deficiency anemia is a very common type of anemia. Approximately 50% of pregnant women and 20% of all women experience anemia. Decreased iron stores result from a decrease in RBCs; causes include heavy menstrual bleeding and poor absorption or lack of iron in the diet.
Actions and Uses
Iron preparations act by elevating the serum iron concentration, which replenishes hemoglobin and depleted iron stores. Oral iron supplements are typically used. Iron is best absorbed on an empty stomach. Supplemental iron is needed during pregnancy and lactation, because normal dietary intake rarely supplies the required amount.
Parenteral iron is used when the patient cannot take oral drugs or when the patient experiences gastrointestinal (GI) intolerance to oral iron administration. Other iron preparations, both oral and parenteral, used in treating iron deficiency anemia can be found in the Summary Drug Table: Immunostimulant Drugs.
Adverse Reactions
Gastrointestinal Reactions
• GI irritation
• Nausea, vomiting
• Constipation, diarrhea
• Darker (black) stools
Generalized System Reactions
• Headache
• Backache
• Allergic reactions
When given parenterally, additional adverse reactions include soreness, inflammation, and sterile abscesses at the intramuscular (IM) injection site. When iron is administered by the IM route, a brownish discoloration of the skin may occur. Intravenous (IV) administration may result in phlebitis at the injection site.
Contraindications and Precautions
Iron supplements are contraindicated in patients with known hypersensitivity to the drug or any component of the drug. Iron compounds are contraindicated in patients with hemochromatosis or hemolytic anemia. Iron compounds are used cautiously in patients with hypersensitivity to aspirin, because these patients may have a hypersensitivity to the tartrazine or sulfite content of some iron compounds.
The parenteral form of iron can cause anaphylactic-type reactions and should be used only when oral supplement is contraindicated.
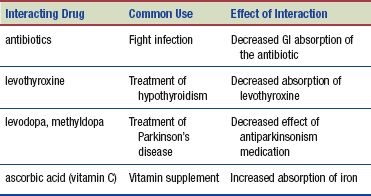
Interactions
The following interactions may occur when an iron preparation is administered with another agent:
DRUGS USED IN TREATING FOLIC ACID DEFICIENCY ANEMIA
Folic acid (folate) is required for the manufacture of RBCs in the bone marrow. Folic acid is found in leafy green vegetables, fish, meat, poultry, and whole grains. A deficiency of folic acid results in megaloblastic anemia. Megaloblastic anemia is characterized by the presence of large, abnormal, immature erythrocytes circulating in the blood.
Actions and Uses
Folic acid is used in treating megaloblastic anemias that are caused by a deficiency of folic acid. Although neural tube defects are not related to anemia, studies indicate there is a decreased risk for embryonic neural tube defects if folic acid is taken before conception and during early pregnancy. Neural tube defects occur during early pregnancy, when the embryonic folds forming the spinal cord and brain join together. Defects of this type include anencephaly (congenital absence of brain and spinal cord), spina bifida (defect of the spinal cord), and meningocele (a sac-like protrusion of the meninges in the spinal cord or skull). The U.S. Public Health Service recommends the use of folic acid for all women of childbearing age to decrease the incidence of neural tube defects. Dosages during pregnancy and lactation are as great as 0.8 mg/day.
Oral supplements are the first choice for megaloblastic anemia and folic acid deficiency treatment. If a patient is unable to take oral medications, leucovorin may be used. This drug is a derivative (an active reduced form) of folic acid. Leucovorin is more commonly used to diminish the hematologic effects of methotrexate, a drug used in treating certain types of cancer (see Chapter 50). Leucovorin “rescues” normal cells from the destruction caused by methotrexate and allows them to survive. This technique of administering leucovorin after a large dose of methotrexate is called folinic acid rescue or leucovorin rescue.
Adverse Reactions
Few adverse reactions are associated with the administration of folic acid. Rarely, parenteral administration may result in allergic hypersensitivity.
Contraindications and Precautions
Folic acid and leucovorin are contraindicated for treating pernicious anemia or for other anemias in which vitamin B12 is deficient. Folic acid is a pregnancy category A drug and is generally considered safe for use during pregnancy. Pregnant women are more likely to experience folate deficiency, because folic acid requirements increase during pregnancy. Pregnant women with a folate deficiency are at increased risk for complications of pregnancy and fetal abnormalities. The recommended dietary allowance (RDA) of folate during pregnancy is 0.4 mg/day and, during lactation, 0.26 to 0.28 mg/day. Although the potential for fetal harm appears remote, the drug should be used cautiously and only within the RDA guidelines.
Interactions
Signs of folate deficiency may occur when sulfasalazine is administered concurrently. An increase in seizure activity may occur when folic acid is administered with the hydantoins (antiseizure drugs).
DRUGS USED IN TREATING VITAMIN B12 DEFICIENCY ANEMIA
Vitamin B12 is essential to growth, cell reproduction, the manufacture of myelin (which surrounds some nerve fibers), and blood cell manufacture. The intrinsic factor, which is produced by cells in the stomach, is necessary for the absorption of vitamin B12 in the intestine. A deficiency of the intrinsic factor results in abnormal formation of erythrocytes because of the body’s failure to absorb vitamin B12, a necessary component for blood cell formation. The resulting anemia is called macrocytic anemia.
Actions and Uses
Vitamin B12 (cyanocobalamin) is used to treat patients with a vitamin B12 deficiency; this condition is seen in those who have:
• A strict vegetarian (vegan) lifestyle
• Total gastrectomy or subtotal gastric resection (in which the cells producing the intrinsic factor are totally or partially removed)
• Intestinal diseases, such as ulcerative colitis or sprue
• Gastric carcinoma
• Congenital decrease in the number of gastric cells that secrete intrinsic factor
Vitamin B12 is also used to perform the Schilling test, which is used to diagnose pernicious anemia.
Pernicious anemia must be diagnosed and treated as soon as possible, because vitamin B12 deficiency that is allowed to progress for more than 3 months may result in degenerative lesions of the spinal cord.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 NURSING ALERT
NURSING ALERT