Human Immunodeficiency Virus Lymphadenitis
Tariq Muzzafar, MBBS
Key Facts
Terminology
Human immunodeficiency virus (HIV)
Lymphadenitis caused by HIV infection
Clinical Issues
History of high-risk exposure should be sought
Microscopic Pathology
Histologic findings can be divided into stages
Florid follicular hyperplasia
Irregularly shaped follicles, attenuation of mantle zones, follicle lysis, hemorrhage
Mixed pattern
Transitional stage
Follicular involution
Small, hypocellular, hyalinized follicles
Expanded paracortical regions
Moderate lymphocyte depletion, plasmacytosis, vascular proliferation
Lymphocyte depletion
Predominantly medullary cords and sinusoids
Marked lymphocyte depletion with absence of follicles and paracortical areas
Predominance of histiocytes and plasma cells; subcapsular and sinusoidal fibrosis
Histologic changes partially reversed by HAART
Top Differential Diagnoses
Other causes of acute lymphadenitis
Infectious mononucleosis (EBV+)
Castleman disease, hyaline-vascular variant
AIDS-related lymphomas
Non-Hodgkin lymphoma
Hodgkin lymphoma
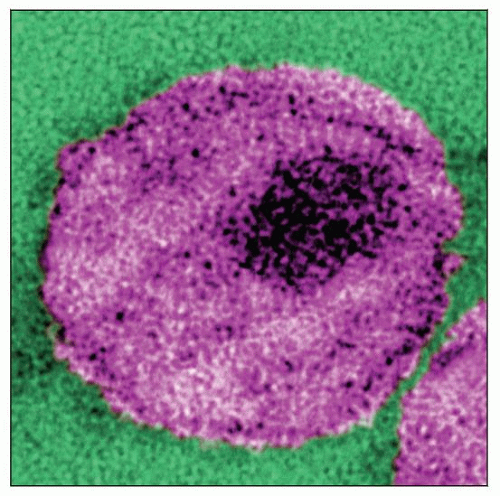 Thin section transmission electron micrograph of HIV. The viral core is the dark area in the center. (Courtesy A. Harrison, P. Feorino, CDC Public Health Image Library, #10860). |
TERMINOLOGY
Abbreviations
Human immunodeficiency virus (HIV)
Synonyms
Acquired immune deficiency syndrome (AIDS) lymphadenitis
HIV lymphadenopathy
Definitions
Lymphadenitis caused by HIV infection
ETIOLOGY/PATHOGENESIS
Infectious Agents
HIV-1 underwent single cross-species transmission from chimpanzees to humans 100 years ago
Virus diversified in humans into many genetic subtypes: A-D
Most sexually transmitted HIV infections are initiated by a single variant
Initial target cells are CD4(+) T cells
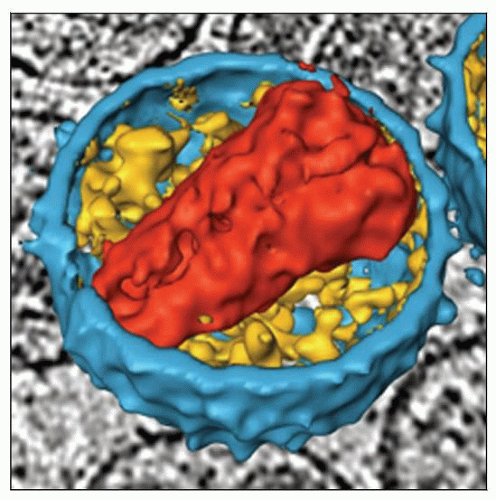
HIV, a retrovirus belonging to the lentivirus family has
9 genes
2 copies of single-stranded RNA in core
Reverse transcriptase generates double-stranded DNA copy that integrates into host genome
Covalently forms a provirus
Provirus can remain latent or be highly expressed, forming progeny viruses
Icosahedral structure with 72 external spikes composed of envelope proteins gp120 and gp41
Crucial for cell attachment and entry
HIV has tropism for CD4(+) T cells, monocytes, and follicular dendritic cells
gp120 binds with CD4 receptor and subsequently with chemokines CR5 and CXCR4
Leads to fusion of viral and cellular membranes and internalization of viral complex
4 nucleocapsid proteins: p24, p17, p9, and p7
Pathogenesis of HIV Lymphadenopathy
High HIV antigen density, marked inflammation, and adhesion molecule expression by lymphocytes
Leads to lymphocyte sequestration
Exposure to increased cytokine levels results in lymphocyte death
Prolonged inflammation leads to fibrosis resulting in
Disrupted maturation of T cells
Decreased naive circulating CD4(+) T cells
Follicular dendritic cells in germinal centers entrap HIV
CLINICAL ISSUES
Epidemiology
Incidence
2.7 million new HIV infections per year in 2007 globally
Prevalence is stable at 0.8%
33.2 million people have HIV infection or AIDS
2 million deaths per year related to AIDS
Age
Patients 15-24 years old represent 45% of new HIV infections globally
Estimated 370,000 children < 14 years old were infected in 2007
2 million children with HIV
Gender
No sex preference; stable globally
Ethnicity
Sub-Saharan Africa accounts for 67% of total people and 90% of children living with HIV
Predominantly heterosexual transmission in general population
Accounts for 75% of AIDS-related deaths
Asia overall has shown a trend toward a decrease in new HIV infections and an increase in AIDS-related deaths
National trends vary considerably
Recreational drug use, commercial sex work, and male-male sex are major factors in transmission
Eastern Europe and Central Asia have shown a rising trend in number of people living with HIV infection
Number of new infections has been slowing
Recreational drug use and commercial sex work are major factors in transmission
Western and Central Europe show stable trends
Heterosexual transmission is major mode of transmission
Caribbean basin, South and North America show stable trends
Male-male sex is major mode of transmission, followed by heterosexual transmission
Number of persons living with HIV infection has increased as result of therapy
Presentation
Acute (primary) phase of HIV infection
Can present as flu-like or mononucleosis type of syndrome with nonspecific symptoms
Findings: Fever, lymphadenopathy, skin rash, myalgia, arthralgia, headache, diarrhea, oral ulcers
Clinical diagnosis of acute HIV infection can be challenging
Usually lasts several weeks
Opportunistic infections can occur during transient CD4 lymphopenia
Most common: Oral and esophageal candidiasis
Chronic phase of HIV infection is characterized by dysregulated or suppressed immunity
HIV infection can generally be latent for a number of years
Eventually patients develop symptoms and abnormalities related to low CD4(+) count
Polyclonal hypergammaglobulinemia
Altered levels of cytokines (e.g., IL-6, TNF-α) and activation markers (e.g., CD38 on T cells)
Opportunistic infections: Mycobacterium tuberculosis, Pneumocystis jiroveci (formerly known as P. carinii)
Neoplasms: Lymphomas, Kaposi sarcoma
˜ 50% of HIV(+) patients with lymphadenopathy are asymptomatic
Usually, lymph node biopsy shows follicular hyperplasia
Laboratory Tests
Acute (primary) phase of HIV infection
Leukopenia, thrombocytopenia, elevated serum transaminase level
Viremia at high titers; CD4(+) T cells and monocytes infected
3rd generation enzyme immunoassays used in clinical practice and in blood banks in USA do not detect HIV antibodies until 3-7 weeks after infection
Chronic phase of HIV infection
Drop in CD4(+) counts to < 200/mm3
Findings related to specific opportunistic infections
Diagnosis of acute infection is established by demonstrating
High viral load
p24 antigen in patient with typical clinical features and negative or indeterminate HIV serologic test
Serologic testing
Based on detection of IgG against HIV antigens in serum
p24, a nucleocapsid protein
gp120 and gp41, envelope proteins
Centers for Disease Control (CDC) criteria for positive serology include
Antibodies to gp120 plus antibodies to either gp41 or p24
Antibodies to gp41 and p24 antigens are 1st detectable serologic markers following HIV infection
IgG antibodies appear 6-12 weeks following infection in most patients (by 6 months in 95%)
Antibodies persist for life
Results are reported as positive, negative, or indeterminate
Criteria for a positive test: Repeatedly positive enzyme immunoassay test followed by a positive Western blot analysis
Positive test should be confirmed by repeat testing or corroborating laboratory data
Accuracy of HIV serologic testing is high
99.3% sensitivity and 99.7% specificity according to CDC survey
Rapid tests can be done at point of care and read by provider
High diagnostic accuracy comparable to standard serological tests and much cheaper
Results can be available in minutes
Treatment
Drugs
Highly active antiretroviral therapy (HAART)
Increases disease-free survival by suppressing viral replication and improving immunologic function
Indications for HAART
History of AIDS-defining illness, CD4 count < 350 cells/mm3, pregnant women, and HIV-associated nephropathy
Syndrome resembling primary HIV infection occurs in patients 2-4 weeks after HAART is discontinued
Fever, lymphadenopathy, and rash; plasma viremia rises and CD4(+) counts fall
Prognosis
HIV infection can be indolent for years but will eventually become lethal without HAART
Lymph nodes in HIV(+) patients show histologic progression without therapy, from follicular hyperplasia to lymphocyte depletion
Lymph node biopsy findings in HIV(+) patients correlate, in part, with outcome
Patients with follicular hyperplasia or mixed pattern have
Longer survival
Lower incidence of opportunistic infections
Patients with lymphocyte depletion have very poor prognosis
HIV(+) patients have increased risk of non-Hodgkin and Hodgkin lymphoma
HAART has reduced risk of non-Hodgkin lymphoma but not Hodgkin lymphoma
MACROSCOPIC FEATURES
General Features
Enlarged lymph nodes in follicular hyperplasia
Small, shrunken lymph nodes in lymphocyte depletion
Often not biopsied but detected at autopsy
MICROSCOPIC PATHOLOGY
Histologic Features
Florid (explosive) follicular hyperplasia
Markedly hyperplastic lymphoid follicles in cortex and medulla
Follicles with irregular shapes (e.g., serpiginous)
Attenuated mantle zones
Follicle lysis, often associated with hemorrhage
Hyperplastic germinal centers: Mitoses, apoptosis, tingible body macrophages (“starry sky”)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree