High-Yield Terms to Learn
Balanced anesthesia Anesthesia produced by a mixture of drugs, often including both inhaled and intravenous agents Inhalation anesthesia Anesthesia induced by inhalation of drug Minimum alveolar anesthetic concentration (MAC) The alveolar concentration of an anesthetic that is required to prevent a response to a standardized painful stimulus in 50% of patients Analgesia A state of decreased awareness of pain, sometimes with amnesia General anesthesia A state of unconsciousness, analgesia, and amnesia, with skeletal muscle relaxation and loss of reflexes
Stages of Anesthesia
Modern anesthetics act very rapidly and achieve deep anesthesia quickly. With older and more slowly acting anesthetics, the progressively greater depth of central depression associated with increasing dose or time of exposure is traditionally described as stages of anesthesia.
Stage 1: Analgesia
In stage 1, the patient has decreased awareness of pain, sometimes with amnesia. Consciousness may be impaired but is not lost.
Stage 2: Disinhibition
In stage 2, the patient appears to be delirious and excited. Amnesia occurs, reflexes are enhanced, and respiration is typically irregular; retching and incontinence may occur.
Stage 3: Surgical Anesthesia
In stage 3, the patient is unconscious and has no pain reflexes; respiration is very regular, and blood pressure is maintained.
Stage 4: Medullary Depression
In stage 4, the patient develops severe respiratory and cardiovascular depression that requires mechanical and pharmacologic support.
Anesthesia Protocols
Anesthesia protocols vary according to the proposed type of diagnostic, therapeutic, or surgical intervention. For minor procedures, conscious sedation techniques that combine intravenous agents with local anesthetics (see Chapter 26) are often used. These can provide profound analgesia, with retention of the patient’s ability to maintain a patent airway and respond to verbal commands. For more extensive surgical procedures, anesthesia protocols commonly include intravenous drugs to induce the anesthetic state, inhaled anesthetics (with or without intravenous agents) to maintain an anesthetic state, and neuromuscular blocking agents to effect muscle relaxation (see Chapter 27). Vital sign monitoring remains the standard method of assessing “depth of anesthesia” during surgery. Cerebral monitoring, automated techniques based on quantification of anesthetic effects on the electroencephalograph (EEG), is also useful.
Mechanisms of Action
The mechanisms of action of general anesthetics are varied. As CNS depressants, these drugs usually increase the threshold for firing of CNS neurons. The potency of inhaled anesthetics is roughly proportional to their lipid solubility. Mechanisms of action include effects on ion channels by interactions of anesthetic drugs with membrane lipids or proteins with subsequent effects on central neurotransmitter mechanisms. Inhaled anesthetics, barbiturates, benzodiazepines, etomidate, and propofol facilitate  -aminobutyric acid (GABA)-mediated inhibition at GABAA receptors. These receptors are sensitive to clinically relevant concentrations of the anesthetic agents and exhibit the appropriate stereospecific effects in the case of enantiomeric drugs. Ketamine does not produce its effects via facilitation of GABAA receptor functions, but possibly via its antagonism of the action of the excitatory neurotransmitter glutamic acid on the N-methyl-D-aspartate (NMDA) receptor. Most inhaled anesthetics also inhibit nicotinic acetylcholine (ACh) receptor isoforms at moderate to high concentrations. The strychnine-sensitive glycine receptor is another ligand-gated ion channel that may function as a “target” for certain inhaled anesthetics. CNS neurons in different regions of the brain have different sensitivities to general anesthetics; inhibition of neurons involved in pain pathways occurs before inhibition of neurons in the midbrain reticular formation.
-aminobutyric acid (GABA)-mediated inhibition at GABAA receptors. These receptors are sensitive to clinically relevant concentrations of the anesthetic agents and exhibit the appropriate stereospecific effects in the case of enantiomeric drugs. Ketamine does not produce its effects via facilitation of GABAA receptor functions, but possibly via its antagonism of the action of the excitatory neurotransmitter glutamic acid on the N-methyl-D-aspartate (NMDA) receptor. Most inhaled anesthetics also inhibit nicotinic acetylcholine (ACh) receptor isoforms at moderate to high concentrations. The strychnine-sensitive glycine receptor is another ligand-gated ion channel that may function as a “target” for certain inhaled anesthetics. CNS neurons in different regions of the brain have different sensitivities to general anesthetics; inhibition of neurons involved in pain pathways occurs before inhibition of neurons in the midbrain reticular formation.
Inhaled Anesthetics
Classification and Pharmacokinetics
The agents currently used in inhalation anesthesia are nitrous oxide (a gas) and several easily vaporized liquid halogenated hydrocarbons, including halothane, desflurane, enflurane, isoflurane, sevoflurane, and methoxyflurane. They are administered as gases; their partial pressure, or “tension,” in the inhaled air or in blood or other tissue is a measure of their concentration. Because the standard pressure of the total inhaled mixture is atmospheric pressure (760 mm Hg at sea level), the partial pressure may also be expressed as a percentage. Thus, 50% nitrous oxide in the inhaled air would have a partial pressure of 380 mm Hg. The speed of induction of anesthetic effects depends on several factors, discussed next.
Solubility
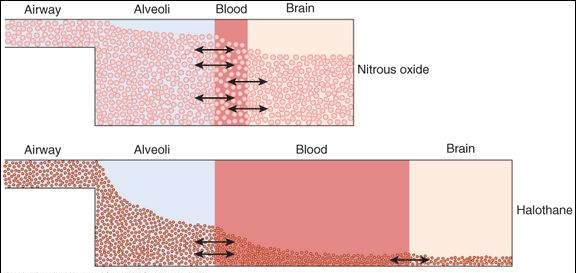
The more rapidly a drug equilibrates with the blood, the more quickly the drug passes into the brain to produce anesthetic effects. Drugs with a low blood:gas partition coefficient (eg, nitrous oxide) equilibrate more rapidly than those with a higher blood solubility (eg, halothane), as illustrated in Figure 25-1. Partition coefficients for inhalation anesthetics are shown in Table 25-1.
FIGURE 25-1
Why induction of anesthesia is slower with more soluble anesthetic gases and faster with less soluble ones. In this schematic diagram, solubility is represented by the size of the blood compartment (the more soluble the gas, the larger is the compartment). For a given concentration or partial pressure of the 2 anesthetic gases in the inspired air, it will take much longer with halothane than with nitrous oxide for the blood partial pressure to rise to the same partial pressure as in the alveoli. Because the concentration in the brain can rise no faster than the concentration in the blood, the onset of anesthesia will be much slower with halothane than with nitrous oxide.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 25-3.)
TABLE 25-1 Properties of inhalation anesthetics.
Anesthetic Blood: Gas Partition Coefficient Minimum Alveolar Concentration (%)a
Metabolism Nitrous oxide 0.47 >100 None Desflurane 0.42 6.5 <0.1% Sevoflurane 0.69 2.0 2-5% (fluoride) Isoflurane 1.40 1.4 <2% Enflurane 1.80 1.7 8% Halothane 2.30 0.75 >40% Methoxyflurane 12 0.16 >70% (fluoride)
aMinimum alveolar concentration (MAC) is the anesthetic concentration that eliminates the response in 50% of patients exposed to a standardized painful stimulus. In this table, MAC is expressed as a percentage of the inspired gas mixture.
Modified and reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 10th ed. McGraw-Hill, 2007.
Inspired Gas Partial Pressure
A high partial pressure of the gas in the lungs results in more rapid achievement of anesthetic levels in the blood. This effect can be taken advantage of by the initial administration of gas concentrations higher than those required for maintenance of anesthesia.
Ventilation Rate
The greater the ventilation, the more rapid is the rise in alveolar and blood partial pressure of the agent and the onset of anesthesia (Figure 25-2). This effect is taken advantage of in the induction of the anesthetic state.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree