What are the major steps involved in migration of leukocytes from the vasculature into the extravascular space?
Leukocyte migration involves rolling of leukocytes along the endothelial surface, firm adhesion to the endothelial surface, release of endothelial damaging agents, and migration of leukocytes into the extravascular space by diapedeses.
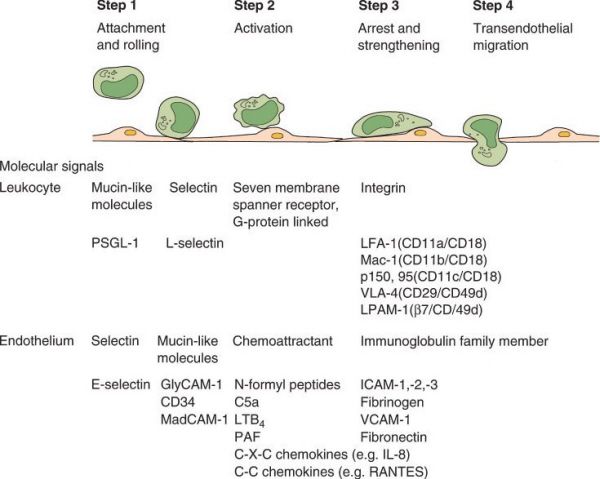
Leukocyte migration. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Leukocyte Migration
•Leukocyte adhesion and transmigration are regulated by
•Binding of complementary adhesion molecules on leukocyte and endothelial surfaces
•Chemical mediators (chemoattractants)
•Cytokines modulating the surface expression or avidity of adhesion molecules
•Cells involved in the emigrating leukocyte response varies over time
•Neutrophils predominate in the first 6 to 24 hours
•Monocytes predominate in the next 24 to 48 hours
•Lymphocytes may be the first cells in a viral infection
•Eosinophilic granulocytes are the first to arrive in hypersensitivity reactions
•The initial rolling of leukocytes along endothelial surfaces is mediated by a family of proteins located on endothelial and leukocyte surfaces called selectins
•Endothelial selectins
•Cytokines including TNF, IL-1, and lipopolysaccharides induce expression of E-selectin and P-selectin
•P-selectin is mobilized from intracellular storage granules as well as de novo synthesis with cytokine stimulation
•E-selectin is made by de novo synthesis with cytokine stimulation
•L-selectin is constitutively expressed on leukocytes
•This slowing of leukocytes allows for activation of β2 integrins, constitutively expressed on the leukocyte surface, by various chemokines
•Activated endothelial cells express ICAM-1 and ICAM-2, which bind to the β2 integrins, resulting in firm adhesion of leukocytes to the endothelial cells
•Release of proteases and oxidants by adhered leukocytes damages the endothelial cells and increases microvascular permeability, allowing the leukocytes to enter the extra-vascular space via diapedeses
A 62-year-old female ICU patient is febrile, breathing 32 times a minute, and has a white count of 16,500 cells/mm3. She is not on any pressors or inotropic support and has no positive cultures from any source. What is her inflammatory state?
She has systemic inflammatory response syndrome (SIRS).
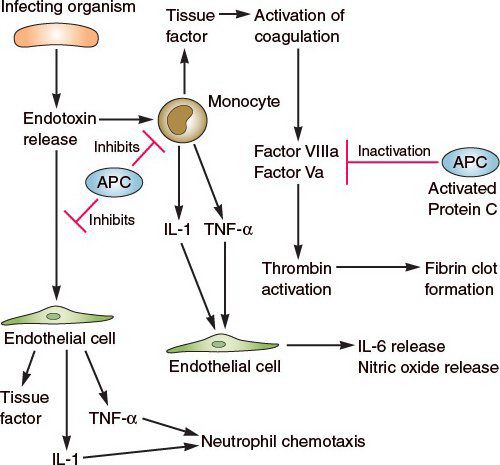
Cells and inflammatory mediators involved in SIRS. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
The Acute Phase Response in SIRS
•Fever due to exogenous pyrogens (bacterial products like lipopolysaccharide) that stimulate leukocytes to produce endogenous pyrogens (IL-1 and TNF-α), which together stimulate prostaglandin synthesis
•This causes an increase in neurotransmitters like cyclic AMP that reset the temperature set point at a higher level
•IL-6, IL-1, and TNF-α increase the acute phase proteins synthesized by the liver and magnify the response to inflammation
•WBC increases, especially in the presence of a bacterial infection
•The leukocytosis is initially because of an accelerated release of cells from the bone marrow’s post-mitotic reserve pool and is associated with a rise in the number of more immature neutrophils in the blood (left shift)
A patient presenting with jaundice and right upper quadrant pain is suspected to have acute HBV infection. What will likely be detected in serum hepatitis studies?
HBV DNA, HBsAg, HBeAg, anti-HBsAb, and IgM anti-HBcAb
•Hepatitis B virus (HBV) is a double stranded virus with three major antigens (Ag):
•HBsAg (envelope surface antigen)
•HBcAg (core antigen)
•HBeAg (a glycoprotein antigen associated with the core)
•The incubation time of HBV is 8 weeks
•The first serum indicator is HBsAg, which can precede symptoms
•Acute HBV infection is associated with serum HBV DNA and serum HbeAg
•IgM anti-HBc Antibody (Ab) occurs during clinical hepatitis at 4 to 12 weeks after infection
•Presence of serum IgM anti-HBcAb is used to distinguish acute from chronic HBV infection
•In most cases where chronic infection is not present, IgM anti-HbcAb does not persist beyond 6 months after infection
•IgM anti-HBcAb is not protective against the disease
•Anti-HBeAb appears 4 months after infection, clears the HBeAg, but does not protect against the disease
•Anti-HBsAb starts to appear during recovery from acute hepatitis (as soon as 2 weeks after infection) and is associated with elimination of infection
•Hep B vaccine consists of recombinant HBsAg. Injection results in production of anti-HBsAb and is protective against reinfection.
Which cytokines are most important in stimulating hepatic acute phase proteins?
IL-6 and IL-1.
Hepatic Acute Phase Proteins
•The acute phase response to cell injury/trauma occurs 6 hours after the event
•Acute phase proteins change in concentration by at least 25% during this inflammation period
•Type I proteins: C-reactive protein (CRP), serum amyloid A (SAA), and C3
•Stimulated by IL-1 and TNF
•Type II proteins: Fibrinogen, haptoglobin, ceruloplasmin, α1-antitrypsin, α1-antichymotrypsin
•Stimulated by IL-6
•CRP
•Activates complement
•Recognizes foreign pathogens and binds to phagocytic cells
•Activates tissue factor to initiate the coagulation cascade
•Peaks 48 hours after the event and returns to baseline after 8 days
•Albumin and transferrin concentrations decrease in the acute phase response
A patient with diabetes mellitus is about to undergo a routine elective right hemicolectomy. Besides appropriate timing and choice of prophylactic antibiotic administration, what is the most important variable in preventing a surgical site infection?
Beyond intraoperative contamination, normoglycemia, both during and following a surgical procedure, is important in preventing a surgical site infection.
Postoperative Blood Glucose Control
•Immunologic deficiencies occur when blood glucose is poorly controlled
•Impaired neutrophil chemotaxis and phagocytosis
•Reduced CD4 cell counts
•Both are reversible with the correction of hyperglycemia
•Glucose toxicity injures the mitochondrial compartment and innate immunity
In diabetic surgical patients, both hyperglycemia and poor tissue perfusion due to microvascular and large vessel disease contribute to infection.
A patient is treated with prednisone for rheumatoid arthritis. What are the possible side effects of high-dose, prolonged steroid therapy?
Adrenal atrophy, impaired glucose control, immunosuppression, impaired wound healing, osteoporosis, glaucoma, cataracts, hypertension, and peptic ulcer disease.
Steroids
•Inhibit prostaglandin synthesis by repression of cyclooxygenase-2 transcription
•Induce MAPK phosphatase, preventing the transcription of genes encoding inflammatory proteins via the c-Jun transcription factor pathway
•Block NF-kB activity by direct binding to the glucocorticoid receptor in the nucleus
•NF-kB stimulates transcription of cytokines, chemokines, complement factors, cell-adhesion molecules, and cyclooxygenase-2
•Side effects of high dose/prolonged steroid therapy
•Adrenal atrophy
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


