Patient Story
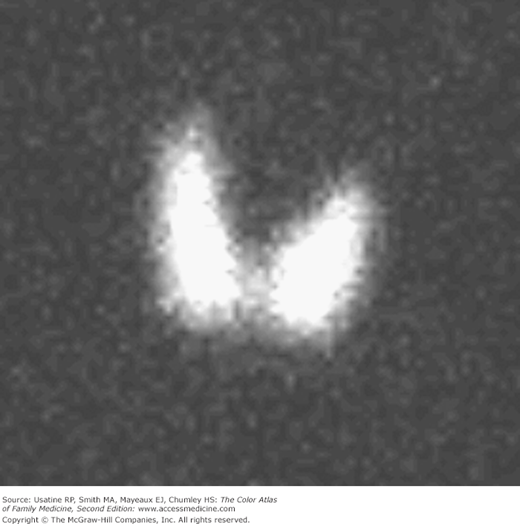
A 32-year-old woman presents with fatigue and “eye strain” (Figure 227-1). She had been working as a secretary and noticed difficulty focusing her eyes. She said she was anxious and was having difficulty writing. She reported that her sister was taking medication for “thyroid trouble.” A low thyroid-stimulating hormone (TSH) and an elevated free thyroxin level (T4) were found on laboratory testing, and the patient was diagnosed with Graves disease (GD). Her thyroid scan showed an enlarged thyroid with increased uptake (Figure 227-2). The patient chose radioactive iodine (RAI) as her treatment and her symptoms resolved. One year later she required levothyroxine treatment.
Introduction
GD is an autoimmune thyroid disorder characterized by circulating antibodies that stimulate the TSH receptor and resulting in hyperthyroidism.1
Synonyms
Epidemiology
- GD is a common disorder affecting 0.5% to 1.2% of the population.
- There is a female-to-male ratio of 5 to 10:1.
- Among patients with hyperthyroidism, 60% to 80% have GD; younger patients (younger than age 64 years) with hyperthyroidism are more likely to have GD than are older patients with hyperthyroidism.
- Graves ophthalmopathy (see “Clinical Features” below) occurs in more than 80% of patients within 18 months of diagnosis of GD. The ophthalmopathy is clinically apparent in 30% to 50% of patients.2
- Goiter is present in 90% of patients younger than age 50 years (vs. 75% in older patients with GD).1
- Untreated hyperthyroidism can lead to osteoporosis, atrial fibrillation, cardiomyopathy, and congestive heart failure; thyrotoxicosis (thyroid storm) has an associated mortality rate of 20% to 50%.3
Etiology and Pathophysiology
- The hyperthyroidism of GD results from circulating immunoglobulin (Ig) G antibodies that stimulate the TSH receptor.2 These antibodies are synthesized in the thyroid gland, bone marrow, and lymph nodes. Activation of the TSH receptor stimulates follicular hypertrophy and hyperplasia causing thyroid enlargement (goiter) and an increase in thyroid hormone production with an increased fraction of triiodothyronine (T3) relative to T4 (from approximately 20% to up to 30%).2
- The etiology is seen as a combination of genetic (human leukocyte antigen-D related [HLA-DR] and cytotoxic T-lymphocyte antigen 4 [CTLA-4] polymorphisms) and environmental factors, including physical and emotional stress (e.g., infection, childbirth, life events).2 In addition, insulin-like growth factor-1 receptor (IGF-1R)-bearing fibroblasts and B-cells exhibiting the IGF-1R(+) phenotype may be involved in the connective tissue manifestations.4 Siblings have higher incidence of both GD and Hashimoto thyroiditis (Chapter 226, Goitrous Hypothyroidism).
- The ophthalmopathy is believed to result from an autoimmune response directed toward an antigen shared by the thyroid and the eye’s orbit. There is infiltration of the extraocular muscles by activated T cells, which release cytokines, activating fibroblasts (fibrosis can lead to diplopia) and increasing the synthesis of glycosaminoglycans (water trapping causes swelling).2
Risk Factors
Diagnosis
There are several guidelines available for the diagnosis and management of thyroid disease in provider resources.
Symptoms depend on the severity of thyrotoxicosis, duration of disease, and age (findings are more subtle in the elderly). More than half of patients diagnosed with GD have these common symptoms:
- Nervousness.
- Fatigue.
- Weight loss.
- Heat intolerance.
- Palpitations.
Signs of disease include:
- Tachycardia (atrial fibrillation is common in patients >50 years of age).2
- Goiter—Listening over the goiter with a stethoscope may reveal a thyroid bruit (Figure 227-3).
- Resting tremor.
- Hyperreflexia
- Flushing and temporal wasting (Figure 227-4).
- Skin and nail changes include:
- Warm, erythematous, moist skin (from increased peripheral circulation).
- Palmer erythema.
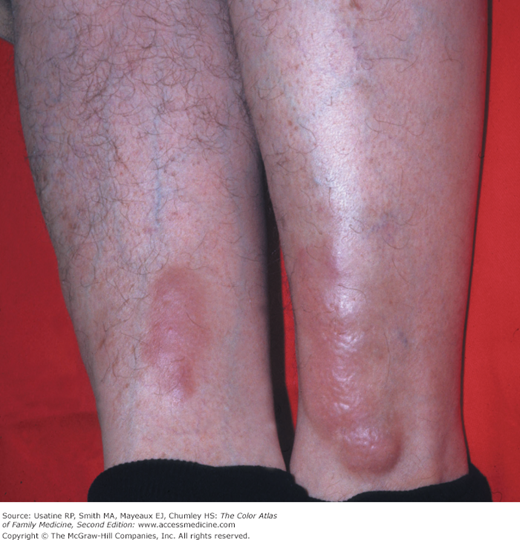
- Pretibial myxedema—Occurring in a small percentage of patients (0.5% to 4%), it consists of nonpitting scaly thickening and induration of the skin usually on the anterior shin and dorsa of the feet (Figures 227-5 and 227-6).5 It can also appear as a few well-demarcated pink, flesh-colored, or purple-brown papules or nodules.
- Nails are soft and shiny and may develop onycholysis (distal separation of the nail plate from the underlying nail bed).
- Warm, erythematous, moist skin (from increased peripheral circulation).
- Eye involvement may occur before hyperthyroidism (in 20% of patients) and gradually progresses with only mild discomfort (a gritty sensation with increased tearing is the earliest manifestation). The eye findings in GD1,2 are:
- Lid retraction (drawing back of the eyelid allowing more sclera to be visible) (Figures 227-1 and 227-7).
- Frank proptosis (displacement of the eye in the anterior direction); occurs in one-third (Figures 227-1 and 227-7).
- It is possible to have unilateral eye involvement with Graves ophthalmopathy (Figure 227-8).
- Extraocular muscle dysfunction (e.g., diplopia).
- Corneal exposure keratitis or ulcer.
- Periorbital edema, chemosis, and scleral injection.
- Lid retraction (drawing back of the eyelid allowing more sclera to be visible) (Figures 227-1 and 227-7).