http://evolve.elsevier.com/McCuistion/pharmacology/
Drug groups used to correct or control vomiting, diarrhea, and constipation are antiemetics, emetics, antidiarrheals, and laxatives. Each of these drug groups is discussed separately. Drugs used to treat peptic ulcers are discussed in Chapter 43.
Vomiting
Vomiting (emesis), the expulsion of gastric contents, has a multitude of causes, including motion sickness, viral and bacterial infection, food intolerance, surgery, pregnancy, pain, shock, effects of selected drugs (e.g., antineoplastics, antibiotics), radiation, and disturbances of the middle ear that affect equilibrium. Nausea, a queasy sensation, may or may not precede the expulsion. The cause of the vomiting must be identified. Antiemetics can mask the underlying cause of vomiting and should not be used until the cause has been determined, unless the vomiting is so severe as to cause dehydration and electrolyte imbalance.
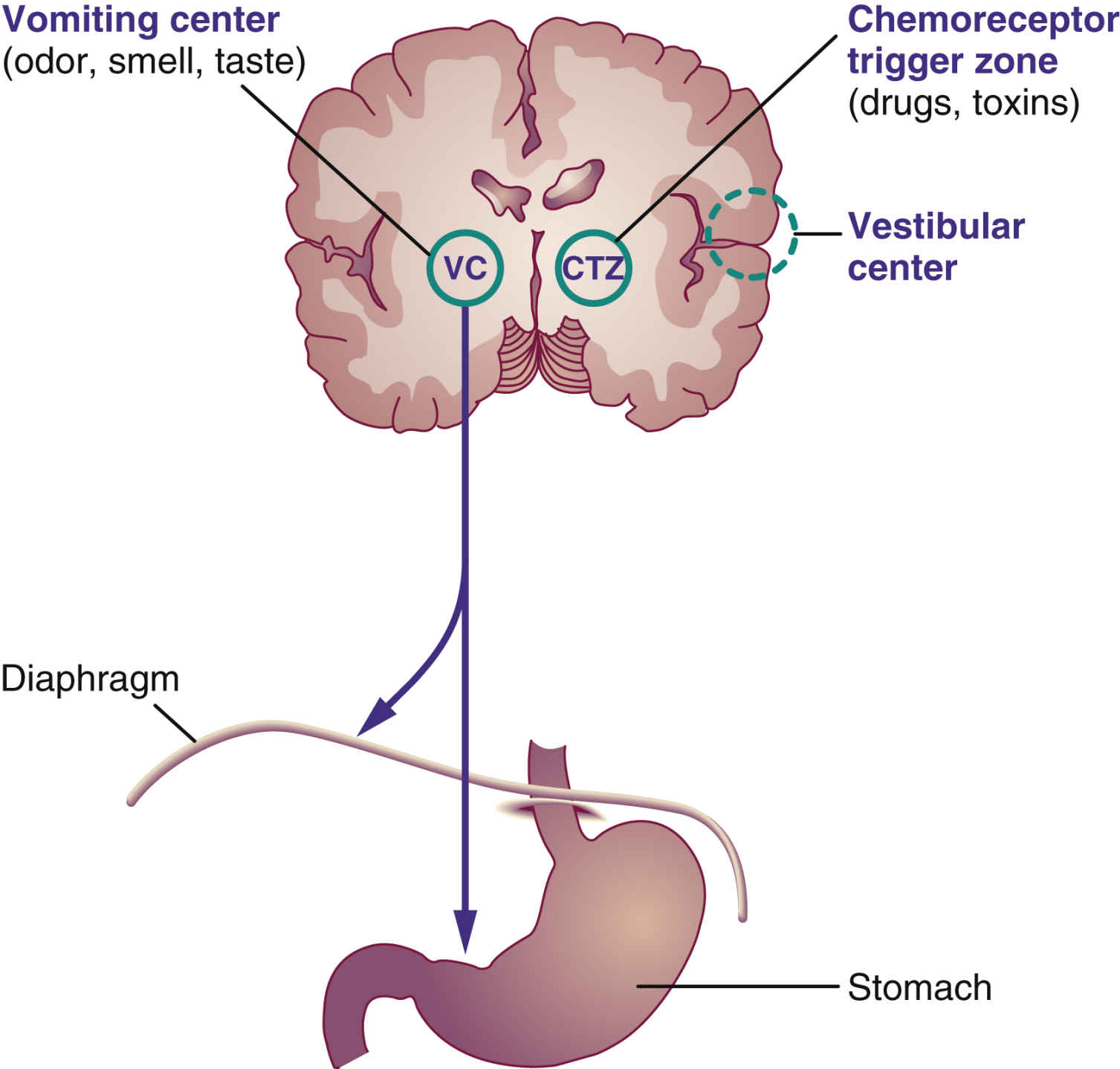
Two major cerebral centers—the chemoreceptor trigger zone (CTZ), which lies near the medulla, and the vomiting center in the medulla—cause vomiting when stimulated (Fig. 42.1). The CTZ receives most of the impulses from drugs, toxins, and the vestibular center in the ear and transmits them to the vomiting center. The neurotransmitter dopamine stimulates the CTZ, which in turn stimulates the vomiting center. Levodopa, a drug with dopamine-like properties, can cause vomiting by stimulating the CTZ. Some sensory impulses—such as odor, smell, taste, and gastric mucosal irritation—are transmitted directly to the vomiting center. The neurotransmitter acetylcholine is also a vomiting stimulant. When the vomiting center is stimulated, the motor neuron responds by causing contraction of the diaphragm, the anterior abdominal muscles, and the stomach. The glottis closes, the abdominal wall moves upward, and vomiting occurs.
Nonpharmacologic measures should be used first when nausea and vomiting occur. If the nonpharmacologic measures are not effective, antiemetics are combined with nonpharmacologic measures. The two major groups of antiemetics are nonprescription (antihistamines, bismuth subsalicylate, and phosphorated carbohydrate solution) and prescription (antihistamines, dopamine antagonists, benzodiazepines, serotonin antagonists, glucocorticoids, cannabinoids, and miscellaneous antiemetics).
Nonpharmacologic Measures
The nonpharmacologic methods of decreasing nausea and vomiting include administration of weak tea, flat soda, gelatin, Gatorade, and Pedialyte (for use in children). Crackers and dry toast may be helpful. When dehydration becomes severe, intravenous (IV) fluids are needed to restore body fluid balance.
Nonprescription Antiemetics
Nonprescription antiemetics (antivomiting agents) can be purchased as over-the-counter (OTC) drugs. These drugs are frequently used to prevent motion sickness but have minimal effect on controlling severe vomiting resulting from anticancer agents (antineoplastics), radiation, and toxins. To prevent motion sickness, the antiemetic should be taken 30 minutes before travel. These drugs are not effective in relieving motion sickness if taken after vomiting has occurred.
Selected antihistamine antiemetics—such as dimenhydrinate, cyclizine hydrochloride, meclizine hydrochloride, and diphenhydramine hydrochloride—can be purchased without a prescription to prevent nausea, vomiting, and dizziness (vertigo) caused by motion. These drugs inhibit vestibular stimulation in the middle ear. Diphenhydramine is also used to prevent or alleviate allergic reactions to drugs, insects, and food by acting as an antagonist to histamine1 (H1) receptors.
The side effects of antihistamine antiemetics are similar to those of anticholinergics and include drowsiness, dryness of the mouth, and constipation. Table 42.1 lists the nonprescription antiemetics used for vomiting caused by motion sickness. Diphenhydramine characteristics are explained in Prototype Drug Chart 35.1.
Several nonprescription drugs, such as bismuth subsalicylate, act directly on the gastric mucosa to suppress vomiting. They are marketed in liquid and chewable tablet forms and can be taken for gastric discomfort or diarrhea. Phosphorated carbohydrate solution, a hyperosmolar carbohydrate, decreases nausea and vomiting by changing the gastric pH; it may also decrease smooth-muscle contraction of the stomach. Its effectiveness as an antiemetic has not been verified. Patients with diabetes mellitus should avoid this drug because of its high sugar content.
Antiemetics that were once frequently used for the treatment of nausea and vomiting during pregnancy are no longer recommended because they may cause harm to the fetus. Instead, nonpharmacologic methods are used when possible to alleviate nausea and vomiting during pregnancy. Ginger and Red Raspberry leaf tea have been used effectively but are not regulated by the U.S. Food and Drug Administration (FDA). When antiemetics are necessary, a delayed release combination of pyridoxine and doxylamine is usually preferred. If vomiting becomes severe and threatens the well-being of the mother and fetus, an antiemetic such as promethazine or metoclopramide can be administered. Other antiemetics may be prescribed cautiously.
Prescription Antiemetics
Common prescription antiemetics are classified into the following groups: (1) antihistamines, (2) anticholinergics, (3) dopamine antagonists, (4) benzodiazepines, (5) serotonin antagonists, (6) glucocorticoids, (7) cannabinoids (for patients with certain diagnoses, such as cancer), and (8) miscellaneous. Many of these drugs act as antagonists to dopamine, histamine, serotonin, and acetylcholine, which are associated with vomiting. Antihistamines and anticholinergics act primarily on the vomiting center; they also act by decreasing stimulation of the CTZ and vestibular pathways. The cannabinoids act on the cerebral cortex. Phenothiazines, the miscellaneous antiemetics (e.g., metoclopramide), and trimethobenzamide act on the CTZ. Drug combination therapy is commonly used to manage chemotherapy-induced nausea and vomiting. Lorazepam, glucocorticoids, and serotonin (5-HT3)-receptor antagonists are quite effective in combination therapy. Lorazepam, haloperidol, and glucocorticoids are not approved by the FDA as antiemetics but are extremely effective when combined for this unlabeled use.
Antihistamines and Anticholinergics
Only a few prescription antihistamines and anticholinergics are used in the treatment of nausea and vomiting. Table 42.2 lists these drugs and their dosages, uses, and considerations.
Side Effects and Adverse Reactions
Side effects include drowsiness, which can be a major problem; dry mouth; blurred vision caused by pupillary dilation; tachycardia (with anticholinergic use); and constipation. These drugs should not be used by patients with glaucoma.
Dopamine Antagonists
These agents suppress emesis by blocking dopamine (D2) receptors in the CTZ. The categories of dopamine antagonists include phenothiazines, butyrophenones, and benzodiazepines. Common side effects of dopamine antagonists are extrapyramidal symptoms, or extrapyramidal syndrome (EPS), caused by blocking dopamine receptors, and hypotension. See Chapter 22 for a more detailed description of EPS and phenothiazines.
Phenothiazine Antiemetics
Selected piperazine phenothiazines are used to treat nausea and vomiting resulting from surgery, anesthetics, chemotherapy, and radiation sickness. They act by inhibiting the CTZ. When used in patients with cancer, these drugs are commonly given the night before treatment, the day of treatment, and for 24 hours after treatment. Not all phenothiazines are effective antiemetic agents. When prescribed for vomiting, the drug dosage is usually smaller than is used for psychiatric disorders.
Chlorpromazine and prochlorperazine edisylate were the first phenothiazines used for both psychosis and vomiting. Promethazine, a phenothiazine introduced as an antihistamine in the 1940s, has a sedative effect and can also be used for motion sickness and management of nausea and vomiting.
 When promethazine is administered intravenously, it is a high-alert medication that may cause significant harm to the patient if given incorrectly. Prototype Drug Chart 42.1 lists the pharmacologic data for promethazine.
When promethazine is administered intravenously, it is a high-alert medication that may cause significant harm to the patient if given incorrectly. Prototype Drug Chart 42.1 lists the pharmacologic data for promethazine.Pharmacokinetics
Promethazine is readily absorbed in the gastrointestinal (GI) tract. It has 80% to 93% protein-binding capacity. Promethazine is metabolized by the liver and is excreted in urine and feces.
Pharmacodynamics
Promethazine blocks H1-receptor sites on effector cells and impedes histamine-mediated responses. The onset of action of oral promethazine is 15 to 60 minutes, and onset with intramuscular (IM) administration is 20 minutes. The duration of action is from 4 to 6 hours. The onset of action of IV promethazine is 3 to 5 minutes; the duration of action is the same as for the oral preparation.
Drug and Laboratory Interactions
Central nervous system (CNS) depression increases when promethazine is taken with alcohol, narcotics, sedative-hypnotics, and general anesthetics. Anticholinergic effects increase when promethazine is combined with antihistamines, anticholinergics such as atropine, and other phenothiazines. Promethazine may interfere with urinary pregnancy tests, producing false results.
Side Effects and Adverse Reactions
Phenothiazines have antihistamine and anticholinergic properties. The side effects of phenothiazine antiemetics are moderate sedation, hypotension, extrapyramidal symptoms, CNS effects (restlessness, weakness, dystonic reactions, agitation), and mild anticholinergic symptoms (dry mouth, urinary retention, and constipation). Because the dose is lower for vomiting than for psychosis, the side effects are not so severe. Promethazine is relatively free of extrapyramidal symptoms at antiemetic doses. Table 42.2 lists the pharmacologic data for phenothiazines and other prescription antiemetics.
Butyrophenones
Haloperidol and droperidol, like phenothiazines, block the D2 receptors in the CTZ. They are used to treat postoperative nausea and the vomiting and emesis associated with toxins, cancer chemotherapy, and radiation therapy. Antiemetic doses of haloperidol are smaller than those required for antipsychotic effects. Like phenothiazines, haloperidol and droperidol are likely to cause extrapyramidal symptoms if used for an extended time. Hypotension may result, therefore blood pressure should be monitored.
Benzodiazepines
Select benzodiazepines indirectly control nausea and vomiting that may occur with cancer chemotherapy. Lorazepam is the drug of choice. Previously, diazepam was the preferred benzodiazepine, but lorazepam effectively provides emesis control, sedation, anxiety reduction, and amnesia when used in combination with a glucocorticoid and serotonin (5-HT3)-receptor antagonist.
Serotonin-Receptor Antagonists
Serotonin antagonists suppress nausea and vomiting by blocking the serotonin (5-HT3) receptors in the CTZ and blocking the afferent vagal nerve terminals in the upper GI tract.
Serotonin antagonists—ondansetron, granisetron, dolasetron, and palonosetron—are the most effective of all antiemetics in suppressing nausea and vomiting caused by cancer chemotherapy–induced emesis or emetogenic anticancer drugs. Ondansetron (the first serotonin antagonist), granisetron, and dolasetron do not block the dopamine receptors, therefore they do not cause extrapyramidal symptoms as do the phenothiazine antiemetics. These drugs can be administered orally and intravenously. They are also effective in preventing nausea and vomiting before and after surgery. Common side effects include headache, diarrhea, dizziness, and fatigue.
Glucocorticoids (Corticosteroids)
Dexamethasone and methylprednisolone are two agents that are effective in suppressing emesis associated with cancer chemotherapy. Because these glucocorticoids are administered intravenously and for only a short while, side effects normally associated with glucocorticoids are minimized. Glucocorticoids are discussed in Chapter 46.
Cannabinoids
Cannabinoids, the active ingredients in Cannabis, were approved for clinical use in 1985 to alleviate nausea and vomiting resulting from cancer treatment. These agents may be prescribed for patients receiving chemotherapy who do not respond to or are unable to take other antiemetics. They are contraindicated for patients with psychiatric disorders. Cannabinoids can be used as an appetite stimulant for patients with acquired immunodeficiency syndrome (AIDS). The cannabinoid dronabinol is described in Table 42.2.
Side Effects and Adverse Reactions
Side effects that can occur as a result of cannabinoid use include mood changes, euphoria, drowsiness, dizziness, headaches, depersonalization, nightmares, confusion, incoordination, memory lapse, dry mouth, orthostatic hypotension or hypertension, and tachycardia. Less common symptoms are depression, anxiety, and manic psychosis.
Miscellaneous Antiemetics
Trimethobenzamide is in the class of miscellaneous antiemetics because it does not act strictly as an antihistamine, anticholinergic, or phenothiazine. The drug suppresses impulses to the CTZ.
Side Effects and Adverse Reactions
The side effects and adverse reactions of the miscellaneous antiemetics are drowsiness and anticholinergic symptoms such as dry mouth, increased heart rate, urine retention, constipation, and blurred vision. Trimethobenzamide can cause hypotension, diarrhea, and extrapyramidal symptoms that include abnormal involuntary movements, postural disturbances, and alterations in muscle tone.
Metoclopramide
Metoclopramide suppresses emesis by blocking the dopamine receptors in the CTZ. It is used in the treatment of postoperative emesis, cancer chemotherapy, and radiation therapy. High doses can cause sedation and diarrhea. With this agent, the occurrence of extrapyramidal symptoms is more prevalent in children than in adults. Metoclopramide should not be given if the patient has GI obstruction, hemorrhage, or perforation.
Table 42.2 lists pharmacologic data for the miscellaneous antiemetics along with other prescription antiemetics.