Homeostasis and Adaptive Responses to Stressors
Debra A. Jansen and Roberta J. Emerson
Key Questions
• What is the relationship between homeostasis and allostasis?
• How do the sympathetic nervous system and neuroendocrine system respond to stress?
• What are the key features of Selye’s General Adaptation Syndrome?
• What factors affect the stress response?
• How does allostatic overload contribute to the development of disease?
![]()
http://evolve.elsevier.com/Copstead/
Survival of the human species is dependent on its ability to respond to changes in the environment. Changes in the external environment, such as moving outside from a warm house on a cold winter day, demand physiologic adjustments in the body’s internal environment beyond the simple addition of layers of clothing to the outside of the body. Variations in the internal environment, such as a fever caused by infection, also necessitate physiologic responses to return the body’s temperature to the normal range. The human organism maintains a variety of highly complex interactions with both internal and external environments. These interactions facilitate ongoing compensatory changes designed to support the organism physically and psychologically. This process is necessary, allowing the perpetuation of both the individual and the species. Researchers, however, have found that the body’s efforts to adapt to prolonged and repeated or extraordinarily demanding environmental changes may be associated with many physical and psychological health problems. This chapter explores the historical and current perspectives of homeostasis, allostasis, and stress responses, and their relationship to illness.
Homeostasis and Allostasis
Homeostasis
The word homeostasis is derived from the Greek words homeo, or same, and stasis, or stable, and means remaining stable by remaining the same.1 Homeostasis is conceptualized as a state of being in which all systems are in balance around a particular ideal “set-point.” From this perspective, bodily changes formerly seen as conflicting or detrimental are understood as adaptive or compensatory to the maintenance of homeostasis within the body as a whole. Homeostasis reflects a tendency to stabilize an organism’s functional systems, despite changes both internally and externally. Deviations from homeostasis resulting from these changes require elaborate systems to support its reestablishment. A great deal of discussion exists in the literature over the past several decades criticizing the inadequacy of the definition of homeostasis to encompass the entire process of maintaining a stable state in complex organisms. But the fact remains that homeostatic concepts are an essential starting point for an exploration of stress, adaptation, and disease.
Claude Bernard, a nineteenth century French physiologist, is credited with describing the basic premise of homeostasis. He believed that the various vital physiologic mechanisms of the body had as their goal the maintenance of a uniform and constant internal environment, or milieu intérieur, for the body. The stability of the internal environment was deemed necessary for the survival of the person, independent or free of the external environment.1,2 Disease occurred when the body did not respond appropriately to maintain internal stability when threatened by perceived or actual events.1 Building on Bernard’s work, Walter B. Cannon created a concept that he referred to as “homeostasis” in his 1932 book The Wisdom of the Body.1–4 Homeostasis, according to Cannon, was a process in which each of the body’s biochemical or physiologic variables (e.g., body temperature; oxygen, sodium, calcium, and glucose levels; and pH) was maintained within a narrow set point range. Negative feedback loops were used to sense and correct any deviations from the set point ranges for the variables, thereby supporting the survival of the individual, despite threats from the external or internal environments. These environmental threats could range from temperature extremes and water loss or gain, to “savage animals,” to bacterial infection.1,3 Box 2-1 provides examples of homeostatic systems designed to support the life of the person in the most basic sense.
Allostasis
The original concept of homeostasis, with the principle that the body attempts to achieve balance around a single optimal level or set point for a given physiologic variable, has been challenged in recent decades. The innate complexity of biological organisms requires that set points be readjusted for different circumstances (i.e., diverse situations necessitate different homeostatic set points).5 For example, respiratory rate needs to increase when vigorously exercising or when ill with pneumonia in order to obtain more oxygen. At the same time, when responding to an internal or external environmental challenge (i.e., a stressor), multiple physiologic parameters may have to raise or lower their levels or actions in order to meet the demands posed by the challenge and achieve some internal stability. Desired changes in one body system, though, may be detrimental to another; these changes, however, may ultimately be needed to support the survival of the organism as a whole at that particular point in time.5 For instance, in shock, when the life of the organism is at risk, blood flow to essential organs (brain and heart) is maintained by reducing perfusion to the kidneys, skin, and gastrointestinal tract. Simply stated, the body is not concerned about digesting dinner or making urine when it is trying to divert resources to a struggling brain and heart.
In 1988 Sterling and Eyer introduced the concept of allostasis in recognition of the complexity and variable levels of activity necessary to reestablish or maintain homeostasis.6 They described allostasis as the ability to successfully adapt to challenges. In order to survive, “an organism must vary all the parameters of its internal milieu and match them appropriately to environmental demands.” Like homeostasis, allostasis is a derivation of the Greek words allo, meaning variable, and stasis, meaning stable. Therefore this term accentuates the role of allostatic systems in maintaining the organism’s stability by being variable.1 Allostasis is a dynamic process that supports and helps the body achieve homeostasis; homeostasis, from this perspective, is seen as a steady-state. In essence, the organism’s overall stability is accomplished through change.1,7
Allostasis involves intricate regulatory processes orchestrated by the brain.8 Through these processes, the body’s parameters are continuously reevaluated and readjusted in order to match resources to the needs dictated by the situation. These parameter readjustments (e.g., of heart rate, blood pressure, or glucose levels) entail altering multiple set points such that the person may be functioning at reduced or elevated levels or rates for numerous physiologic variables. Thus, an individual may have different set points for different circumstances (e.g., when resting versus running or when healthy versus sick). Allostasis comes into play in the complexity of social interactions, during changes in the weather, during reproduction, and even in the hibernation and migration patterns of bears and birds, as well as in critical illness.1,6,7,9 Although the concept is occasionally challenged,7,10 it has garnered broad support in both the physical and the behavioral sciences. It seems especially applicable to subsequent discussions of adaptation and disease.
Stress as a Concept
Referring to stress as something of an “ambiguous” term is an understatement. Its ubiquitous use in everyday parlance is matched by its frequent presence in the health and psychology literature. Stress often is interpreted as a physical, chemical, or emotional factor that produces tension in the body or the mind (“He’s experiencing a lot of stress”). But it also can mean the actual physical and mental state of tension (“I feel stressed”). Others use the term stress in relation to the response by the body to internal and external demands. Stress can be defined as a real or perceived threat to the balance of homeostasis. The neuroendocrinologist Robert Sapolsky more specifically distinguishes between the stress terminology and defines a stressor as anything that throws the body out of allostatic balance, whereas the stress response is the body’s effort to try to restore the balance. To that end, stress is a natural outgrowth of the concept of homeostasis but is even more applicable to the dynamic concept of allostasis. Sapolsky’s5 definition also underscores an important point: The stress response by the body is meant to be helpful, at least in the short term; however, it becomes damaging when repeatedly activated or when it does not cease.
As early as the 1920s, Walter Cannon used the term stress in relation to humans and medicine. Hans Selye, however, often is erroneously credited with being the first person to borrow the term from the fields of engineering and physics and apply it to the human condition.5 In the 1930s Selye was experimenting with assorted ovarian and placental hormonal preparations and other tissue extracts and toxic agents. He was injecting these into rats when he serendipitously uncovered a biological basis for stress.1,5,11 Selye was expecting to find different physiologic responses in the rats, depending on which of the various substances was injected; however, to his surprise and disappointment, the same three changes occurred each time. In every animal tested, the cortex of the adrenal gland enlarged, lymphatic organs (thymus, spleen, and lymph nodes) shrank, and bleeding peptic ulcers developed in the stomach and duodenum. When Selye experimented with other noxious stimuli, such as exposing the rats to temperature extremes, surgery, or forced exercise, the same three changes occurred. Any kind of harmful physical stimuli he used produced the same observed physiologic changes. Selye termed the harmful stimuli or causative agents stressors and concluded that the changes observed represented a nonspecific response by the body to any noxious stimulus or demand, a general “stress” response.11 Because so many different agents caused the same changes, Selye called this process a general adaptation syndrome (GAS) with three components: an alarm reaction, a stage of resistance, and a stage of exhaustion.1,5,11 According to Selye, when confronted by stressors during daily life, individuals move through the first two stages repeatedly and eventually become adapted and “used to” the stressors.11
Selye’s original conceptualization of the stress response and GAS has been criticized as being too simplistic for the complexities of humans. In particular, evidence suggests the body does not produce the same responses to all types of stressors. Depending on the type and severity of stressor, different patterns of hormone release occur, with more of some substances and less of others being produced and at different speeds and for varying lengths of time.5,12 Moreover, Selye’s early work in the 1930s concentrated on stimuli of a physical or biological nature.11 Beginning in the 1970s, researchers began to realize that perception of these stimuli was important to individuals’ responses to stress, and that responses could be physiologic, as Selye described, as well as behavioral in nature. When stress is generated by extreme psychological or environmental demands, balance is disrupted, and allostatic reactions are initiated to restore balance.13 The discussion that follows presents the GAS as a reflection of the responses to these diverse stimuli and incorporates much of the knowledge acquired since Selye’s early pioneering work.
The General Adaptation Syndrome and Allostasis
Components of the GAS can be subdivided into three unique, largely physiologic stages (Table 2-1). Examining the stages separately is the best way to understand the entire GAS. The specific chemicals involved are among those seen today as integral to the broader view of allostatic responses to stress in the maintenance of homeostasis. All will be discussed later in the chapter.
TABLE 2-1
STAGES OF THE GENERAL ADAPTATION SYNDROME
| ALARM | RESISTANCE | EXHAUSTION |
| Increased secretion of glucocorticoids and responses | Eventual normalization of glucocorticoid secretion | Increased glucocorticoid secretion followed by significant reduction |
| Increased sympathetic nervous system activity | Eventual normalization of sympathetic nervous system activity | Diseases of adaptation |
| Increased secretion of epinephrine (and some norepinephrine) from adrenal medulla | Eventual normalization of epinephrine and norepinephrine secretion from adrenal medulla | Loss of resistance to stressor; possible death of organism |
| Fight-or-flight manifestations | Resolution of fight-or-flight manifestations | |
| Reduced resistance to stressors | Increased resistance (adaptation) to stressor |
Alarm Stage
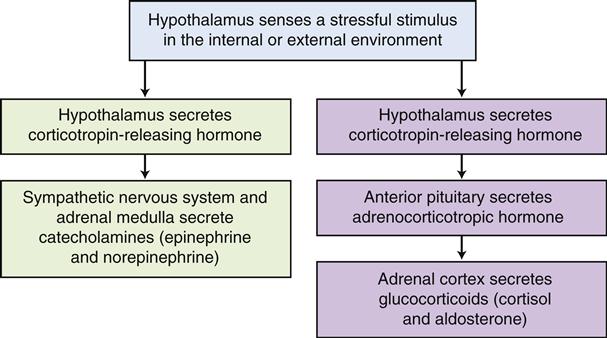
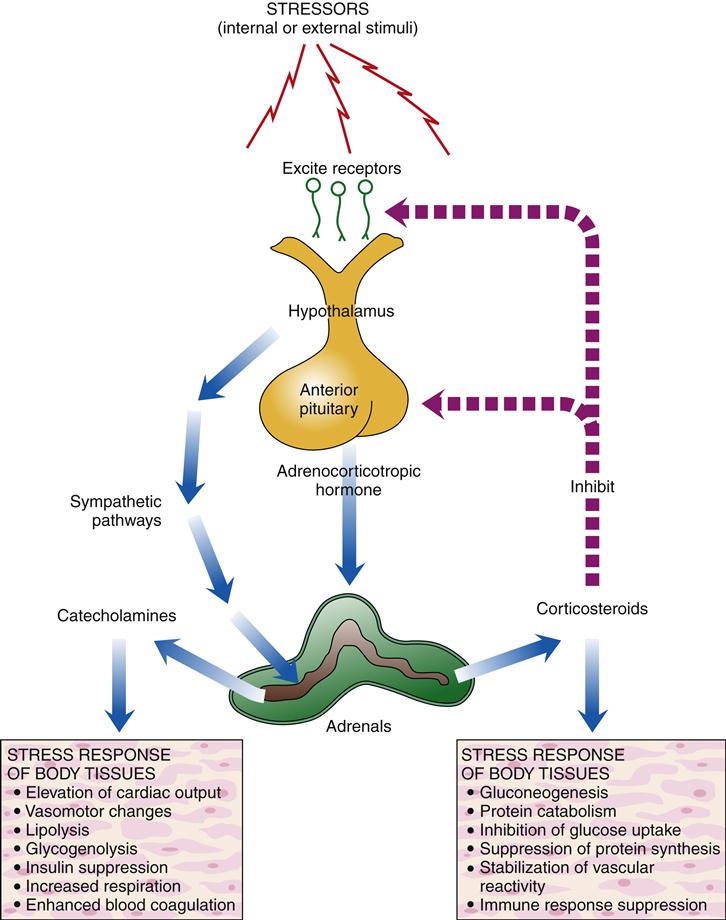
The alarm stage has been called the fight-or-flight response, derived from Cannon’s work, because it provides a surge of energy and physical alterations to either evade or confront danger12 (Figure 2-1). This stage begins when the hypothalamus, as it monitors the internal and external environment, senses a need to activate the GAS in response to a stimulus, a stressor placing the balance of homeostasis at risk. The stressor might be physical or emotional, positive or negative—arguing with a friend, having an upper respiratory tract infection, running to catch a bus, or winning the lottery. The hypothalamus then secretes corticotropin-releasing hormone (CRH) to activate the sympathetic nervous system, which in turn also stimulates the adrenal medulla (the inner portion of the adrenal gland) to release the catecholamines—norepinephrine and epinephrine. The increased levels of catecholamines enable the body to rapidly take action to fight or flee the stressor. This series of events is part of the sympathetic-adrenal-medullary system, originally referred to as the fight-or-flight response by Walter Cannon. Additionally, the hypothalamus secretes CRH to also stimulate the anterior pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH then causes the adrenal cortex (the outer portion of the adrenal gland) to release substantial amounts of the glucocorticoids, specifically cortisol, eliciting its diverse responses, and also aldosterone. This cascade of effects is termed the hypothalamic-pituitary-adrenal (HPA) axis.4 Once the pituitary gland is activated, the alarm stage progresses to the stage of resistance. This coordinated systemic response to stress is illustrated in Figure 2-2.
Allostasis is essentially the activation of these stress responses to evoke changes that return the organism to homeostasis. Mediators of allostasis include the aforementioned hormones, neurotransmitters of the HPA axis and the sympathetic-adrenal-medullary system (e.g., cortisol, epinephrine, and norepinephrine),1,8,9 various other hormones presented later in this chapter, and also cytokines from the immune system. The alarm stage of the stress response with the release of its various hormones is meant to be helpful to the organism in overcoming the stressor, at least initially.
Resistance or Adaptation Stage
If the alarm stage were to persist, the body would soon suffer undue wear and tear and become subject to permanent damage and even death.11 To survive, the body must move beyond the alarm stage to a stage of resistance (also called adaptation) supportive of the allostatic return to a state of homeostasis. As the body moves into the stage of resistance, the sympathetic nervous system and adrenal medulla and cortex are functioning at full force to mobilize resources to manage the stressor. The resources include glucose, free fatty acids, and amino acids, and concentrations of all of these chemicals are elevated through the effects of cortisol and the catecholamines (i.e., epinephrine and norepinephrine). These resources are used for energy and as building blocks, especially the amino acids, for the later growth and repair of the organism after the stress abates. If the stressor is adequately addressed and resolved, the organism returns to its steady-state, having reattained allostatic balance.5 This process described by Selye is clearly a part of the more recently described process of allostasis. However, with the current understanding of allostasis, it is possible that in order to adapt and reattain homeostasis, the organism may have to function at a new baseline steady-state for different physiologic variables, either higher or lower than the previous set points. For instance, the normal partial pressure of carbon dioxide (pCO2) in the blood is 35 to 45 mm Hg and the normal oxygen saturation is greater than 94% in a healthy individual. For someone with chronic obstructive pulmonary disease, a new normal pCO2 value might be 50 to 60 mm Hg and the oxygen saturation may be 88% to 90%, while still maintaining a homeostatically normal serum pH.
Exhaustion Stage
Exhaustion occurs when the body is no longer able to effect a return to homeostasis following prolonged exposure to noxious agents.11 Selye postulated that when energy resources are completely depleted, death occurs because the organism is no longer able to adapt. He speculated that individuals are born with a given amount of adaptation energy. However, when these adaptive energy stores are depleted, no other resource exists to facilitate recovery. Diseases of adaptation such as hypertension and heart disease occur when the body is continuously taxed by stressors.11 It is now understood that exhaustion and stress-related disease do not necessarily occur because resources are depleted; instead, they can occur because the actual stress response itself, with all of its various biological mediators, can be harmful when repeatedly activated.5
Concepts related to allostasis help with understanding the damaging effects of stress. The HPA axis, the sympathetic-adrenal-medullary system, and other systems (including the immune system) work to help the person adapt to and defend against stressors. Wear and tear on the body and on the brain occurs when these body systems are chronically over- or underactivated in their attempts to support an allostatic return to homeostasis. The accumulation of all of the various mediators produced by the systems is damaging to tissues over time. This wear and tear on the body and brain is called allostatic load.4,8,9 Allostatic load is basically due to the typical demands that are part of daily life as well as unpredictable events. However, with chronic, unremitting, or excessive demands, allostatic load can become an overload. This allostatic overload reflects the “cost” to the body’s organs and tissues for an allostatic response that is excessive or ineffectively regulated and unable to deactivate.1,7,14 It is essentially a re-envisioning of the effect of wear and tear on the body, both acutely and chronically, and is a more useful definition than homeostasis in discussions of pathophysiology.
Stressors and Risk Factors
Stressors are agents or conditions that are capable of producing stress and endangering homeostasis. They initiate stress response systems in order to return to a state of allostatic balance. Every day the human organism encounters stressors. These may be external to the individual (e.g., air pollution, radiation, a motor vehicle accident) or internal (e.g., low blood glucose level or a threat to self-esteem). Common general stressors are physical (e.g., extreme hot or cold air temperature), chemical (e.g., auto exhaust), biological (e.g., bacteria and viruses), social (e.g., overcrowding and relationships), cultural (e.g., behavioral norms), or psychological (e.g., feelings of hopelessness). Stressors of an emotional or mental origin may be actually present or anticipated, or may involve the recollection of prior traumatic events. Less commonly noted but extremely powerful stressors are psychosocial experiences over which a person may have little or no personal control. Racial15–18 and socioeconomic stressors8,19–21 as well as childhood abuse22 can produce many of the manifestations of stress described in this chapter.
Stressors vary in their scope, intensity, and duration. A stressor of less intensity can still have a significant impact if it persists for some time. A glass of water held at arm’s length poses little stress initially, but as minutes turn into hours the stress on the body escalates. Even events associated with happiness may serve as stressors—holidays, childbirth, and vacations. Stressors of all types challenge human adaptation.
The identification of specific stressors in isolation provides little insight into today’s complex global society. As noted by Sapolsky,5 a given stressor may have its own particular pattern of hormone release; however, researchers have explored innumerable factors that can indirectly increase or decrease the impact of stressors. It is now generally well accepted that inherent personal characteristics as well as the psychological context of the situation allow for a great deal of variation in the way humans perceive and respond to stressors, and thus the type of stress response produced.4,5 The activation of both the sympathetic-adrenal-medullary system response and the HPA axis occurs with a wide variety of physical, mental, and psychosocial stressors. The HPA axis with its glucocorticoid response, however, seems to be notably prominent and dysregulated in cases of depression and posttraumatic stress disorder, and is also active when a person’s sense of self is negatively evaluated or the person lacks a sense of control.5,23 On the other hand, the sympathetic system is particularly active with anxiety and vigilant states.5 Furthermore, personality characteristics have been found to be associated with variations in cortisol release and sympathetic-adrenal-medullary system activation in the stress response.24 Indeed, the effect of personality on the stress response differs with the situational context, including one’s past experiences and conditioning, cultural influences, and the availability of social support, and is influenced by one’s genetic profile4 and gender.
Beginning in the early 1970s researchers started to examine gender differences related to stress and recent research has continued to expand what is known about these differences between men and women.14,25–29 For example, one study in the 1980s examined the differences in performance and stress responses of men and women under controlled laboratory conditions.27 When subjected to a stressful task, there was a 50% to 100% increase in epinephrine release in men, whereas there was little if any increase noted in women, who were also found to perform as well or better than their male counterparts. Women did have an elevation in epinephrine release in a more real-life stress situation (i.e., an academic examination), but these elevations remained well below those of men.27 Although some researchers consider these differences, at least in part, to be related to gender-associated roles and psychological factors,26 other researchers also attribute these variances to the effects of the sex hormones on the stress response.28,29
Developmental stage of life and age also appear to relate to the way the body responds to stressors. Variations in HPA axis function are noticeable during adolescence, when sex hormone secretion is significantly elevated in both males and females.29 A prolonged HPA activation in response to stress in childhood has been documented in both genders when compared with that of adults. This physiologic finding has been suggested to impact the vulnerability of brain development in adolescents exposed to high levels of stress during this period.29 Adult women during the period between menarche and menopause have lower stress responses than men of the same age.28 It has been hypothesized that this is a physiologic evolutionary effort to protect the fetus from the effects of exposure to elevated levels of cortisol, in particular. Postmenopause, the responses of both the sympathetic nervous system and the HPA axis appear to increase.28 Clearly, stressors can affect the same person in different ways at different times over the course of a lifetime.
Risk factors alone are not inherently stressors, but rather conditions or situations that increase the likelihood of encountering or experiencing a stressor. Using a cellular phone while driving is a risk factor for having a motor vehicle accident; running in the dark is a risk factor for falling; inadequate immunization is a risk factor for certain infectious illnesses and even cancers. Risk factors include genetic predispositions and epigenetic factors, as well as early life experiences.4,30,31 By being aware of risk factors, it is possible to decrease the probability of exposure to certain stressors and their inevitable threat to homeostasis.