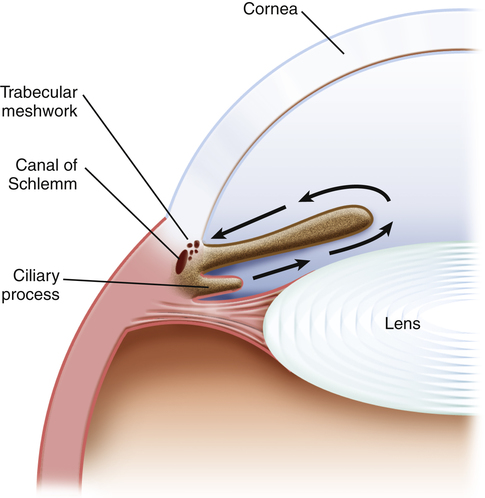
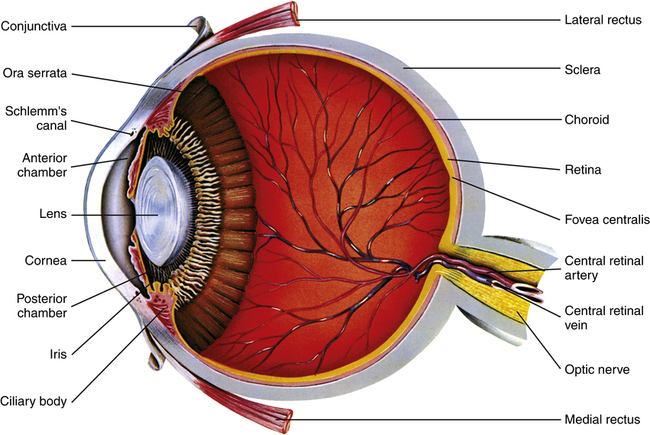
Chapter 14 The eye is protected by the tear film, which covers the cornea and conjunctiva, up to the lid margins; it provides moisture, lubrication, oxygen, and protective chemicals, including cytokines. Tears are regularly distributed over the lens by blinking of the eyelid. Tears drain through the puncta at the lid margins (Figure 14-1), into the lacrimal ducts and sac, then to the nasolacrimal duct and to the nose. Medications in the tears may be systemically absorbed through the nasal and pharyngeal mucosa. Figure 14-2 shows the internal anatomy of the eye. The conjunctiva covers the inside of the eyelids and the cornea. Aqueous humor is produced by the ciliary body. Excess humor drains through the canals of Schlemm in the trabecular meshwork. • Sympathomimetics and vasoconstrictors are OTC agents that are commonly used for relief of red, irritated eyes. Generally, they are safe and effective. However, chronic use is discouraged because of rebound inflammation. • Ocular lubricants (i.e., artificial tears) are also OTC agents. They are also very safe and effective in relieving irritated eyes. They are used in elderly patients and in those who are on medications that cause dry eyes. • Fluorescein is used in the primary care setting when the eye is examined for abrasions or foreign bodies. When the strips are used, they should be moistened with sterile water. Place the moistened strip at the fornix in the lower cul-de-sac close to the punctum of the eye. The patient should then blink several times. Allow a few seconds for staining. An injury will show up as an intense green fluorescent color. Rinse out the eye with sterile irrigating solution. • The American Academy of Ophthalmology has Preferred Practice Patterns for many ophthalmology problems. The guidelines for conjunctivitis are reflected in this discussion. See http://one.aao.org. 1. Diagnose the cause of conjunctivitis. 2. Ophthalmic antibiotics are effective for bacterial conjunctivitis and are commonly used to prevent secondary bacterial infection in viral conjunctivitis. Effective treatment demands accurate diagnosis. Primary care providers collect pertinent information and begin the process of diagnosis. However, many problems require referral to a specialist for care. See Table 14-1 for evaluation and management of potentially serious eye problems. TABLE 14-1 Evaluation and Management of Potentially Serious Eye Problems
