General Principles of Cancer Chemotherapy
INTRODUCTION. Cancer pharmacology has changed dramatically as curative treatments have been identified for many previously fatal malignancies such as testicular cancer, lymphomas, and leukemia. Adjuvant chemotherapy and hormonal therapy can extend life and prevent disease recurrence following surgical resection of localized breast, colorectal, and lung cancers. Chemotherapy is also employed as part of the multimodal treatment of locally advanced head and neck, breast, lung, and esophageal cancers, soft-tissue sarcomas, and pediatric solid tumors, thereby allowing for more limited surgery and even cure in these formerly incurable cases. Colony-stimulating factors restore bone marrow function and expand the utility of high-dose chemotherapy. Chemotherapeutic drugs are increasingly used in nonmalignant diseases: cytotoxic antitumor agents have become standard in treating autoimmune diseases, including rheumatoid arthritis (methotrexate and cyclophosphamide), Crohn disease (6-mercaptopurine), organ transplantation (methotrexate and azathioprine), sickle cell anemia (hydroxyurea), and psoriasis (methotrexate). Despite these therapeutic successes, few categories of medication have a narrower therapeutic index and greater potential for causing harmful effects than the cytotoxic antineoplastic drugs. A thorough understanding of their pharmacology, including drug interactions and clinical pharmacokinetics, is essential for their safe and effective use in humans.
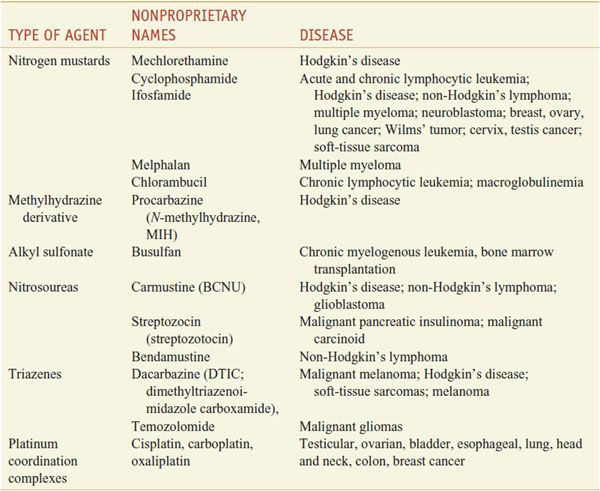
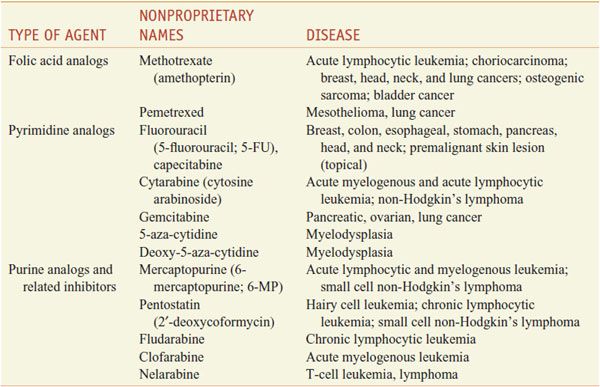
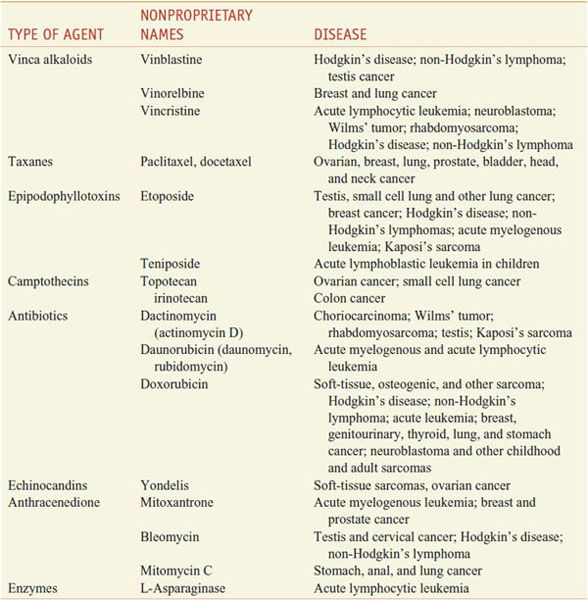
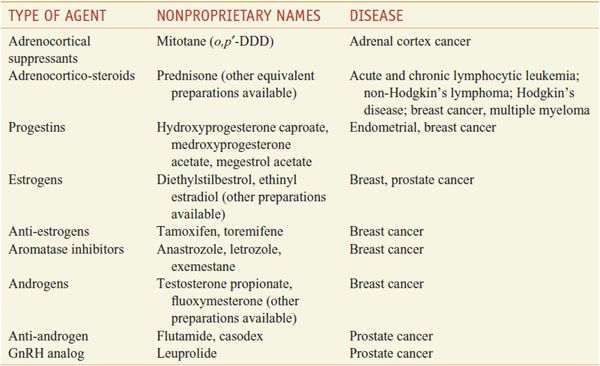
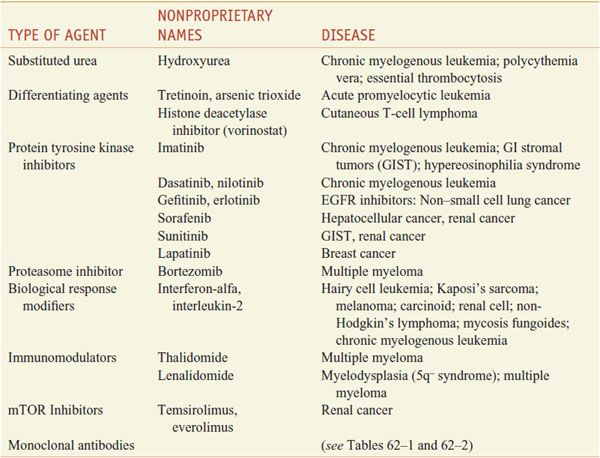
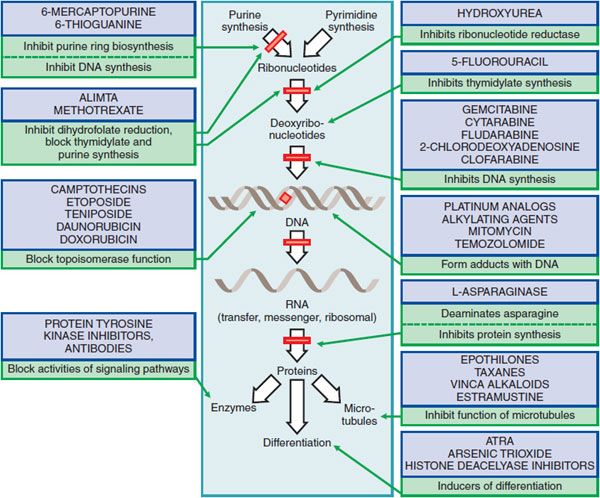
The compounds used in the chemotherapy of neoplastic disease are quite varied in structure and mechanism of action, including alkylating agents; antimetabolite analogs of folic acid, pyrimidine, and purine; natural products; hormones and hormone antagonists; and a variety of agents directed at specific molecular targets. Tables 60–1 through 60–5 summarize of the main classes and examples of these drugs. Figure 60–1 depicts the cellular targets of chemotherapeutic agents.
Table 60–1
Alkylating Agents
Table 60–2
Antimetabolites
Table 60–3
Natural Products
Table 60–4
Hormones and Antagonists
Table 60–5
Miscellaneous Agents
Figure 60–1 Mechanisms and sites of action of some chemotherapeutic agents for neoplastic disease.
The rapidly expanding knowledge of cancer biology has led to the discovery of entirely new and more cancer-specific targets (e.g., growth factor receptors, intracellular signaling pathways, epigenetic processes, tumor vascularity, DNA repair defects, and cell death pathways). For example, in many tumors, proliferation and survival depends on the constitutive activity of a single growth factor pathway, or so-called oncogene addiction (i.e., the “Achilles heel”), and inhibition of that pathway leads to cell death. Thus, imatinib (GLEEVEC) attacks the unique and specific bcr-abl translocation in chronic myelocytic leukemia. Imatinib also inhibits c-kit and produces extended control of GI stromal tumors that express a mutated and constitutively activated form of c-kit. Monoclonal antibodies effectively inhibit tumor-associated antigens such as the amplified her-2/neu receptor in breast cancer cells. These examples emphasize that entirely new strategies for drug discovery and development, and advances in patient care, will result from new knowledge of cancer biology.
New clinical trial designs, aimed at determining effects of new drugs at the molecular level, increasingly employ biomarkers derived from samples of biological fluids or tumors to assess the effects of these new agents on signaling pathways, tumor proliferation and cell death, and angiogenesis. Imaging of molecular, metabolic, and physiological effects of drugs will become increasingly important in establishing that drugs effectively engage their targets.
New therapies are not likely to replace cytotoxics in the foreseeable future. Rather, the targeted drugs and cytotoxics will continue to be used in combination. For instance, monoclonal antibodies or small targeted molecules, used as single agents against solid tumors, produce low response rates and modest benefits; however, in combination with cytotoxics and in early stages of disease, monoclonal antibodies such as trastuzumab (HERCEPTIN) and bevacizumab (AVASTIN) are dramatically effective. At the same time, the toxicities of cytotoxic drugs have become more manageable with the development of better anti-nausea medications (see Chapters 13 and 46) and with granulocyte colony-stimulating factor and erythropoietin to restore bone marrow function (see Chapters 37 and 62). Finally, targeted drugs are helping to overcome resistance to chemotherapeutic agents by normalizing blood flow, promoting apoptosis, and inhibiting pro-survival signals from growth factor pathways. Tumor angiogenesis leads to increased interstitial pressure and diminishes delivery of drugs to tumor cells; inhibitors of angiogenesis (e.g., bevacizumab) normalize blood flow and interstitial pressure, improve drug delivery, and are thus synergistic with cytotoxic drugs in the treatment of lung, breast, and other cancers.
Drug resistance remains a major obstacle to successful cancer treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree