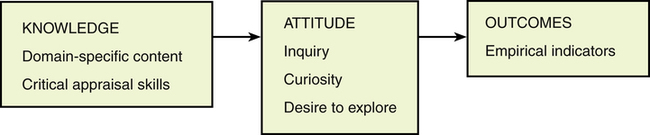
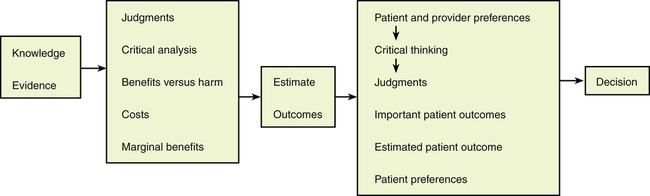
Chapter 11 D.M. Eddy, one of the long-term writers to dominate the field of critical thinking, observed that the quality of health care is determined by two main factors: the quality of the decisions that determine what actions are taken, and the quality with which those actions are executed—what to do and how to do it. If the wrong actions are chosen, no matter how skillfully they are executed, the quality of care will suffer. Similarly, if the correct actions are chosen but the execution is flawed, the quality of care will suffer (Eddy, 1990). Health care requires clinicians who can make decisions autonomously. It is therefore essential that health care providers consciously strive to develop effective problem-solving and decision-making skills (Edwards, 2007). The intrusion of insurance plans and public health programs, restricted formularies, electronic health records, and managed care into clinical practice means that resources for health care clinicians are restricted. The presence of many patients without any insurance or who are underinsured affects clinical decision making in a practice. Ordering multiple tests to rule in or rule out various disease states is not an option, but not doing so may increase the risk for liability. More than ever before, health care providers must learn critical thinking skills in making proper clinical judgments. So the question becomes “How do we individually and collectively ensure that higher-level thinking is engaged for health care problem solving?” (Ellerman et al, 2006). Benjamin S. Bloom’s seminal work in 1956 on the original taxonomy of educational objectives for the cognitive domain does not contain the term decision making. However, each of the two higher cognitive domains—synthesis and evaluation—contains verbs that involve planning, composing, designing, constructing, creating, setting up, organizing, appraising, evaluating, comparing, revising, and assessing—all components of the decision-making process as recognized in the 2000 revision of that taxonomy (Anderson et al, 2000). Much of the initial research about critical thinking in clinical settings was completed in the 1980s and 1990s by nurses. Much of the early work was conducted by nursing faculty as they prepared for National League for Nursing program accreditation. This early work by nurses and not by physicians informs the literature on critical thinking. These early writers agree that critical thinking involves dimensions of logic, problem solving (Beyer, 1985), and scientific inquiry, and might be defined as “careful, deliberate, goal-directed thinking based on principles of science and the scientific method” (Bandman & Bandman, 1995). Clearly, the construct of critical thinking is not a set body of knowledge but rather a nonlinear dynamic process (Jacobs et al, 1997); it is not an outcome. Watson and Glaser (1964) dominated the literature about critical thinking in nursing, arguing that it has two basic components: knowledge and an attitude of inquiry. Knowledge includes knowledge of the domain-specific subject matter and knowledge of specific mental operations or critical thinking skills. Attitude denotes frame of mind or an attitude of inquiry, curiosity, and willingness or desire to examine and explore the problem. This component is uniquely developed in each individual and results from the health care provider’s personality and culturally determined behavioral norms. However, knowledge and an attitude of inquiry alone do not capture true critical thinking. The thinker must critically appraise knowledge. This component of thinking allows the thinker to apply, synthesize, and evaluate what is known and, as such, brings critical thinking into the highest cognitive domain. This process of critical thinking is outlined in Figure 11-1. As can be seen from this figure, the clinician’s knowledge is key. Clearly, the beginning student or novice will have less knowledge than the expert. This is particularly true in clinical practice fields like medicine and nursing. However, health care provider students do not have minds as empty as blank pages. They have information from previous courses and experiences. RNs returning to school for nurse practitioner (NP) education may have had years of successful clinical practice, although increasingly there are nursing to DNP programs, so the student NP may have had very little or no previous clinical experience as a nurse. Many older nurse or PA students have had other careers before they turned to health care. All these students have some knowledge but need additional information that is evaluated and then organized so it becomes usable. Early researchers suggested that the mind might be thought of as a series of matrices in which information is stored. The matrix is entered and information is retrieved as the individual recognizes patterns, sees similarities, recognizes what is important, generalizes, and uses common sense (Gerdeman, Lux, & Jacko, 2012). Research into the critical thinking that a clinician uses in diagnostic reasoning and problem solving suggests two different theories of clinical expertise. The first theory proposes that experts perform better than novices because they have better problem-solving strategies. The alternative theory suggests that experts perform better because they have more knowledge. Current evidence in the literature supports the latter position—that clinical expertise is largely a function of domain-specific knowledge (Elstein et al, 1990; Lange et al, 1997). For example, several researchers have found that the diagnostic strategies used by experts and novices are very similar. Norman and colleagues argue that experts do not possess any innate or learned advantage in problem-solving techniques. Rather, experts solve problems better because they know more in their domains than novices do, and problem-solving expertise generalizes somewhat within a domain of medical knowledge (e.g., rheumatology) but does not necessarily generalize to other domains (e.g., pulmonary, cardiology) (Norman et al, 1985). This early research has now been substantiated by additional clinical research (Cockcroft, 2007; Hadley et al, 2007; Morey, 2012). In other situations, schemata, algorithms, or mental models have been used in decision making. These are all abstract representations of information gained from experience, and they assist us in understanding the world and the reality in which people exist. The foundational research of Benner (1984) and Benner and Tanner (1987) emphasize the place of experience in the quality of thinking. New trends look at reflective journaling and structural conditions to facilitate critical thinking (Martensson et al, 2012; Schuessler, Wilder, & Byrd, 2012). Although much of critical thinking and clinical decision making may be related to natural curiosity and intelligence, some attributes (steps or tools) tend to make thinking more complete. Describe the importance of preceptor questioning in helping students think critically. If clinicians have knowledge, then it is important to observe what they do with that knowledge so one can determine the extent of critical thinking that is taking place (Martensson et al, 2012; Sullivan, 2012). Some observable behaviors of critical thinkers have been identified as the ability to do the following: • Distinguish between observation and inference, and facts and claims • Determine the reliability of a claim or source • Evaluate the accuracy of statements • Differentiate relevant from irrelevant data • Differentiate between warranted and unwarranted claims • Recognize ambiguous or equivocal claims/arguments • Discern inconsistencies in reasoning • Identify an argument’s strength An additional way of determining whether critical thinking has taken place is to look at the outcomes of the critical thinking process (Box 11-1). Lack of knowledge, problems in attitude, and flaws in critical appraisal may result in defective thinking. For example, one may have good knowledge of a subject but may be inflexible or unwilling to consider other options or points of view. Likewise, the individual may have curiosity, motivation, and interest but may lack the knowledge necessary to develop alternatives and to consider options (Banfield, Fagan, & James, 2012; Riddell, 2007; Turner, 2007). In exploring how people make decisions, nursing has focused almost exclusively on the process of critical thinking, whereas the medical literature is filled with research on diagnostic and clinical decision making. Reports suggest that in most medical schools, when clinical reasoning is taught, this is provided as an add-on and is not continued as an integral component in the rest of the courses. Because of this lack of curricular integration, one of the early writers on medical decision making concluded that special courses in clinical reasoning appear to have a marginal effect (Chessare et al, 1996). The general focus of most medical curricula is on acquisition of knowledge. How to search for and critically evaluate evidence is a skill that is generally addressed superficially, if at all. Some of the research findings of the past 20 years about decision making of nurses are provocative. Findings suggest that many nurses are action oriented, resulting in a focus on action rather than on analysis of all relevant data. A study based on NP students found that they often attempted to formulate a diagnosis too early in the decision-making process. Almost all of the NP students had practiced as staff nurses in acute care settings, where rapidly formulating a diagnosis was important. Although that manner of clinical decision making was successful for experienced clinicians, for inexperienced NP students, formulating hypotheses too early often resulted in incomplete assessments (Lipman & Deatrick, 1997). Thus, skills that had helped students as RNs were counterproductive in the new role without a broader knowledge base. Research suggests that much of the confusion that is seen in some NP students early in their program can be attributed to a reworking of decision-making and critical-thinking skills. The NP program asks students to take their existing domain-specific knowledge acquired as an RN in which they have “expert” skills and use it to process information in new ways and to exhibit different behaviors. It appears that asking them to do this temporarily suspends use of their previously learned skills. (Another explanation proposed for this phenomenon is that NPs are inhibited by their return to a setting in which they must undergo intense scrutiny of their performance by preceptors/faculty members as they attempt to use newly acquired knowledge and skills [Roberts et al, 1997].) What some faculty members have begun to accept is that combining a nursing education foundation with advanced medical information may require a paradigm shift for the student, prompting reorganization of existing knowledge and critical thinking skills, and not just the addition of new knowledge. In this paradigm shift, NP students must move to a new developmental stage that allows them to recognize the limitations of their existing knowledge and must learn how to acquire needed knowledge to assume increased responsibility for their own judgment and decisions. Simply put, the problem for NP students is probably the result of “taking an expert and asking [him] to be a novice again” (Roberts et al, 1997). Some of these same problems may apply to older students who worked in other disciplines and are now turning to nursing or PA programs. The medical literature abounds with reports on decision making and the development of diagnostic skills. One of the best authors to bring together the various theories and ideas has been Eddy (1990, 2005, 2007; Eddy et al, 2011). Eddy suggests that, in general, the goal of a health care decision maker is to choose an action that is most likely to deliver the outcomes the patient wants. Eddy goes on to identify the two main steps involved in making a clinical decision. First, the outcomes of the different options must be estimated; then, the desirability of the outcomes of each option must be compared. “The first step involves collecting and analyzing whatever evidence exists regarding the benefits, harms, and costs of each option. Because the available evidence is virtually never perfect or complete, this step will also involve some subjective judgment” (Eddy, 2005). For example, should a patient with a prostatic mass continue to be monitored, have chemotherapy, or undergo surgery? The resulting estimates of that analysis then form the basis for the second step. Three types of comparisons are required in the second step: (1) The benefits of a practice must be compared with the harms (e.g., risks, side effects, inconvenience, length of disability, anxiety); (2) the health outcomes must be compared with the costs; and (3) if it is not possible to do everything because of limited resources, the amount of benefit gained and the resources consumed must be compared with those of other options so that priority will be given to options that have the highest yield (Eddy, 2005) (Figure 11-2). No matter how explicitly, how consciously, or how correctly each of these steps is performed, these factors must be considered every time a decision is made regarding a health practice. This is true whether the decision is made by an individual clinician, whether a group of health care providers are recommending a guideline for a group of patients, or whether third-party payers are setting coverage policy. Learning in a setting where there are other health care providers often facilitates collaborative practice and thinking (Kramer et al, 2012). To appreciate this, imagine trying to advise a patient regarding the merits of a health practice without considering any evidence of its effects or the magnitude of the benefit or harm caused by the practice, and without caring whether the benefit outweighs the harm. Anyone who makes a responsible decision regarding a health practice must have some idea, however uncertain, of the evidence that justifies its use, of its consequences, and of its desirability. It is important to separate the decision-making process into these two steps for several reasons. Specifically, Eddy’s two steps involve different thought processes, have different anchors, and might be performed by different people. In addition, different degrees of agreement about the results can be expected. The first step is to agree on the facts. The anchor is empirical evidence. The process is a scientific one that involves experiments, analysis of evidence, and forecasting. The required skills are analytic. Finally, assuming there is some evidence to evaluate, it should be possible to get reasonable, open-minded people to agree on the results of this step (Eddy, 2005). Returning to Eddy’s model, the second step is to clarify the personal values or preferences of the patient. The move to managed care and the recognition that the patient has rights as a consumer of care with resultant restriction on resources have served to highlight the necessity of joint decision making between the patient and the clinician. The thought process is not analytic but personal and subjective; it is an appeal not to the left side of the brain but to the right side of the brain, or even the gut. Different people can properly have different preferences. There is no single correct answer, and there is no obligation that everyone must agree (Eddy, 2007). Now, we are getting to the art of medicine. To the extent that science is involved in this step at all, it is the science of discovering people’s preferences—through polls, questionnaires, and focus groups—that is involved. Perhaps most important, the people whose preferences count are the patients, because they are the ones who will have to live (or die) with the outcomes. Others might intervene if an individual’s decision is based on inaccurate information (e.g., insistence on antibiotic therapy for a viral upper respiratory tract infection), is illegal (e.g., drug abuse), or harms a public interest (e.g., refusal of control measures for an infectious disease), or when the patient is not competent enough to make a decision. However, assuming these complications do not apply, it is the patient’s preferences that should determine the decision (Eddy, 2007). Eddy’s later research has focused on how individualizing recommended guidelines actually can increase quality and reduce costs (Eddy et al, 2011). In one of the classic research studies of how expert clinicians make clinical diagnoses, Elstein and colleagues (1990) proposed that expert physicians generate specific diagnostic hypotheses well before the time that they gather most of the data for a particular case. Rather than progressively and systematically converging on a diagnosis through a series of constraining questions, experienced physicians appear to leap directly to a small array of provisional hypotheses very early in their encounter with the patient. These provisional hypotheses are generated out of the physicians’ background knowledge of medicine, including their range of specific experiences, in conjunction with the problematic elements recognized in the early stages of encounter with the patient. • Attending to initially available cues • Identifying problematic elements from among these cues and searching long-term memory • Generating hypotheses and suggestions for further inquiry • Informally rank-ordering hypotheses according to the physician’s subjective estimates Rank ordering is based on the physician’s evaluation of probability (estimates closely approximate the population base rate for a disease), seriousness (life-threatening or incapacitating conditions are ranked higher than their population base rate warrants), treatability (a treatable problem is ranked higher so that any treatment that might possibly be helpful will not be overlooked), and novelty (the uniqueness of the problem keeps the physician interested in the case and ensures that unlikely avenues are explored, thus protecting the patient from the physician’s premature closure on a more generally probable hypothesis that, in a particular case, might be in error) (Elstein et al, 1990). The work of Benner (1984) remains one of the foremost accomplishments in describing the passage of a nurse from novice to expert and in detailing the ways in which nurses with varying levels of experience function. Benner’s (1984) seminal work describes the process of skill acquisition by nurses, indicating a developmental approach to decision making, commencing with decision analysis and progressing to hypothetical-deductive reasoning, with the eventual emergence of the expert who functions at an intuitive level. Later, Benner and Tanner (1987) examined the effects of intuition on an expert nurse’s ability to make clinical decisions. They identified the following six key aspects of intuitive judgment: 1. Pattern recognition—recognition of relationships 2. Similarity recognition—recognition of relationships despite obvious differences 3. Commonsense understanding—having a deep understanding of a given entity 4. Skilled know-how—ability to visualize a situation 5. Sense of salience—ability to recognize what is important These six aspects are seen to work in synergy in expert practice and not as solo components of behavior. These aspects are remarkably similar to the reported ways in which hypotheses are generated by expert physicians (Elstein et al, 1990). In teaching critical decision making, the new guiding principle for teacher–learner interactions might be embodied in the question “What’s the evidence?” This new guiding principle must permeate didactic lectures, discussions on rounds, and case-based sessions. The faculty become more coach than teacher. New curricula must foster the development of analytic skills in a more purposive manner (Chessare et al, 1996). Some of the specific competencies that should be taught are summarized in Table 11-1. TABLE 11-1 Specific Curricular Content to Enhance Critical Analysis for Problem Solving Modified from Chessare JB et al: Impact of a medical school course in clinical epidemiology and health care systems, Med Teach 18:227-233, 1996. It seems clear that diagnostic errors may occur among both experts and novices as a result of inadequate information processing. In Kassirer and Kopelman’s important work (1989), diagnostic errors were classified into four major types: It also must be acknowledged that diagnostic errors can result because the information-processing capacities of both experts and novices are limited. The short-term memory capacity of the human information-processing system is considerably less than its capacity for long-term memory storage. Thus, unstructured inputs of large amounts of information can quickly overload the system. Even in simple medical cases, the range of facts to be considered is large compared with the number of items (typically five to seven) about which humans can simultaneously think. “Provisional diagnoses or hypotheses formed early in the patient encounter serve as organizers or bases for chunking in data collection, keeping to a manageable number of categories under which information is filed” (Elstein et al, 1990). This strategy of organizing large numbers of facts into smaller numbers of clusters leads to the development of automatic, well-learned information management processes (Allen et al, 2004; Young et al, 2007). In diagnostic reasoning, these clusters of information may assume the form of causal models that are based on pathophysiologic relationships, epidemiologic principles, or schematic algorithms. However, although such heuristics may simplify diagnostic decision making, they also may lead to diagnostic errors (Kempainen et al, 2003). The main sources of error in medical decision making correspond to the two main steps in Eddy’s (1990) model: “A decision can be flawed either if there is a misperception of the outcomes or if there is a misperception of the values that patients place on the outcomes.” Most misperceptions result from failure of critical thinking. See Table 11-2 for a summary of common misperceptions that distort clinical decision-making accuracy. TABLE 11-2 Sources of Error in Clinical Decision Making Modified from Eddy DM: Anatomy of a decision, JAMA 263:441-443, 1990.
Evidence-Based Decision Making and Treatment Guidelines
Critical Decision Making
Critical Thinking
Decision Making
General Content to Be Included in Curricula
Specific Content
Basic tools of clinical epidemiology
Rates, incidence, prevalence, risk assessment, diagnostic test characteristics, and reproducibility of diagnostic information
Rules of evidence and research methods
Knowledge of research methods and assessment of causality, demonstrated knowledge of the hierarchy of research designs to avoid bias and confounding, and the strengths and weaknesses of each design
Hypothetical-deductive reasoning process
The science of decision making and the hypothetical-deductive reasoning process
Biases and heuristics
Learning about incumbent biases and mental shortcuts of heuristic thinking
Uncertainty and probabilistic thinking
Ways to minimize error in judgment and probabilistic thinking
Incorporating the patient’s values into medical decisions
Decision analysis
Medicine for populations
Policy analysis, cost-effectiveness analysis
Sources of Error
Examples
Misperception of the outcomes
Important outcomes may be ignored.
Extraneous outcomes might be included.
Available evidence regarding outcomes may be incomplete.
Existing evidence might be overlooked.
Evidence might be misinterpreted.
Reasoning might be incorrect.
Personal experiences might be given undue weight.
Reliance on wishful thinking might occur.
Misperceptions of patients’ preferences
Patient might misunderstand outcomes.
The measure of the effect might be misleading.
The outcomes might be presented or framed in different ways, leading to different conclusions.
The patient might not be consulted at all.
Health care providers might project their own preferences onto the patient.
Logical flaws in thinking and evaluating
Type of evidence available for determining intervention
“If there is no direct evidence from randomized, controlled trials, intervention should not be used.”
Degree of certainty regarding existence of an effect
“The P value is only .1, which is not statistically significant. The intervention should not be used.”
Seriousness of the outcome
“If the outcome without treatment is very bad, we have to assume that the treatment might work.”
Need to do something
“This intervention is all that is available.”
Novelty or technical appeal of an intervention or treatment
“This machine takes such a pretty picture it must have some use.”
Other factors
Pressure from patient, family, the press, the courts; the amount of paperwork; personal financial interests
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