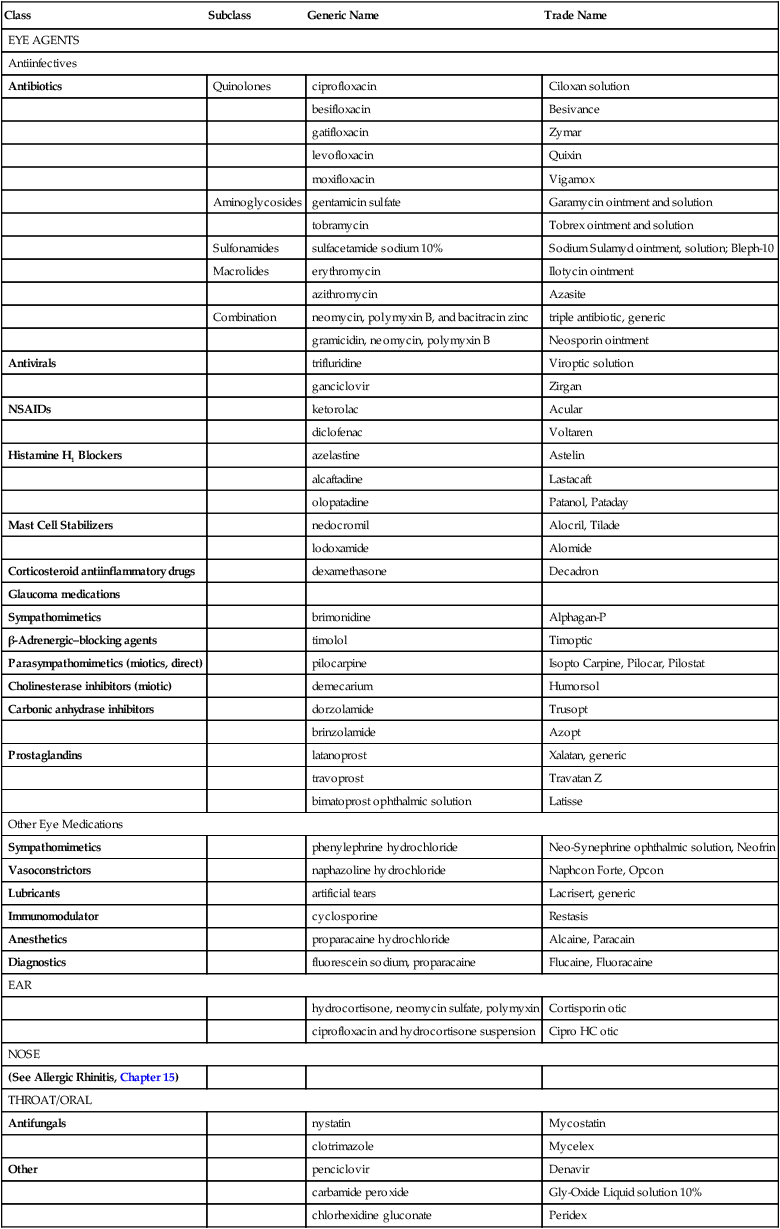
Eye, Ear, Throat, and Mouth Agents
Class
Subclass
Generic Name
Trade Name
EYE AGENTS
Antiinfectives
Antibiotics
Quinolones
ciprofloxacin
Ciloxan solution
besifloxacin
Besivance
gatifloxacin
Zymar
levofloxacin
Quixin
moxifloxacin
Vigamox
Aminoglycosides
gentamicin sulfate
Garamycin ointment and solution
tobramycin
Tobrex ointment and solution
Sulfonamides
sulfacetamide sodium 10%
Sodium Sulamyd ointment, solution; Bleph-10
Macrolides
erythromycin
Ilotycin ointment
azithromycin
Azasite
Combination
neomycin, polymyxin B, and bacitracin zinc
triple antibiotic, generic
gramicidin, neomycin, polymyxin B
Neosporin ointment
Antivirals
trifluridine
Viroptic solution
ganciclovir
Zirgan
NSAIDs
ketorolac
Acular
diclofenac
Voltaren
Histamine H1 Blockers
azelastine
Astelin
alcaftadine
Lastacaft
olopatadine
Patanol, Pataday
Mast Cell Stabilizers
nedocromil
Alocril, Tilade
lodoxamide
Alomide
Corticosteroid antiinflammatory drugs
dexamethasone
Decadron
Glaucoma medications
Sympathomimetics
brimonidine
Alphagan-P
β-Adrenergic–blocking agents
timolol
Timoptic
Parasympathomimetics (miotics, direct)
pilocarpine
Isopto Carpine, Pilocar, Pilostat
Cholinesterase inhibitors (miotic)
demecarium
Humorsol
Carbonic anhydrase inhibitors
dorzolamide
Trusopt
brinzolamide
Azopt
Prostaglandins
latanoprost
Xalatan, generic
travoprost
Travatan Z
bimatoprost ophthalmic solution
Latisse
Other Eye Medications
Sympathomimetics
phenylephrine hydrochloride
Neo-Synephrine ophthalmic solution, Neofrin
Vasoconstrictors
naphazoline hydrochloride
Naphcon Forte, Opcon
Lubricants
artificial tears
Lacrisert, generic
Immunomodulator
cyclosporine
Restasis
Anesthetics
proparacaine hydrochloride
Alcaine, Paracain
Diagnostics
fluorescein sodium, proparacaine
Flucaine, Fluoracaine
EAR
hydrocortisone, neomycin sulfate, polymyxin
Cortisporin otic
ciprofloxacin and hydrocortisone suspension
Cipro HC otic
NOSE
(See Allergic Rhinitis, Chapter 15)
THROAT/ORAL
Antifungals
nystatin
Mycostatin
clotrimazole
Mycelex
Other
penciclovir
Denavir
carbamide peroxide
Gly-Oxide Liquid solution 10%
chlorhexidine gluconate
Peridex
Eye Agents
Therapeutic Overview of Eye Agents
Anatomy, Physiology, and Pathophysiology
Tears drain through the puncta at the lid margins, into the lacrimal ducts and sac, then to the nasolacrimal duct and to the nose. (From Thibodeau GA, Patton KT: Anatomy & physiology, ed 7, St Louis, 2010, Mosby.)
Other Eye Problems
Treatment Principles
Standardized Guidelines
Cardinal Points of Treatment
Complaint or Problem
Suggested Treatment
EMERGENCIES
Chemical burn
Irrigate eye for 15-20 min; send to emergency department.
Retinal artery occlusion with sudden, painless loss of vision in one eye
Must be seen by specialist within 90 min to preserve vision
“Something in eye”
Check visual acuity in each eye, document findings; if significant loss of vision or blurring, refer patient to specialist.
Examine eye for foreign body: Evert eyelid, and if a foreign body is seen, do not irrigate, but flick off with a needle; if fine powder, irrigate.
Stain with fluorescein dye to check integrity of epithelial surface; moisten strip if eye is dry, touch strip to inner conjunctival surface, let patient blink, then shine flashlight (blue filter preferred); epithelial break stains green, refer to specialist.
Red eye
Check vision; if vision is decreased, refer to specialist.
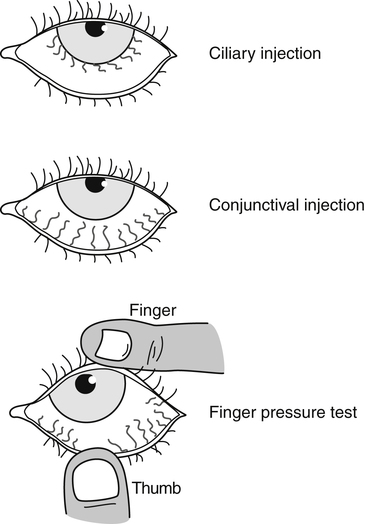
Check injection, use finger pressure test to determine whether conjunctival or ciliary (Figure 14-3); press lower lid against cornea, draw downward; conjunctiva should blanch; ciliary injection is around the limbus, does not blanch; if ciliary injection, refer to specialist.
CONTACT LENSES
Symptoms: Lens wearers are at risk for corneal abrasion and infection and for hypoxic corneal injury.
If patient complains of pain, remove contact lens, check for abrasion with fluorescein dye, refer to specialist.
CORNEAL ABRASIONS
Symptoms: pain, foreign body sensation, photophobia, tearing, or blepharospasm immediately after insertion or removal of contact lens or from direct trauma to the eye from projected particles
Remove contact lens, stain eye with fluorescein dye, remove foreign body if present; topical antibiotic may be required; refer to specialist.
Signs: epithelial defect confirms corneal abrasion; may become infected and progress to corneal ulceration
HYPOXIC CORNEAL INJURY
Symptoms: during contact lens wear, blurred vision, conjunctival hyperemia, pain
Remove contact lens, stain with fluorescein dye, evaluate, and refer to specialist if necessary.
Signs: conjunctival hyperemia and ciliary flush, contact lens immobility, diffuse corneal edema; may lead to corneal neovascularization and scarring
Conjunctivitis
Diagnostic cultures generally not necessary
Treat with antibiotics: Use a broad-spectrum drug or one that covers gram-positive organisms; refer if not resolved in 7 days.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Eye, Ear, Throat, and Mouth Agents
Only gold members can continue reading. Log In or Register to continue