High-Yield Terms to Learn
5 -Reductase The enzyme that converts testosterone to dihydrotestosterone (DHT); it is inhibited by finasteride, a drug used to treat benign prostatic hyperplasia and prevent male-pattern hair loss in men Anabolic steroid Androgen receptor agonists used for anabolic effects (eg, weight gain, increased muscle mass) Breakthrough bleeding Vaginal bleeding that occurs outside of the period of regular menstrual bleeding Combined oral contraceptive (COC or just OC) Hormonal contraceptive administered orally that contains an estrogen and a progestin Hirsutism A male pattern of body hair growth (face, chest, abdomen) in females that results from hyperandrogenism HRT Hormone replacement therapy; refers to estrogen replacement for women who have lost ovarian function and nearly always involves combination therapy with estrogen and a progestin SERM Selective estrogen receptor modulator such as tamoxifen
-Reductase The enzyme that converts testosterone to dihydrotestosterone (DHT); it is inhibited by finasteride, a drug used to treat benign prostatic hyperplasia and prevent male-pattern hair loss in men Anabolic steroid Androgen receptor agonists used for anabolic effects (eg, weight gain, increased muscle mass) Breakthrough bleeding Vaginal bleeding that occurs outside of the period of regular menstrual bleeding Combined oral contraceptive (COC or just OC) Hormonal contraceptive administered orally that contains an estrogen and a progestin Hirsutism A male pattern of body hair growth (face, chest, abdomen) in females that results from hyperandrogenism HRT Hormone replacement therapy; refers to estrogen replacement for women who have lost ovarian function and nearly always involves combination therapy with estrogen and a progestin SERM Selective estrogen receptor modulator such as tamoxifen
Ovarian Hormones
The ovary is the primary source of gonadal hormones in women during the childbearing years (ie, between puberty and menopause). When properly regulated by follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary, each menstrual cycle consists of the following events: A follicle in the ovary matures, secretes increasing amounts of estrogen, releases an ovum, and is transformed into a progesterone-secreting corpus luteum. If the ovum is not fertilized and implanted, the corpus luteum degenerates; the uterine endometrium, which has proliferated under the stimulation of estrogen and progesterone, is shed as part of the menstrual flow, and the cycle repeats. The mechanism of action of both estrogen and progesterone involves entry into cells, binding to cytosolic receptors, and translocation of the receptor-hormone complex into the nucleus, where it modulates gene expression (see Figure 39-1).
Estrogens
The major ovarian estrogen in women is estradiol. Estradiol has low oral bioavailability but is available in a micronized form for oral use. It can also be administered via transdermal patch, vaginal cream, or intramuscular injection. Long-acting esters of estradiol that are converted in the body to estradiol (eg, estradiol cypionate) can be administered by intramuscular (IM) injection. Mixtures of conjugated estrogens from biologic sources (eg, Premarin) are used orally for hormone replacement therapy (HRT). Synthetic estrogens with high bioavailability (eg, ethinyl estradiol, mestranol) are used in hormonal contraceptives.
Effects
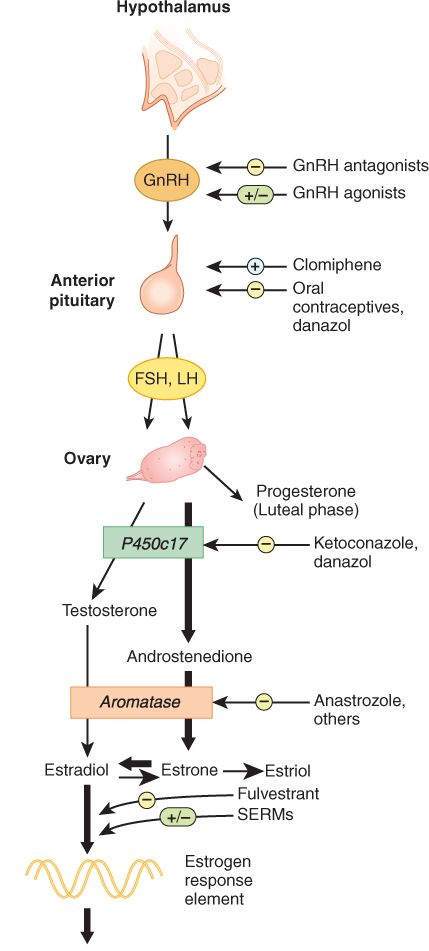
Estrogen is essential for normal female reproductive development. It is responsible for the growth of the genital structures (vagina, uterus, and uterine tubes) during childhood and for the appearance of secondary sexual characteristics and the growth spurt associated with puberty. Estrogen has many metabolic effects: It modifies serum protein levels and reduces bone resorption. It enhances the coagulability of blood and increases plasma triglyceride levels while reducing low-density lipoprotein (LDL) cholesterol and increasing high-density lipoprotein (HDL) cholesterol. Continuous administration of estrogen, especially in combination with a progestin, inhibits the secretion of gonadotropins from the anterior pituitary (Figure 40-1).
FIGURE 40-1
Control of ovarian secretion, the action of its hormones, and some sites of action of antiestrogens. In the follicular phase, the ovary produces mainly estrogens; in the luteal phase it produces estrogens and progesterone. SERMs, selective estrogen receptor modulators.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 40-5.)
Clinical Use
Estrogens are used in the treatment of hypogonadism in young females (Table 40-1). Another use is as HRT in women with estrogen deficiency resulting from premature ovarian failure, menopause, or surgical removal of the ovaries. HRT ameliorates hot flushes and atrophic changes in the urogenital tract. It is effective also in preventing bone loss and osteoporosis. The estrogens are components of hormonal contraceptives (see later discussion).
TABLE 40-1 Representative applications for the gonadal hormones and hormone antagonists.
Clinical Application Drugs Hypogonadism in girls, women Conjugated estrogens, ethinyl estradiol, estradiol esters Hormone replacement therapy Estrogen component: conjugated estrogens, estradiol, estrone, estriol Progestin component: progesterone, medroxyprogesterone acetate Oral hormonal contraceptive Combined: ethinyl estradiol or mestranol plus a progestin Progestin only: norethindrone or norgestrel Parenteral contraceptive Medroxyprogesterone as a depot IM injection Ethinyl estradiol and norelgestromin as a weekly patch Ethinyl estradiol and etonogestrel as a monthly vaginal ring L-Norgestrel as an intrauterine device (IUD) Etonogestrel as a subcutaneous implant Postcoital contraceptive L-Norgestrel, combined oral contraceptive Intractable dysmenorrhea or uterine bleeding Conjugated estrogens, ethinyl estradiol, oral contraceptive, GnRH agonist, depot injection of medroxyprogesterone acetate Infertility Clomiphene; hMG and hCG; GnRH analogs; progesterone; bromocriptine Abortifacient Mifepristone (RU 486) and misoprostol Endometriosis Oral contraceptive, depot injection of medroxyprogesterone acetate, GnRH agonist, danazol Breast cancer Tamoxifen, aromatase inhibitors (eg, anastrozole) Osteoporosis in postmenopausal women Conjugated estrogens, estradiol, raloxifene (see also Chapter 42) Hypogonadism in boys, men; replacement therapy Testosterone enanthate or cypionate; methyltestosterone; fluoxymesterone, testosterone (patch) Anabolic protein synthesis Oxandrolone, stanozolol Prostate hyperplasia (benign) Finasteride Prostate carcinoma GnRH agonist, GnRH receptor antagonist, androgen receptor antagonist (eg, flutamide) Hirsutism Combined oral contraceptive, spironolactone, flutamide, GnRH agonist
Toxicity
In hypogonadal girls, the dosage of estrogen must be adjusted carefully to prevent premature closure of the epiphyses of the long bones and short stature. When used as HRT, estrogen increases the risk of endometrial cancer; this effect is prevented by combining the estrogen with a progestin. Estrogen use by postmenopausal women is associated with a small increase in the risk of breast cancer and cardiovascular events (myocardial infarction, stroke). Dose-dependent toxicity includes nausea, breast tenderness, increased risk of migraine headache, thromboembolic events (eg, deep vein thrombosis), gallbladder disease, hypertriglyceridemia, and hypertension.
Diethylstilbestrol (DES), a nonsteroidal estrogenic compound, is associated with infertility, ectopic pregnancy, and vaginal adenocarcinoma in the daughters of women who were treated with the drug during pregnancy in a misguided attempt to prevent recurrent spontaneous abortion. These effects appear to be restricted to DES because there is no evidence that the estrogens and progestins in hormonal contraceptives have similar effects or other teratogenic effects.
Progestins
Progesterone is the major progestin in humans. A micronized form is used orally for HRT, and progesterone-containing vaginal creams are also available. Synthetic progestins (eg, medroxyprogesterone) have improved oral bioavailability. The 19-nortestosterone compounds differ primarily in their degree of androgenic effects. Older drugs (eg, L-norgestrel and norethindrone) are more androgenic than the newer progestins (eg, norgestimate, desogestrel).
Effects
Progesterone induces secretory changes in the endometrium and is required for the maintenance of pregnancy. The other progestins also stabilize the endometrium but do not support pregnancy. Progestins do not significantly affect plasma proteins, but they do affect carbohydrate metabolism and stimulate the deposition of fat. High doses suppress gonadotropin secretion and often cause anovulation in women.
Clinical Use
Progestins are used as contraceptives, either alone or in combination with an estrogen. They are used in combination with an estrogen in HRT to prevent estrogen-induced endometrial cancer. Progesterone is used in assisted reproductive technology methods to promote and maintain pregnancy.
Toxicity
The toxicity of progestins is low. However, they may increase blood pressure and decrease HDL. Long-term use of high doses in premenopausal women is associated with a reversible decrease in bone density (a secondary effect of ovarian suppression and decreased ovarian production of estrogen) and delayed resumption of ovulation after termination of therapy.
Hormonal Contraceptives
Hormonal contraceptives contain either a combination of an estrogen and a progestin or a progestin alone. Hormonal contraceptives are available in a variety of preparations, including oral pills, long-acting injections, transdermal patches, vaginal rings, and intrauterine devices (IUDs) (Table 40-1). Three types of oral contraceptives for women are available in the United States: combination estrogen-progestin tablets that are taken in constant dosage throughout the menstrual cycle (monophasic preparations); combination preparations (biphasic and triphasic) in which the progestin or estrogen dosage, or both, changes during the month (to more closely mimic hormonal changes in a menstrual cycle); and progestin-only preparations.
The postcoital contraceptives (also known as “emergency contraception”) prevent pregnancy if administered within 72 h after unprotected intercourse. Oral preparations containing a progestin (L-norgestrel) alone, estrogen alone, or the combination of an estrogen and a progestin are effective. The progestin-only preparation causes fewer side effects than the estrogen-containing preparations.
Mechanism of Action
The combination hormonal contraceptives have several actions, including inhibition of ovulation (the primary action) and effects on the cervical mucus glands, uterine tubes, and endometrium that decrease the likelihood of fertilization and implantation. Progestin-only agents do not always inhibit ovulation and instead act through the other mechanisms listed. The mechanisms of action of postcoital contraceptives are not well understood. When administered before the LH surge, they inhibit ovulation. They also affect cervical mucus, tubal function, and the endometrial lining.
Other Clinical Uses and Beneficial Effects
Combination hormonal contraceptives are used in young women with primary hypogonadism to prevent estrogen deficiency. Combinations of hormonal contraceptives and progestins are used to treat acne, hirsutism, dysmenorrhea, and endometriosis. Users of combination hormonal contraceptives have reduced risks of ovarian cysts, ovarian and endometrial cancer, benign breast disease, and pelvic inflammatory disease as well as a lower incidence of ectopic pregnancy, iron deficiency anemia, and rheumatoid arthritis.
Toxicity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree