Epidemiology: Lesions Conferring Increased Risk of Breast Carcinoma
TERMINOLOGY
Abbreviations
Benign breast disease (BBD)
Definitions
BBD can be classified according to subsequent risk of developing invasive breast cancer
INTRODUCTION
Study of Benign Breast Lesions
Widespread use of mammographic screening has led to increased detection of BBD
Studies have identified 2 main classes of benign lesions
Risk indicators for development of invasive breast cancer
Predict generalized increased risk to both breasts
May be associated with other risk factors such as those related to hormone exposure
Precursor lesions for invasive carcinoma
Cells or lesions that may accumulate additional changes to eventually evolve into carcinoma
Lesions are nonobligate precursors; majority do not progress during patient’s lifetime
Some lesions are both risk indicators and precursors
For example, 60% of cancers developing after atypical hyperplasia (AH) are ipsilateral, and 40% are contralateral
Suggests that AH not only is an indicator of bilateral risk but can also act as a precursor in same breast
Morphologic Studies
BBD was originally classified according to histologic appearance
Association with carcinoma was postulated based on appearance and location
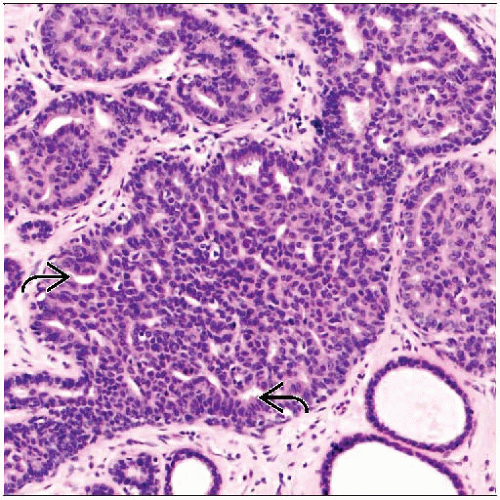
Some BBD resembles carcinoma
Hyperplasia resembles atypical ductal hyperplasia (ADH), which resembles DCIS
Atypical lobular hyperplasia (ALH) and LCIS are cytologically identical to invasive lobular carcinoma
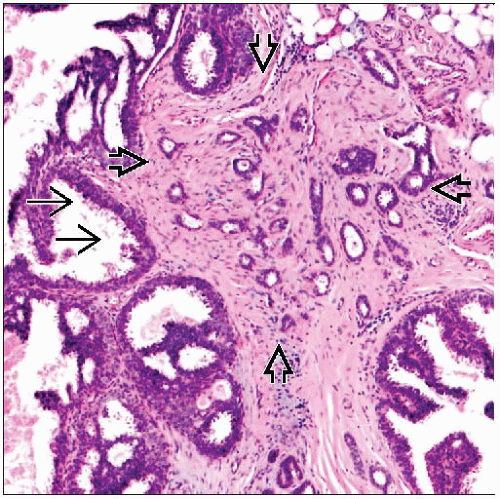
Radial sclerosing lesions are similar in appearance to tubular carcinoma
BBD is frequently seen adjacent to invasive carcinomas
ALH and LCIS near invasive lobular carcinoma
ADH and DCIS near invasive ductal carcinoma
Columnar cell change (± flat epithelial atypia), ALH/LCIS, and tubular carcinoma (“Rosen triad”)
Epidemiologic Studies
In 3 large studies, BBD in breast biopsies from women without cancer were categorized
Nashville Study
Nurses’ Health Study
Mayo Clinic Study
Women were followed over time to determine groups most likely to develop invasive carcinoma
Each study confirmed importance of classification of BBD to predict risk of subsequent carcinoma
Estimates of risk associated with each group of lesions were similar
Biologic Studies
Attempt to separate markers of risk from true precursors of invasive carcinoma
Loss of heterozygosity (LOH) for selected markers
Gene expression profiling
Comparative genomic hybridization
Most common recognized precursors are similar to ER-positive cancers
“Low-grade neoplasia” family includes columnar cell lesions, flat epithelial atypia, ADH, ALH, LCIS, and low-grade DCIS
Show strong diffuse positivity for ER
In normal breast, only ER-negative cells undergo division
Therefore, there must be a change in regulation of cell proliferation
Often associated with invasive tubular carcinoma, invasive cribriform carcinoma, grade 1 and 2 lobular carcinomas, and grade 1 invasive ductal carcinomas
All share deletions of 16q and gains of 1p
Radial sclerosing lesions are sometimes associated with tubular carcinomas or lobular carcinomas
Some are associated with loss of 16q
In some cases, it may be difficult to distinguish radial sclerosing lesion from low-grade invasive carcinoma
High-grade ER-positive cancers also show 16q deletions and are likely etiologically related to low-grade ER-positive cancers
Precursors for ER-negative cancer have not been established
Carcinomas are heterogeneous and include triple negative (basal-like), HER2 positive, apocrine, and other types
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree