• Benign breast discomfort: conditions present in most women of reproductive age should never be labeled pathologic. Misconception: women with painful or lumpy breasts have increased breast cancer risk. Premenstrual pain and sensitivity is common; more prominent estrogen than progesterone effect at this time, when effect of progesterone is normally greater in luteal phase. This does not mean lower or higher levels of any particular hormone, but increased tissue sensitivity to estrogen with related fluid retention. This discomfort is tolerable in most women. Others need lifestyle changes or supplements. Oral contraceptives or hormone replacement therapy may cause breast discomfort: physiological, cyclical pain and swelling. • Mastalgia: breast pain of severity interfering with daily life and prompting medical attention. Cyclical mastalgia is this severe 15% of the time. Noncyclical is rarer, caused by infection, old trauma, musculoskeletal conditions of chest wall. • Diffuse lumpiness: cyclic or noncyclic and may or may not include pain. Normal breasts can have diffuse lumpiness—glands, fat, connective tissue. Prominent lumpiness and numerous lumps distinguish this from normal. Diffuse lumpiness is symmetric, distinguishing a normal from suspicious lump. • Unilateral densities: most are benign. If mass edge merges in one or more places with surrounding tissue, it is nondominant. Evaluate masses carefully to distinguish dominant mass or mass • Dominant masses: noncyclical, unilateral, distinct on all sides from surrounding tissue. They persist over time and require thorough assessment, except in the very young. They are either fibroadenomas or obvious cysts. Fibroadenomas are rubbery, smooth, benign, fibrous tumors that usually do not grow bigger. Cysts are softer and disappear by draining with needle aspiration. Fibroadenomas and cysts do not increase risk but must be distinguished from malignancy. See the Textbook, “Premenstrual Syndrome,” for additional factors that can influence FBD. • Methylxanthines: caffeine, theophylline, and theobromine in-hibit action of cyclic adenosine monophosphate (cAMP) and cyclic guanosine monophosphate (cGMP) phosphodiesterase and elevate their levels in breast tissue. Increased cyclic nucleotides excessively stimulate protein kinase, causing overproduction of cellular products (fibrous tissue, cyst fluid). Excess cyclic nucleotides in breast are one of the biochemical findings in breast cancer; caffeine promotes carcinogenesis in mammary gland of rats. Limiting dietary methylxanthines (coffee, tea, cola, chocolate, caffeinated medicines) improved 97.5% of 45 women who completely abstained and 75% of 28 who limited con-sumption. Women may have varying thresholds of response to methylxanthines. Stress plays a role; fibrocystic breasts are more responsive to epinephrine, which increases adenylate cyclase activity (cAMP). • Fiber: an inverse association exists between dietary fiber and risk of benign, proliferative, epithelial breast disorders. Fiber may reduce risk of benign breast disease and cancer. • Soy: in premenopausal women consuming soy protein daily for 1 year, their physicians reported subjective reduction in breast tenderness and FBD by using breast-enhanced scintigraphy test imaging. Average and maximal count breast activity and variability of tissue activity declined.
Fibrocystic Breast Disease
GENERAL CONSIDERATIONS
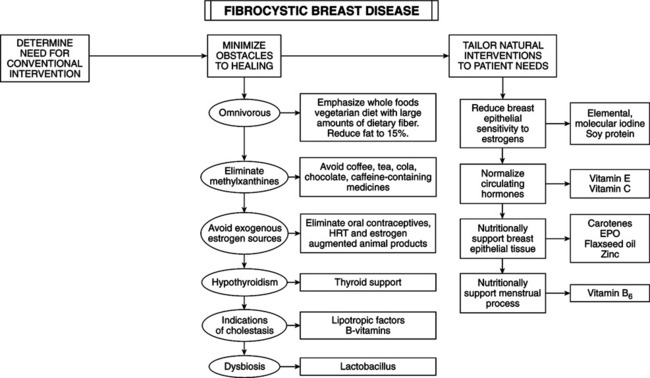
THERAPEUTIC CONSIDERATIONS
Dietary considerations
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fibrocystic Breast Disease
