Patient Story
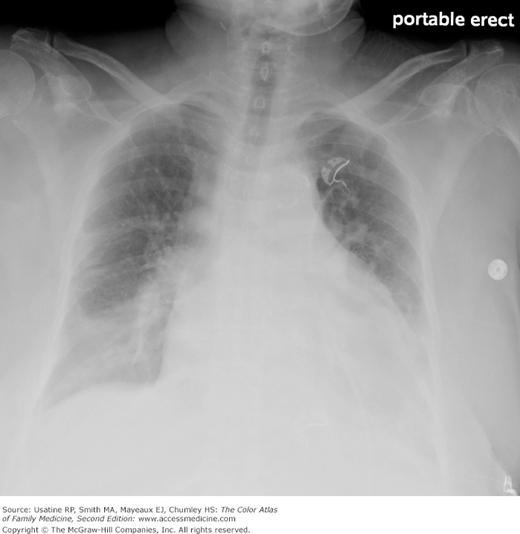
A 60-year-old man presents to the emergency department with shortness of breath increasing in severity over the past several days, along with paroxysmal nocturnal dyspnea and orthopnea. He does not have a history of heart failure or previous myocardial infarction. On examination it was found that he had a third heart sound and an elevated jugular venous pressure. His chest radiograph showed cardiomegaly (Figure 48-1) and his B-type natriuretic peptide (BNP) was elevated at 600 pg/mL. He was diagnosed with heart failure, evaluated for underlying causes including coronary artery disease, and treated initially with an angiotensin-converting enzyme inhibitor (ACEI) and a diuretic. Later, he will be started on a β-blocker and an aldosterone inhibitor.
Introduction
Epidemiology
- The prevalence of HF in the community increases with age: 0.7% (45 to 54 years); 1.3% (55 to 64 years); 1.5% (65 to 74 years); and 8.4% (75 years or older).1
- More than 40% of patients in the community with HF have an ejection fraction greater than 50%.1
- At age 40 years, the lifetime risk for HF is 21.0% (95% confidence interval [CI] 18.7% to 23.2%) for men and 20.3% (95% CI 18.2% to 22.5%) for women.2
Etiology and Pathophysiology
- Heart pumping capacity declines from any cause (i.e., myocardial infarction or ischemia, hypertension, valvular dysfunction, cardiomyopathy, or infections such as endocarditis or myocarditis).
- Cardiac dysfunction activates the adrenergic and renin-angiotensin-aldosterone systems.
- These systems provide short-term compensation, but chronic activation leads to myocardial remodeling and eventually worsening cardiac function.
- Norepinephrine, angiotensin II, aldosterone, and tissue necrosis factor each contribute to disease progression.
- Angiotensin II directly causes cell death through necrosis and apoptosis, as well as cardiac hypertrophy.
Diagnosis
Many history, examination, radiographic, ECG, and laboratory features are helpful in making the diagnosis of HF for patients presenting with dyspnea in the emergency department:3
- History and physical
- History of HF (LR + [likelihood ratio] = 5.8), myocardial infarction (LR+ = 3.1).3
- Symptoms of paroxysmal nocturnal dyspnea (LR+ = 2.6), orthopnea (LR+ = 2.2), edema (LR+ = 2.1).3
- Examination finding of third heart sound (LR+ = 11), hepatojugular reflex (LR+ = 6.4), jugular venous distention (LR+ = 5.1).3
- History of HF (LR + [likelihood ratio] = 5.8), myocardial infarction (LR+ = 3.1).3
- Laboratory value of BNP ≥250 (LR+ = 4.6); BNP <100 decreases likelihood of HF.3
- ECG finding of atrial fibrillation (LR+ = 3.8), T-wave changes (LR+ = 3.0), any abnormality (LR+ = 2.2). A normal ECG lowers likelihood (LR− = 0.640).3
- Radiographic finding of pulmonary venous congestion (Figure 48-2) (LR+ = 12.0), interstitial edema (LR+ = 12.0), alveolar edema (LR+ = 6.0), cardiomegaly (Figures 48-1, 48-2, and 48-3) (LR+ = 3.3).3