Chapter 17 The management of hypertension in general is discussed, with emphasis on the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines. Many alternative treatment protocols have been proposed. The JNC 8 is due to be published in 2013. The drugs most commonly used for hypertension are diuretics, β-blockers, calcium channel blockers, ACE inhibitors, and angiotensin II receptor blockers (ARBs). How these drugs are used to treat hypertension is discussed in this chapter. Detailed information on these antihypertensives is given in the specific drug chapters (Table 17-1). This chapter provides detailed information on other antihypertensive medications used in primary care. TABLE 17-1 Drugs Commonly Used for Hypertension (listed in order of use) Some conditions produce secondary hypertension as a consequence of other disease. The hypertension that results from these conditions is often treatable (see Table 17-3). The cause of primary hypertension (which accounts for approximately 95% of cases of hypertension) remains unknown. Although these are not completely understood, many factors have been linked to primary hypertension, including some that are genetically determined. Involved mechanisms include elevated peripheral resistance, alteration in the cell membrane related to elevated lipids, endothelial dysfunction, changes in sodium or calcium levels, and hyperinsulinemia. Sympathetic nervous system hyperactivity caused by insensitivity of the baroreflexes may contribute to hypertension accompanied by tachycardia and elevated cardiac output in younger patients. TABLE 17-3 Secondary Causes of Hypertension A “metabolic syndrome” has recently been identified as a major cardiac risk factor. This constellation of symptoms is also referred to as syndrome X, the insulin resistance syndrome, or the obesity dyslipidemia syndrome. A patient who has abdominal obesity, hypertension, insulin resistance, and a lipid disorder has a greatly elevated risk of CVD. Instead of serving as separate risk factors, they work together to increase risk. Table 17-2 lists the major cardiovascular risk factors. The WHO diabetes group proposed a set of criteria for diagnosing the metabolic syndrome in 1998 and later updated these (Grundy et al, 2004). This definition is as follows: TABLE 17-2 Major Cardiovascular Risk Factors for Hypertension Metabolic syndrome Hypertension Dyslipidemia Obesity (body mass index [BMI] ≥30)∗ Diabetes mellitus Cigarette smoking Physical inactivity Microalbuminuria or estimated glomerular filtration rate (GFR) <60 ml/min Family history of premature cardiovascular disease (men younger than age 55 or women younger than 65 years) ∗Body mass index is calculated as: From Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure Education Program: The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, NIH publication No. 03-5233, Bethesda, MD, May 2003, National Institutes of Health, National Heart, Lung, and Blood Institute. PLUS at least two of the following: 1. Abdominal obesity, defined as a waist-to-hip ratio greater than 0.90, a body mass index (BMI) ≥30 kg/m2, or a waist-to-girth ratio ≥0.9 in men and 0.85 in women 2. Dyslipidemia, defined as serum triglycerides 150 mg/dl (1.7 mmol/L) 3. HDL cholesterol <35 mg/dl (0.9 mmol/L) in men or <39 mg/dl (1.0 mmol/L) in women 4. BP ≥140/90 mm Hg or the administration of antihypertensive drugs 5. Urinary albumin excretion rate >20 mcg/min or albumin-to-creatinine ratio >30 mg/g Fifty million Americans have hypertension, and the prevalence increases with age. Only about 34% of these people are adequately treated. Hypertension is a risk factor for CVD, stroke, CHF, renal failure, and peripheral vascular disease. CVD and stroke are the most common causes of death in the United States. Current levels of cardiovascular morbidity and mortality show that much greater effort is required to control hypertension (ALLHAT, 2002). The diagnosis of hypertension is based on the average of readings taken at an initial screening and two or more readings taken at each of two or more subsequent visits. The readings on these three separate occasions should not be influenced by any other known mechanism, such as recent exercise, anxiety, or an acute illness. Initial evaluation includes a thorough history, physical examination, and laboratory screening (Box 17-1). Once the diagnosis of hypertension is made, further evaluation of three factors that are affecting the patient’s risk is necessary. Severity should be determined according to the classification in Table 17-4. Next, target organ damage (Table 17-5), which is the damage the hypertension has already caused, should be evaluated. Finally, assessment should be completed for compelling indications (Table 17-6), which include conditions managed in parallel with HTN. These three factors will affect management. TABLE 17-4 JNC 7 Classification and Management of Blood Pressure for Adults From Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure Education Program: The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, NIH Publication No. 03-5233, Bethesda, MD, May 2003, National Institutes of Health, National Heart, Lung, and Blood Institute. TABLE 17-5 Target Organ Damage Occurring with Hypertension
Hypertension and Miscellaneous Antihypertensive Medications
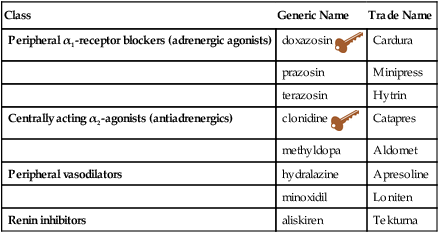
Class
Generic Name
Trade Name
Peripheral α1-receptor blockers (adrenergic agonists)
doxazosin ![]()
Cardura
prazosin
Minipress
terazosin
Hytrin
Centrally acting α2-agonists (antiadrenergics)
clonidine ![]()
Catapres
methyldopa
Aldomet
Peripheral vasodilators
hydralazine
Apresoline
minoxidil
Loniten
Renin inhibitors
aliskiren
Tekturna
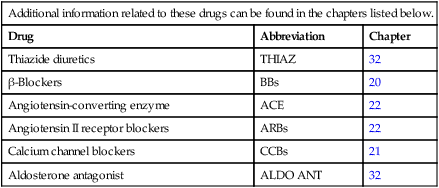
Additional information related to these drugs can be found in the chapters listed below.
Drug
Abbreviation
Chapter
Thiazide diuretics
THIAZ
32
β-Blockers
BBs
20
Angiotensin-converting enzyme
ACE
22
Angiotensin II receptor blockers
ARBs
22
Calcium channel blockers
CCBs
21
Aldosterone antagonist
ALDO ANT
32
Therapeutic Overview of Hypertension
Anatomy and Physiology
Pathophysiology
Pathology
Signs and Symptoms
Diagnostic Studies
Coarctation of the aorta
Delayed or absent femoral arterial pulses, decreased BP in lower extremities
ECG, chest x-ray studies, echocardiography, Doppler ultrasonography
Cushing’s syndrome
Long-term steroid use: truncal obesity with purple striae, moon facies
Morning plasma cortisol after 1 mg hour of sleep dexamethasone
Pheochromocytoma
Labile HTN, tachycardia, headache, palpitations, pallor, sweating, or tremors
Spot urine for metanephrine
Primary aldosteronism
Muscle weakness, polydipsia, polyuria
Hypokalemia, excessive urinary potassium excretion, suppressed levels of plasma renin activity, elevated sodium level
Chronic kidney disease
Abdominal or flank masses (polycystic kidneys)
Urinalysis, creatinine, renal ultrasound
Renovascular disease
Epigastric or renal artery bruits, atherosclerotic disease of aorta or peripheral arteries
Renal duplex ultrasound, renal arteriography
Sleep apnea
Fatigue, loud cyclic snoring
Polysomnography
Hyperthyroidism
Weight loss, fatigue, tachycardia
TSH, T4, free T4, free T4 index
Hypothyroidism
Weight gain, fatigue
May be due to decreased tissue metabolism leading to low production of vasodilating metabolites
Hyperparathyroidism
Renal stones, polyuria, constipation
Serum and urine calcium, urine phosphate, serum parathyroid hormone

Disease Process
Assessment
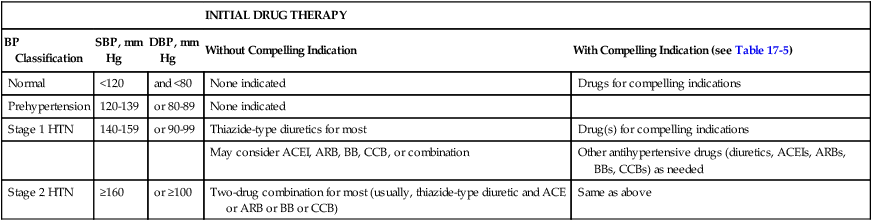
INITIAL DRUG THERAPY
BP Classification
SBP, mm Hg
DBP, mm Hg
Without Compelling Indication
With Compelling Indication (see Table 17-5)
Normal
<120
and <80
None indicated
Drugs for compelling indications
Prehypertension
120-139
or 80-89
None indicated
Stage 1 HTN
140-159
or 90-99
Thiazide-type diuretics for most
Drug(s) for compelling indications
May consider ACEI, ARB, BB, CCB, or combination
Other antihypertensive drugs (diuretics, ACEIs, ARBs, BBs, CCBs) as needed
Stage 2 HTN
≥160
or ≥100
Two-drug combination for most (usually, thiazide-type diuretic and ACE or ARB or BB or CCB)
Same as above
HEART
Left ventricular hypertrophy
Angina or prior myocardial infarction
Prior coronary revascularization
Heart failure
BRAIN
Stroke or transient ischemic attack
Chronic kidney disease
Peripheral arterial disease
Retinopathy ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hypertension and Miscellaneous Antihypertensive Medications
Only gold members can continue reading. Log In or Register to continue
