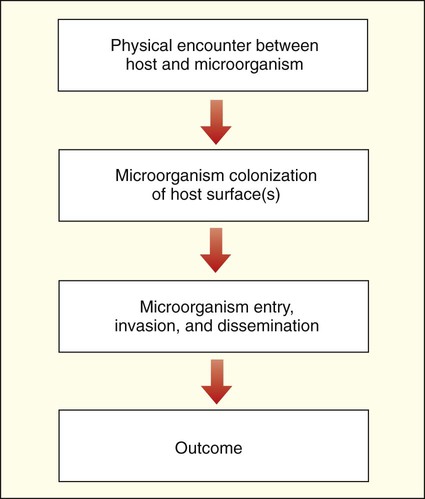
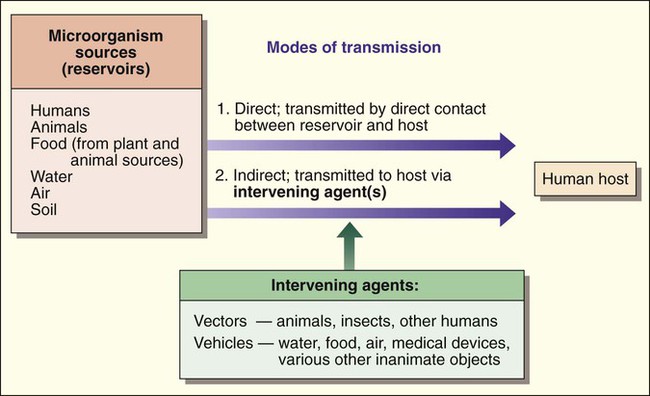
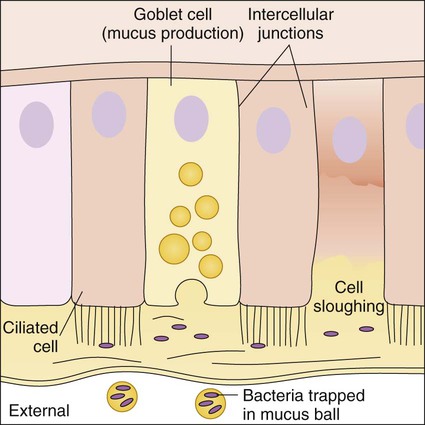
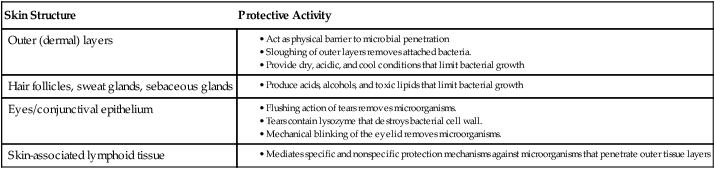
1. List the various reservoirs (environments) that facilitate host-microorganism interactions. 2. Define direct versus indirect transmission and provide examples of each. 3. Define and differentiate the interactions between the host and microorganism, including colonization, infection, normal (resident) flora, pathogens, opportunistic pathogens, and nosocomial infection. 4. List and describe the components involved in specific versus nonspecific immune defenses, including inflammation, phagocytosis, antibody production, and cellular responses. 5. Identify elements involved in the two arms of the immune system: humoral and cell-mediated immunity. 6. Provide specific examples of disease prevention strategies, including preventing transmission, controlling reservoirs and minimizing risk of exposure. 7. Differentiate between bacterial endotoxins and exotoxins and provide examples of each. 8. Given a patient history of an infectious process, identify and differentiate a sign versus a symptom. 9. Define and differentiate between an acute infectious process and one that is chronic and/or latent. Interactions between humans and microorganisms are exceedingly complex and far from being completely understood. What is known about the interactions between these two living entities plays an important role in the practice of diagnostic microbiology and in the management of infectious disease. Understanding these interactions is necessary for establishing methods to reliably isolate specific microorganisms from patient specimens and for developing effective treatment strategies. This chapter provides the framework for understanding the various aspects of host-microorganism interactions. Box 3-1 lists a variety of terms and definitions associated with host-microorganism interactions. The complex relationships between human hosts and medically relevant microorganisms are best understood by considering the sequential steps in the development of microbial-host associations and the subsequent development of infection and disease. The stages of interaction (Figure 3-1) include (1) the physical encounter between host and microorganism; (2) colonization or survival of the microorganism on an internal (gastrointestinal, respiratory, or genitourinary tract) or external (skin) surface of the host; (3) microbial entry, invasion, and dissemination to deeper tissues and organs of the human body; and (4) resolution or outcome. Humans encounter microorganisms when they enter or are exposed to the same environment in which the microbial agents live or when the infectious agents are brought to the human host by indirect means. The environment, or place of origin, of the infecting agent is referred to as the reservoir. As shown in Figure 3-2, microbial reservoirs include humans, animals, water, food, air, and soil. The human host may acquire microbial agents by various means referred to as the modes of transmission. The mode of transmission is direct when the host directly contacts the microbial reservoir and is indirect when the host encounters the microorganism by an intervening agent of transmission. The agents of transmission that bring the microorganism from the reservoir to the host may be a living entity, such as an insect, in which case they are called vectors, or they may be a nonliving entity, referred to as a vehicle or fomite. Additionally, some microorganisms may have a single mode of transmission, whereas others may spread by various methods. From a diagnostic microbiology perspective, knowledge about an infectious agent’s mode of transmission is often important for determining optimum specimens for isolation of the organism and for implementing precautions that minimize the risk of laboratory-acquired infections (see Chapters 4 and 80 for more information regarding laboratory safety). Once a microbe and the human host are brought into contact, the outcome of the encounter depends on what happens during each step of interaction (see Figure 3-1), beginning with colonization. The human host’s role in microbial colonization, defined as the persistent survival of microorganisms on a surface of the human body, is dictated by the defenses that protect vital internal tissues and organs against microbial invasion. The first defenses are the external and internal body surfaces that are in direct contact with the external environment and are the anatomical regions where the microorganisms will initially come in contact with the human host. These surfaces include: • Skin (including conjunctival epithelium covering the eye) • Mucous membranes lining the mouth or oral cavity, the respiratory tract, the gastrointestinal tract, and the genitourinary tract Skin serves as a physical and chemical barrier to microorganisms; its protective characteristics are summarized in Table 3-1 and Figure 3-3. The acellular, outermost layer of the skin, along with the tightly packed cellular layers underneath, provide an impenetrable physical barrier to all microorganisms, unless damaged. Additionally, these layers continuously shed, thus dislodging bacteria that have attached to the outer layers. The skin is also a dry and cool environment; this is incompatible with the growth requirements of many microorganisms, which thrive in a warm, moist environment. TABLE 3-1 Protective Characteristics of the Skin and Skin Structures Because cells that line the respiratory tract, gastrointestinal tract, and genitourinary tract are involved in numerous functions besides protection, they are not covered with a hardened, acellular layer as is the skin surface. However, the cells that compose these membranes still exhibit various protective characteristics (Table 3-2 and Figure 3-4). TABLE 3-2 Protective Characteristics of Mucous Membranes Besides the general protective properties of mucosal cells, the mucosal linings throughout the body have characteristics specific to each anatomic site (Figure 3-5). In the upper respiratory tract, nasal hairs keep out large airborne particles that may contain microorganisms. The cough-sneeze reflex significantly contributes to the removal of potentially infective agents. The cells lining the trachea contain cilia (hairlike cellular projections) that move microorganisms trapped in mucus upward and away from the delicate cells of the lungs (see Figure 3-4); this is referred to as the mucociliary escalator. These barriers are so effective that only inhalation of particles smaller than 2 to 3 µm have a chance of reaching the lungs. As previously discussed, microorganisms that inhabit many surfaces of the human body (see Figure 3-5) are referred to as colonizers, or normal flora (also referred to as normal microbiota). Some are transient colonizers, because they are able to survive, but do not multiply, on the surface and are frequently shed with the host cells. Others, called resident flora, not only survive but also thrive and multiply; their presence is more persistent. Colonization may be the last step in the establishment of a long-lasting, mutually beneficial (i.e., commensal), or harmless, relationship between a colonizer and the human host. Alternatively, colonization may be the first step in the process for the development of infection and disease. Whether colonization results in a harmless or damaging infection depends on the characteristics of the host and the microorganism. In either case, successful initial colonization depends on the microorganism’s ability to survive the conditions first encountered on the host surface (Box 3-2). Besides surviving the host’s physical and chemical conditions, colonization also requires that microorganisms attach and adhere to host surfaces (see Box 3-2). This can be particularly challenging in places such as the mouth and bowel, in which the surfaces are frequently washed with passing fluids. Pili, the rodlike projections of bacterial envelopes, various molecules (e.g., adherence proteins and adhesins), and biochemical complexes (e.g., biofilm) work together to enhance attachment of microorganisms to the host cell surface. Biofilm is discussed in more detail later in this chapter. (For more information concerning the structure and functions of pili, see Chapter 2.)
Host-Microorganism Interactions
The Encounter Between Host and Microorganism
The Human Host’s Perspective
Microbial Reservoirs and Transmission
Microorganism Colonization of Host Surfaces
The Host’s Perspective
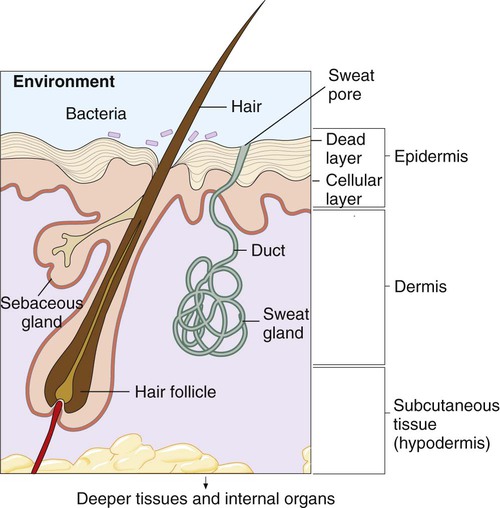
Skin and Skin Structures
Skin Structure
Protective Activity
Outer (dermal) layers
Hair follicles, sweat glands, sebaceous glands
Eyes/conjunctival epithelium
Skin-associated lymphoid tissue
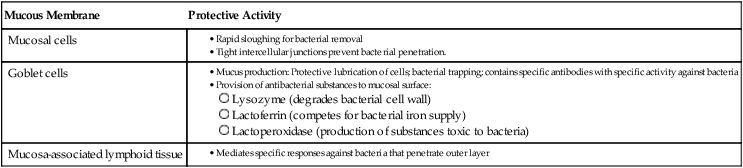
Mucous Membranes
Mucous Membrane
Protective Activity
Mucosal cells
Goblet cells
Mucosa-associated lymphoid tissue
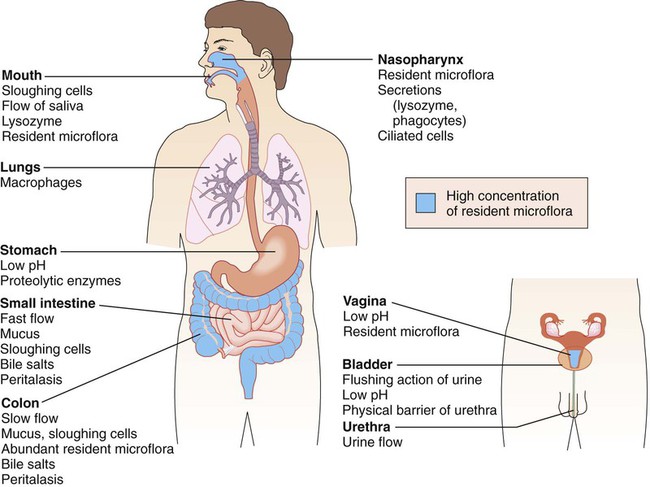
Specific Protective Characteristics.
The Microorganism’s Perspective
Microbial Colonization
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Host-Microorganism Interactions