Patient Story
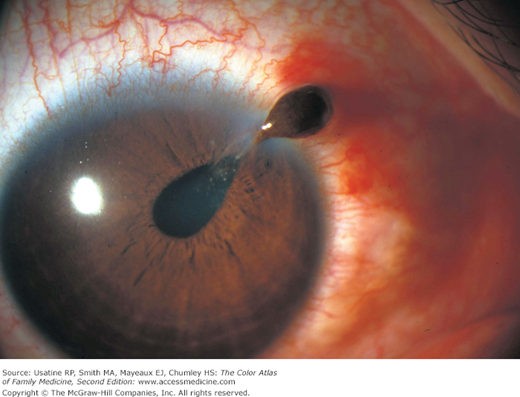
A 22-year-old man was hit in the eye with a baseball and presented to the emergency department with eye pain and redness and decreased visual acuity. There was a collection of blood in his anterior chamber (Figure 24-1) and he was diagnosed with a hyphema. He was given an eye shield for protection, advised to take acetaminophen for pain, and counseled not to engage in sporting activities until his hyphema resolved. He saw his physician daily for the next 2 days, during which his vision improved. His hyphema resolved in 5 days.
Introduction
Hyphema, blood in the anterior chamber, can be seen following eye trauma or as a result of clotting disturbances, vascular abnormalities, or mass effects from neoplasms. Traumatic hyphema occurs more often in boys and men, often related to work or sports. Hyphema typically resolves in 5 to 7 days, but some cases are complicated by rebleeding.
Epidemiology
- Hyphema occurs in 17 to 20 per 100,000 persons per year in the United States.1
- Sixty percent of hyphemas result from sports injuries.2 Sports with higher risk for eye injuries include paintball, baseball/softball, basketball, soccer, fishing, ice hockey, racquet sports, fencing, lacrosse, and boxing.
Etiology and Pathophysiology
- A hyphema is a collection of blood, mostly erythrocytes, that layer within the anterior chamber.
- Trauma is the most common cause, often resulting from a direct blow from a projectile object such as a ball, air pellet or BB, rock, or fist.
- Direct force to the eye (blunt trauma) forces the globe inward, distorting the normal architecture.
- Intraocular pressure rises instantaneously causing the lens/iris/ciliary body to move posteriorly, thus disrupting the vascularization with resultant bleeding.
- Intraocular pressure continues to rise and bleeding stops when this pressure is high enough to compress the bleeding vessels.
- A fibrin-platelet clot forms and stabilizes in 4 to 7 days; this is eventually broken down by the fibrinolytic system and cleared through the trabecular meshwork.
Diagnosis
The diagnosis of hyphema is clinical, depending on the classic appearance of blood layering in the anterior chamber.
History and physical:
- Layered blood in the anterior chamber.
- History of eye trauma or risk factor for nontraumatic hyphema.
- Increased intraocular pressure (32%).
- Decreased vision.
- Hyphemas are classified according to the amount of blood in the anterior chamber:1
- Grade 1: Less than one-third of the anterior chamber (see Figure 24-1); 58% of all hyphemas.
- Grade 2: One-third to one-half of the anterior chamber; 20% of all hyphemas.
- Grade 3: One-half to almost completely filled anterior chamber; 14% of all hyphemas.
- Grade 4: Completely filled anterior chamber; 8% of all hyphemas.
- Grade 1: Less than one-third of the anterior chamber (see Figure 24-1); 58% of all hyphemas.
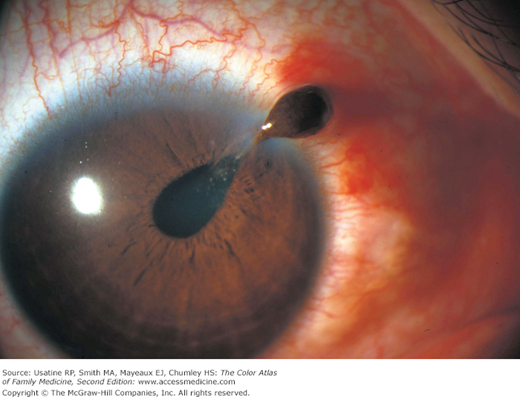
- Eye trauma without hyphema (Figure 24-2 and 24-3) can lead to subconjunctival hemorrhage, anterior uveitis, and/or distortion of the normal architecture, including globe rupture.
Figure 24-2
This young patient was hit in the eye with the corner of a laminated name card. The sharp edge perforated the cornea and pulled a portion of the iris out of the wound. Note the abnormal configuration of the pupil (dyscoria). No hyphema noted. This patient required emergent surgical repair. (Reprinted with permission from Lo MW, Chalfin S. Retrobulbar anesthesia for repair of ruptured globes. Am J Ophthalmol. 1997;123(6):833-835. Photo by Paul D. Comeau.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree