65
Hypersensitivity (Allergy)
CHAPTER CONTENTS
INTRODUCTION
Hypersensitivity is the term used when an immune response results in exaggerated or inappropriate reactions harmful to the host. The term allergy is often equated with hypersensitivity but more accurately should be limited to the IgE–mediated reactions discussed later in the section “Type I: Immediate (Anaphylactic) Hypersensitivity.”
The clinical manifestations of these reactions are typical in a given individual and occur on contact with the specific antigen to which the individual is hypersensitive. The first contact of the individual with the antigen sensitizes (i.e., induces the antibody), and the subsequent contacts elicit the allergic response.
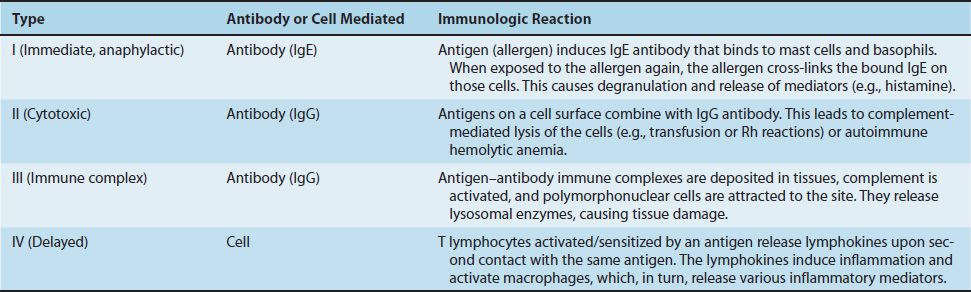
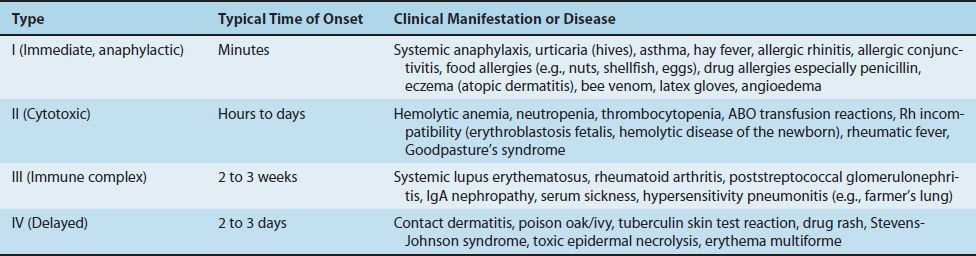
Hypersensitivity reactions can be subdivided into four main types. Types I, II, and III are antibody-mediated, whereas type IV is cell-mediated (Table 65–1). Type I reactions are mediated by IgE, whereas types II and III are mediated by IgG. The immunologic reactions are summarized in Table 65–1. The clinical manifestations of the hypersensitivity reactions are described in Table 65–2.
TYPE I: IMMEDIATE (ANAPHYLACTIC) HYPERSENSITIVITY
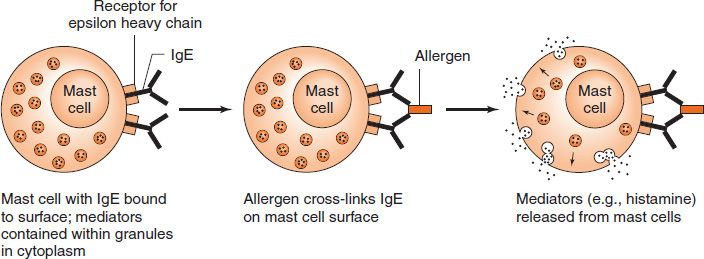
An immediate hypersensitivity reaction occurs when an antigen (allergen) binds to IgE on the surface of mast cells with the consequent release of several mediators (see list of mediators that follows) (Figure 65–1). The process begins when an antigen induces the formation of IgE antibody, which binds firmly by its Fc portion to receptors on the surface of basophils and mast cells. Reexposure to the same antigen results in cross-linking of the cell-bound IgE, degranulation, and release of pharmacologically active mediators within minutes (immediate phase). Cyclic nucleotides and calcium play essential roles in release of the mediators.1 Symptoms such as edema and erythema (“wheal and flare”) and itching appear rapidly because these mediators (e.g., histamine) are preformed.
The late phase of IgE-mediated inflammation occurs approximately 6 hours after exposure to the antigen and is due to mediators (e.g., leukotrienes [SRS-A]) that are synthesized after the cell degranulates. These mediators cause an influx of inflammatory cells, such as neutrophils and eosinophils, and symptoms such as erythema and induration occur. For example, eosinophils play a major role in the late-phase reaction in asthma.
Complement is not involved with either the immediate or late reactions because IgE does not activate complement.
Note that the allergens involved in hypersensitivity reactions are substances, such as pollens, animal danders, foods (nuts, shellfish), and various drugs, to which most people do not exhibit clinical symptoms. However, some individuals respond to those substances by producing large amounts of IgE and, as a result, manifest various allergic symptoms. The increased IgE is the result of increased class switching to IgE in B cells caused by large amounts of interleukin (IL)-4 produced by Th-2 cells. Nonallergic individuals respond to the same antigen by producing IgG, which does not cause the release of mediators from mast cells and basophils. (There are no receptors for IgG on those cells.) There is a genetic predisposition to immediate hypersensitivity reactions, which is discussed in the “Atopy” section later.
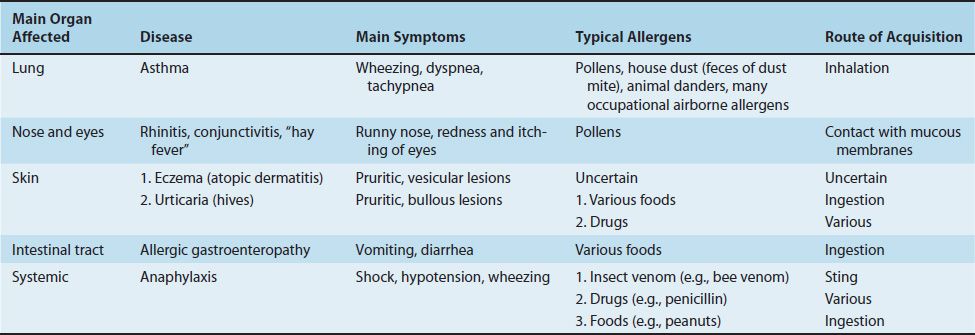
The clinical manifestations of type I hypersensitivity can appear in various forms (e.g., urticaria [also known as hives], eczema, rhinitis and conjunctivitis [also known as hay fever], and asthma). Which clinical manifestation occurs depends in large part on the route of entry of the allergen and on the location of the mast cells bearing the IgE specific for the allergen. For example, some individuals exposed to pollens in the air get hay fever, whereas others who ingest allergens in food get diarrhea. Furthermore, people who respond to an allergen with urticaria have the allergen-specific IgE on mast cells in the skin, whereas those who respond with rhinitis have the allergen-specific mast cells in the nose.
The most severe form of type I hypersensitivity is systemic anaphylaxis, in which severe bronchoconstriction and hypotension (shock) can be life-threatening. The most common causes of anaphylaxis are foods such as peanuts and shellfish, bee venom, and drugs such as penicillin. Of particular interest to medical personnel are type I hypersensitivity reactions to the wearing of latex rubber gloves, which include urticaria, asthma, and even systemic anaphylaxis. Table 65–3 summarizes some of the important clinical aspects of immediate hypersensitivities.
No single mediator accounts for all the manifestations of type I hypersensitivity reactions. Some important mediators and their effects are as follows:
(1) Histamine occurs in granules of tissue mast cells and basophils in a preformed state. Its release causes vasodilation, increased capillary permeability, and smooth muscle contraction. Clinically, disorders such as allergic rhinitis (hay fever), urticaria, and angioedema can occur. The bronchospasm so prominent in acute anaphylaxis results, in part, from histamine release. Antihistamine drugs block histamine receptor sites and can be relatively effective in allergic rhinitis but not in asthma (see later).
(2) Slow-reacting substance of anaphylaxis (SRS-A) consists of several leukotrienes, which do not exist in a preformed state but are produced during anaphylactic reactions. This accounts for the slow onset of the effect of SRS-A. Leukotrienes are formed from arachidonic acid by the lipoxygenase pathway and cause increased vascular permeability and smooth muscle contraction. They are the principal mediators in the bronchoconstriction of asthma and are not influenced by antihistamines.
(3) Eosinophil chemotactic factor of anaphylaxis (ECF-A) is a tetrapeptide that exists preformed in mast cell granules. When released during anaphylaxis, it attracts eosinophils that are prominent in immediate allergic reactions. The role of eosinophils in type I hypersensitivity reactions is uncertain, but they do release histaminase and arylsulfatase, which degrade two important mediators, histamine and SRS-A, respectively. Eosinophils may therefore reduce the severity of the type I response.
(4) Serotonin (hydroxytryptamine) is preformed in mast cells and blood platelets. When released during anaphylaxis, it causes capillary dilation, increased vascular permeability, and smooth muscle contraction but is of minor importance in human anaphylaxis.
(5) Prostaglandins and thromboxanes are related to leukotrienes. They are derived from arachidonic acid via the cyclooxygenase pathway. Prostaglandins cause dilation and increased permeability of capillaries and bronchoconstriction. Thromboxanes aggregate platelets.
(6) Platelet-activating factor (PAF) is a phospholipid produced by mast cells that can cause bronchoconstriction, hypotension, and vascular permeability.
The aforementioned mediators are active only for a few minutes after release; they are enzymatically inactivated and resynthesized slowly. Manifestations of anaphylaxis vary among species because mediators are released at different rates in different amounts, and tissues vary in their sensitivity to them. For example, the respiratory tract (bronchospasm, laryngeal edema) is a principal shock organ in humans, but the liver (hepatic veins) plays that role in dogs.
In allergic airway disease (asthma), the airway hyperactivity appears to be caused by IL-13. IL-13 is made by Th-2 cells and binds to a receptor that shares a chain with the IL-4 receptor. IL-13 does not increase the amount of IgE. Lebrikizumab, a monoclonal antibody against IL-13, reduces symptoms in some patients with severe asthma.
In contrast to anaphylactic reactions, which are IgE-mediated, anaphylactoid reactions, which appear clinically similar to anaphylactic ones, are not IgE-mediated. In anaphylactoid reactions, the inciting agents, usually drugs or iodinated contrast media, directly induce the mast cells and basophils to release their mediators without the involvement of IgE.
Atopy
Atopic disorders, such as hay fever, asthma, eczema, and urticaria, are immediate-hypersensitivity reactions that exhibit a strong familial predisposition and are associated with elevated IgE levels. Several processes seem likely to play a role in atopy, for example, failure of regulation at the T-cell level (e.g., increased production of IL-4 leads to increased IgE synthesis), enhanced uptake and presentation of environmental antigens, and hyperreactivity of target tissues. Target tissues often contain large numbers of Th-2 cells, and these are thought to play a major role in the pathogenesis of atopic reactions.
It is estimated that up to 40% of people in the United States have experienced an atopic disorder at some time in their lives. The incidence of allergic diseases, such as asthma, is increasing markedly in the developed countries of North America and Europe. One hypothesis that might explain this increase is that the parasite burden is low in those countries. IgE evolved as a host defense against parasites. In regions where the parasite burden is high, IgE is used for host defense against those organisms. But in developed regions where the parasite burden is low, IgE is available to cause allergic diseases. This is called the “hygiene” hypothesis, which states that people who live in countries with a high parasite burden have fewer allergic diseases, whereas those who live in countries with a low parasite burden have more allergic diseases.
The symptoms of these atopic disorders are induced by exposure to the specific allergens. These antigens are typically found in the environment (e.g., pollens released by plants and dust mite feces often found in bedding and carpet) or in foods (e.g., shellfish, eggs, and nuts). Exposure of nonatopic individuals to these substances does not elicit an allergic reaction. Many sufferers give immediate-type reactions to skin tests (injection, patch, or scratch) containing the offending antigen.
Atopic hypersensitivity is transferable by serum (i.e., it is antibody-mediated), not by lymphoid cells. In the past, this observation was used for diagnosis in the passive cutaneous anaphylaxis (Prausnitz-Küstner) reaction, which consists of taking serum from the patient and injecting it into the skin of a normal person. Some hours later, the test antigen, injected into the “sensitized” site, will yield an immediate wheal-and-flare reaction. This test is now impractical because of the danger of transmitting certain viral infections. Radioallergosorbent tests (RAST) permit the identification of specific IgE against potentially offending allergens if suitable specific antigens for in vitro tests are available.
There is evidence that initiation of the atopic response occurs when proteases in allergens, such as fungal allergens, pollens, and dust mite feces, cleave fibrinogen. The resulting cleavage products then activate Toll-like receptors (TLR-4) on the surface of macrophages and airway-lining cells to activate the atopic response.
Several genes associated with atopy have been identified. Mutations in the gene encoding the alpha chain of the IL-4 receptor strongly predispose to atopy. These mutations enhance the effectiveness of IL-4, resulting in an increased amount of IgE synthesis by B cells. Other genes identified include the gene for IL-4 itself, the gene for the receptor for the epsilon heavy chain, and several class II major histocompatibility complex (MHC) genes.
Drug Hypersensitivity
Drugs, particularly antimicrobial agents such as penicillin, are now among the most common causes of hypersensitivity reactions. Usually it is not the intact drug that induces antibody formation. Rather, a metabolic product of the drug, which acts as a hapten and binds to a body protein, does so. The resulting antibody can react with the hapten or the intact drug to give rise to type I hypersensitivity.2
When reexposed to the drug, the person may exhibit a drug rash, fever, or local or systemic anaphylaxis of variable severity. Reactions to very small amounts of the drug can occur (e.g., in a skin test with the hapten). A clinically useful example is the skin test using penicilloyl polylysine to reveal an allergy to penicillin.
Desensitization
Major manifestations of anaphylaxis occur when large amounts of mediators are suddenly released as a result of a massive dose of antigen abruptly combining with IgE on many mast cells. This is systemic anaphylaxis, which is potentially fatal. Desensitization can prevent systemic anaphylaxis.
Acute desensitization involves the administration of very small amounts of antigen at 15-minute intervals. Antigen–IgE complexes form on a small scale, and not enough mediator is released to produce a major reaction. This permits the administration of a drug or foreign protein to a hypersensitive person, but the hypersensitive state returns because IgE continues to be made.
Chronic desensitization involves the long-term weekly administration of the antigen to which the person is hypersensitive. This stimulates the production of IgA-and IgG-blocking antibodies, which can prevent subsequent antigen from reaching IgE on mast cells, thus preventing a reaction. It also induces regulatory T cells to produce IL-10, which reduces the synthesis of IgE.
Treatment & Prevention
Treatment of anaphylactic reactions includes drugs to counteract the action of mediators, maintenance of an airway, and support of respiratory and cardiac function. Epinephrine, antihistamines, corticosteroids, or cromolyn sodium, either singly or in combination, should be given. Cromolyn sodium prevents release of mediators (e.g., histamine) from mast cell granules. Prevention relies on identification of the allergen by a skin test and avoidance of that allergen.
There are several approaches to the treatment of asthma. Inhaled β-adrenergic bronchodilators, such as albuterol, are commonly used. Corticosteroids, such as prednisone, are also effective. Aminophylline, a bronchodilator, is effective but not commonly used. A monoclonal anti-IgE antibody (omalizumab, Xolair) is indicated for patients with severe asthma whose symptoms are not controlled by corticosteroids. For the prevention of asthma, leukotriene receptor inhibitors, such as montelukast (Singulair), and cromolyn sodium are effective.
The treatment of allergic rhinitis typically involves antihistamines along with nasal decongestants. For allergic conjunctivitis, eye drops containing antihistamines or vasoconstrictors are effective. Avoidance of the inciting allergens, such as pollens, is helpful in prophylaxis. Desensitization can also be helpful.
TYPE II: CYTOTOXIC HYPERSENSITIVITY
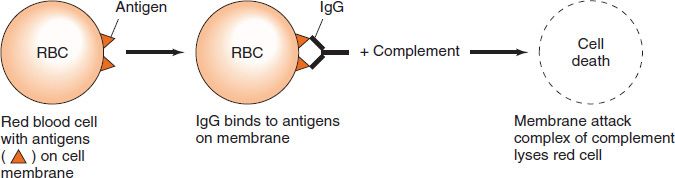
Cytotoxic hypersensitivity occurs when antibody directed at antigens of the cell membrane activates complement (Figure 65–2). This generates a membrane attack complex (see Chapter 63), which damages the cell membrane. The antibody (IgG or IgM) attaches to the antigen via its Fab region and acts as a bridge to complement via its Fc region. As a result, there is complement-mediated lysis as in hemolytic anemias, ABO transfusion reactions, or Rh hemolytic disease. In addition to causing lysis, complement activation attracts phagocytes to the site, with consequent release of enzymes that damage cell membranes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree