Patient Story
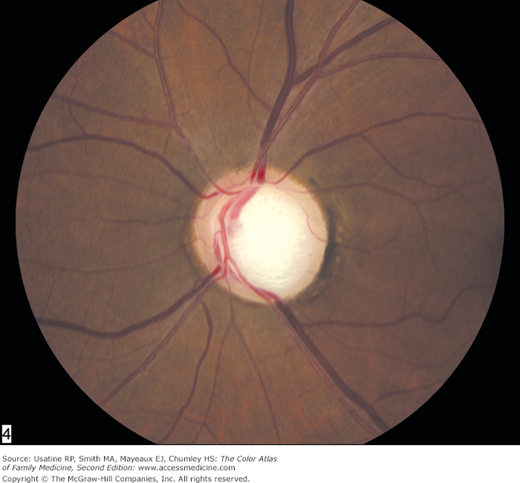
A 50-year-old black man was noted to have a large cup-to-disc ratio during a funduscopic examination by his primary care provider (Figure 19-1). The patient reported no visual complaints. Further evaluation revealed elevated intraocular pressure and early visual field defects. He was started on medication to lower his intraocular pressure. He remained asymptomatic, and his visual field defects did not progress for the next several years.
Introduction
Glaucoma is a leading cause of blindness in the United States and globally. Open-angle glaucoma is an acquired loss of retinal ganglion cells characterized by either normal or increased intraocular pressure, a large cup-to-disc ratio, and visual field defects. Open-angle glaucoma is treated by reducing intraocular pressure, most commonly with eye drops. Angle-closure glaucoma, which is much less common, is an acute increase in intraocular pressure from a mechanical obstruction that must be treated emergently to preserve vision.
Epidemiology
- Approximately 2.5 million persons in the United States have glaucoma.
- Glaucoma is the second leading cause of blindness in the United States and the leading cause of blindness among African Americans.1
- Population studies predict there will be 60.5 million people worldwide with glaucoma by 2010, and of these, 74% will have open-angle glaucoma.2
- Women comprise approximately 60% of all glaucoma cases, but 70% of patients with acute angle-closure glaucoma.2
- Asians comprise approximately 47% of all glaucoma cases, but 87% of acute angle-closure glaucoma.2
- The incidence of primary open-angle glaucoma was 8.3 per 100,000 population in people older than 40 years in a Minnesota population study.3
- According to a population-based study, a family history of glaucoma increased the risk of having glaucoma (odds ratio [OR] = 3.08).4
Etiology and Pathophysiology
- Glaucoma pathophysiology is incompletely understood, but the end point is the acquired loss of retinal ganglion cells and axons with resulting irreversible vision loss.
- Increased intraocular pressure (IOP) is a well known risk factor; however, recent attention has turned to ocular perfusion pressure (OPP), the difference between blood pressure (BP) and IOP. OPP is essentially BP minus IOP. As such, OPP is decreased by either high IOP or low BP.5 If a patient with apparently well-controlled IOP continues to have progressive visual field loss, it may be because of lack of perfusion of the optic nerve from aggressively lowered diastolic BPs. Therefore the management of glaucoma requires attention to diastolic BP.
- Glaucoma is categorized as either:
- Open-angle—Dysfunction of the aqueous humor drainage system with no visible pathology to the anterior chamber angle.
- Angle-closure—Occlusion of the anterior chamber angle.
- Open-angle—Dysfunction of the aqueous humor drainage system with no visible pathology to the anterior chamber angle.
- Impaired outflow of aqueous humor elevates IOP in some patients, but many patients with open-angle glaucoma have normal IOPs.
- Optic nerve atrophy is seen as optic disc cupping and irreversible visual field loss. Compare Figures 19-1 and 19-2 to see the difference between abnormal (Figure 19-1) and normal (Figure 19-2) optic disc cupping.
Risk Factors
- Nonmodifiable: age older than 50 years, first-degree family history, and African ancestry.6
- Modifiable: high IOP, high or low BP, and maybe diabetes mellitus.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree