Giant Cell Tumor
G. Petur Nielsen, MD
Andrew E. Rosenberg, MD
Key Facts
Terminology
Neoplasm composed of cytologically benign, oval or polyhedral mononuclear cells that are admixed with numerous, evenly distributed, osteoclast-like giant cells
Clinical Issues
Represents approximately 5% of primary bone tumors
Vast majority arise in epiphyseal-metaphyseal region of long tubular bones
Pain and swelling
Usually treated by curettage
Local recurrence rate approximately 25% for patients treated with curettage
1-2% of GCTs eventually metastasize, primarily to lungs
Image Findings
Large
Purely lytic
Cystic degeneration is common secondary finding (aneurysmal bone cyst-like changes)
Macroscopic Features
Friable
Hemorrhagic
Red-brown
Microscopic Pathology
Mononuclear cells are diagnostic and neoplastic component of tumor
Numerous, multinucleated osteoclast-like giant cells that are scattered evenly throughout tumor
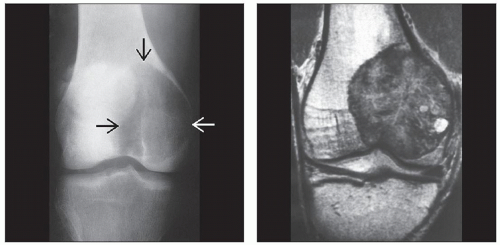
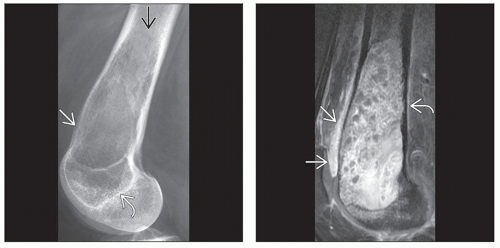
 A giant cell tumor involving the distal femur shows a geographic lytic lesion with extension to the subchondral plate. The margins are well defined and nonsclerotic with cortical thinning medially. |
TERMINOLOGY
Abbreviations
Giant cell tumor (GCT)
Synonyms
Osteoclastoma
Definitions
Benign but locally aggressive neoplasm composed of cytologically banal, oval or polyhedral mononuclear cells admixed with numerous, evenly distributed, osteoclast-like giant cells
ETIOLOGY/PATHOGENESIS
Neoplastic
Mononuclear cells are neoplastic cells of possible osteoblast phenotype that induce formation of osteoclast-type giant cells by expressing receptor activator of NF-κΒ (RANK) ligand
Osteoclast-type giant cells express receptor RANK, which binds to RANK ligand on surfaces of mononuclear cells
CLINICAL ISSUES
Epidemiology
Incidence
Represents approximately 5% of primary bone tumors
Represents approximately 20% of benign bone tumors
Age
Develops in skeletally mature individuals during 3rd-5th decades of life
Rarely occurs in children
Gender
Females are affected slightly more frequently than males
Site
Vast majority arise in epiphyseal-metaphyseal region of long tubular bones
Tumors in patients with open growth plates are often centered in metaphysis and abut epiphyseal plate
Rarely arise in diaphysis
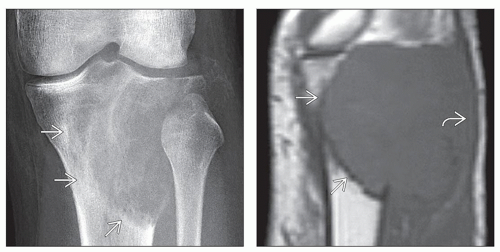
In almost 1/2 of cases, GCT develops around knee, with predilection for distal femur, followed by proximal tibia and distal radius
Uncommon sites include vertebral bodies, short tubular bones of hands and feet, craniofacial bones, and patella
Many giant cell tumors of bone that arise in craniofacial skeleton occur in setting of Paget disease of bone
Usually solitary
1% of cases are multifocal, and these often affect bones of hands and feet
Presentation
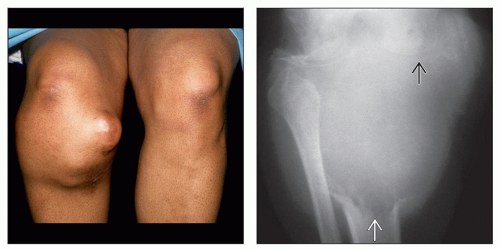
Pain, swelling, pathologic fracture in minority of cases
Treatment
Surgical approaches
Usually treated by thorough curettage
En bloc resection for large tumors with little residual structural bone
Drugs
Preliminary studies with RANK ligand inhibitors such as denosumab seem to be effective and may possibly supplement radiation treatment and surgery in difficult cases
Tumor locally recurs if drug therapy is discontinued
Radiation
Prognosis
Local recurrence rate approximately 25% for patients treated with curettage, usually within 3 years
Although GCT of bone is classified as a benign neoplasm, it is well recognized that 1-2% eventually metastasize, primarily to lungs
Metastatic deposits frequently cured by resection
Metastatic disease can also be treated with RANK ligand inhibitors such as denosumab
Metastases occur more frequently in patients with pathologic fracture or following multiple curettages for recurrent disease
Uncommon complication is development of sarcoma within a GCT
This may occur de novo, develop in a locally recurrent tumor, or happen following radiation therapy
IMAGE FINDINGS
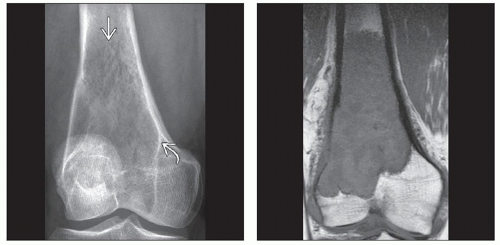
Radiographic Findings
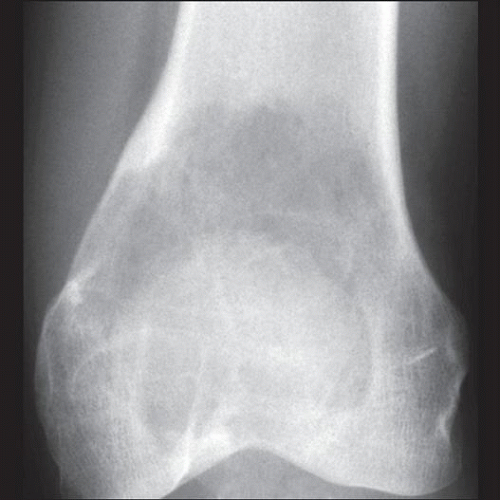
Large, lytic, intramedullary and frequently eccentric
Usually extends from metaphysis to subchondral bone plate
Very large tumors may involve adjacent diaphysis, focally destroy cortex, and invade into neighboring soft tissues
May expand bone and elevate periosteum
Results in thin periosteal shell of reactive bone, which may be incomplete
Medullary margins are well defined, may have “motheaten” appearance, and are usually not sclerotic
Cystic degeneration is common secondary finding (aneurysmal bone cyst-like changes)
After RANKL inhibitor therapy, tumor shows increased sclerosis/bone formation
MR Findings
Low to intermediate signal on T1- and T2-weighted images
T1 is better to see intramedullary component of tumor
T2 is better to evaluate extraosseous component of large tumors and to identify any cystic changes (fluid-fluid levels)
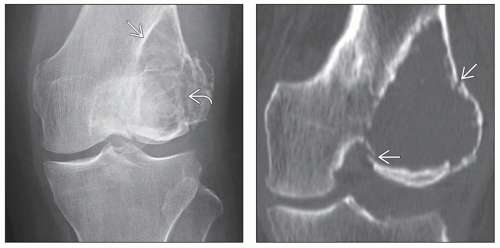
CT Findings
Tumor is lytic with well-defined borders
Bone Scan
Increased uptake on technetium scan
MACROSCOPIC FEATURES
General Features
Friable, hemorrhagic, red-brown
Solid or focally cystic
Erodes cortex
Well-delineated margins within medullary canal and in neighboring soft tissues
Sections to Be Submitted
10 cassettes for curettage specimens
Resection specimens: Bone and soft tissue margins, minimum of 1 section per cm of tumor
Size
Typically range from 5-15 cm in dimension
MICROSCOPIC PATHOLOGY
Histologic Features
Mononuclear stromal cells are diagnostic and neoplastic component of tumor
Numerous multinucleated osteoclast-like giant cells are scattered evenly throughout tumor
Number of nuclei in any individual cell variable but may be as many as 50 or more
Mononuclear cells appear to grow in a syncytium, have ill-defined cell borders, and little eosinophilic cytoplasm
Tumor cell nuclei are round or ovoid, vesicular, have central nucleoli, and are morphologically identical to nuclei of giant cells
Mononuclear cells may be mitotically active and can show variable degrees of cytologic atypia
Atypia may be prominent in areas admixed with previous hemorrhage and fibrin deposition
Foci of necrosis and vascular invasion may be present
Tumor can demonstrate benign fibrous histiocytomalike areas that are devoid of classic mononuclear and osteoclast-type giant cells
Other secondary changes commonly encountered in GCT include hemosiderin deposits, aggregates of foamy macrophages, cystic changes, and reactive bone formation
Following RANKL inhibitor therapy, giant cells disappear, mononuclear tumor cells decrease, and bone formation increases
Soft tissue recurrence is frequently surrounded by shell of reactive bone
Ultrastructural Features
Abundant dilated rough endoplasmic reticulum, well-developed Golgi apparatus, mitochondria, and occasional lipid droplets
None of these features are specific for GCT of bone
ANCILLARY TESTS
Immunohistochemistry
Giant cells have immunoprofile similar to macrophages
Osteoclast-type giant cells stain for RANK
Many of stromal mononuclear tumor cells stain for RANKL, indicating that they may have osteoblastic phenotype
Mononuclear tumor cells show nuclear staining for p63
DIFFERENTIAL DIAGNOSIS
Nonossifying Fibroma/Benign Fibrous Histiocytoma
Most GCTs have areas that resemble benign fibrous histiocytoma or nonossifying fibroma
Areas are composed of banal spindle cells arranged in storiform pattern with scattered osteoclast-like giant cells
Spindle cell component is frequently located at periphery of tumor and is not diagnostic of GCT
True nonossifying fibroma/benign fibrous histiocytoma does not have characteristic giant cell tumor-like areas
Chondroblastoma
Seen in skeletally immature individuals with an open growth plate and is centered in epiphysis
Mononuclear cells do not resemble nuclei of osteoclast-type giant cells as seen in GCT of bone
“Chicken wire” calcifications and chondroid areas frequently seen in chondroblastoma and are not present in GCT of bone
Mononuclear cells in chondroblastoma stain for S100 but are usually negative for p63
Giant Cell Reparative Granuloma/Brown Tumor
Contains clusters of osteoclast-type giant cells around area of hemorrhage
In contrast, in GCT of bone, giant cells are usually evenly distributed
Proliferating cells are spindle-shaped and do not resemble nuclei of osteoclast-type giant cells
Aneurysmal Bone Cyst
Difficult to distinguish between primary aneurysmal bone cyst and cystic GCT of bone
In cystic GCT of bone, characteristic morphologic areas must be present
FISH for t(16;17) present in primary aneurysmal bone cyst may be helpful
Giant Cell-Rich Osteosarcoma
Tumor grows with an infiltrative pattern
Contains cytologically malignant mononuclear cells
DIAGNOSTIC CHECKLIST
Clinically Relevant Pathologic Features
Lytic lesion in distal long bone extending to subchondral area in an adult is characteristic
Pathologic Interpretation Pearls
Proliferation of mononuclear cells and evenly distributed osteoclast-type giant cells
Nuclei of mononuclear cells identical to those of osteoclast-type giant cells
If a needle biopsy looks like fibrous histiocytoma, think possible GCT
SELECTED REFERENCES
1. Klenke FM et al: Giant cell tumor of bone: risk factors for recurrence. Clin Orthop Relat Res. 469(2):591-9, 2011
2. Thomas D et al: Denosumab in patients with giant-cell tumour of bone: an open-label, phase 2 study. Lancet Oncol. 11(3):275-80, 2010
3. Lee CH et al: Gene expression profiling identifies p63 as a diagnostic marker for giant cell tumor of the bone. Mod Pathol. 21(5):531-9, 2008
4. Rock MG et al: Secondary malignant giant-cell tumor of bone. Clinicopathological assessment of nineteen patients. J Bone Joint Surg Am. 68(7):1073-9, 1986
5. Rock MG et al: Metastases from histologically benign giantcell tumor of bone. J Bone Joint Surg Am. 66(2):269-74, 1984
Image Gallery
Imaging Features
Clinical and Imaging Features
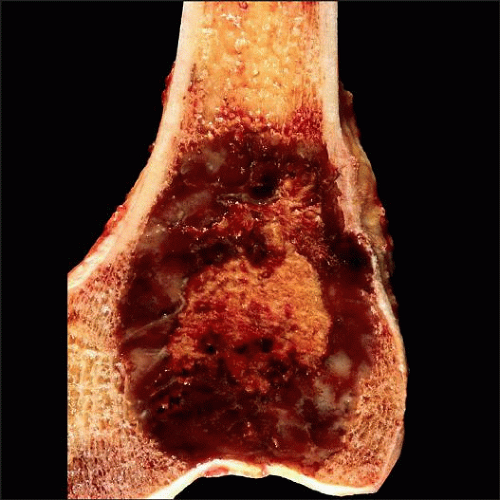
Imaging and Gross Features
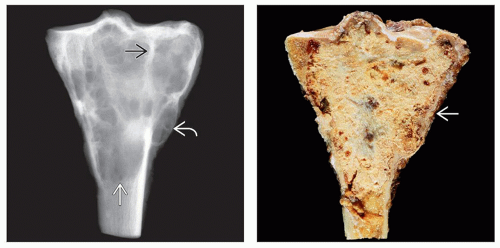 (Left) Specimen radiograph of a giant cell tumor of bone involving the proximal tibia shows a multiloculated, subarticular lesion with focal areas of cortical expansion
 , internal septation , internal septation  , and a well-demarcated distal margin , and a well-demarcated distal margin  . (Right) Gross photograph of a giant cell tumor of bone arising in the proximal tibia shows that the tan-yellow tumor extends to the articular cartilage and has broken through the cortex laterally with a thin layer of periosteal new bone . (Right) Gross photograph of a giant cell tumor of bone arising in the proximal tibia shows that the tan-yellow tumor extends to the articular cartilage and has broken through the cortex laterally with a thin layer of periosteal new bone  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|