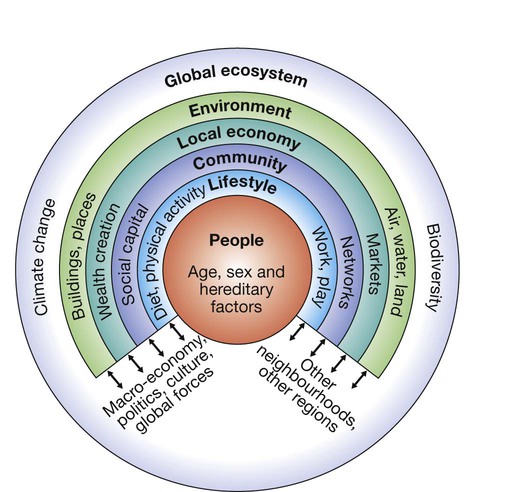
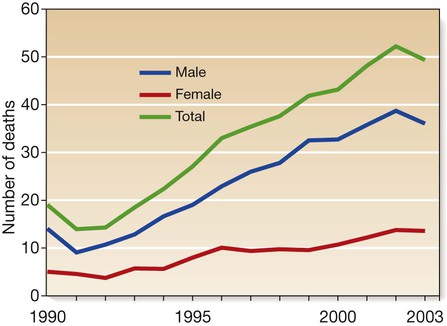
Health emerges from a highly complex interaction between factors intrinsic to the patient and his or her environment. Many factors within the environment influence health, including aspects of the physical environment, biological environment (bacteria, viruses), built environment and social environment, but these also encompass more distant influences such as the global ecosystem (Fig. 5.1). Environmental changes affect many physiological systems and do not respect boundaries between medical specialties. The specialty of ‘public health’ in the UK is concerned with the investigation and management of health in communities and populations, but the principles apply in all specialties. Exposure to infectious agents is a major environmental determinant of health and is described in detail in Chapter 6. This chapter describes the approach to other common environmental factors that influence health. When assessing a patient, a clinician subconsciously considers many levels at which problems may be occurring, including molecular, cellular, tissue, organ and body systems. When the environment’s influence on health is being considered, this ‘hierarchy of systems’ extends beyond the individual to include the family, community, population and ecology. Box 5.1 shows an example of the utility of this concept in describing determinants of coronary heart disease operating at each level of a hierarchy. The first task is to establish how common a problem is within the population. This is expressed in two ways (Box 5.2). • If the problem is a continuing condition (e.g. enlarged spleen due to malaria), then prevalence is the appropriate measurement and is calculated by dividing the number of people with the condition at a specified time by the number of people in the population at risk at that time. Prevalence tends to be higher if the problem is common (many new cases) and/or if it is of longer duration. • If the problem is an event that occurs at a clear point in time (e.g. fever due to malaria), then incidence is used. Incidence is a measure of the rate at which new cases occur (e.g. confirmed pyrexia with malaria parasites on a blood film) in the population at risk during a defined period of time. Associations between a risk factor and a disease do not prove that the risk factor causes the disease. In the northern hemisphere, both multiple sclerosis and blue eyes are more common but it is implausible that having blue eyes is the cause of multiple sclerosis. Cause and effect can only be proven by more detailed investigation. In the above example, further investigation of the river water will be needed, using the criteria for causation defined in Koch’s postulates (for infectious agents, p. 134) or the more generic Bradford Hill criteria. There are many examples of epidemiological associations defining causative factors in disease, e.g. the association between cigarette smoking and lung cancer (p. 699). However, as illustrated above, the complexity of the interactions between physical, social and economic determinants of health means that successful prevention is often difficult. Moreover, the life course perspective illustrates that it may be necessary to intervene early in life or even before birth, to prevent important disease in later life. Successful prevention is likely to require many interventions across the life course and at several levels in the hierarchy of systems. The examples below illustrate this principle. The term ‘homeostasis’ describes the capacity to maintain the internal milieu by adapting to increases or decreases in a given environmental factor. However, there are limits to the coping abilities of any system, at which ‘too much’ or ‘too little’ of a given environmental factor will result in ill health. Too many calories lead to obesity, while too few lead to malnutrition. Either involuntarily or deliberately, we expose ourselves to many poisons and hazards. Examples discussed elsewhere include industrial/occupational hazards, such as asbestos (p. 718) and other carcinogens (p. 266). ‘Social’ poisons, such as tobacco, alcohol and drugs of misuse, also need to be considered (p. 240). The World Health Organization (WHO) estimates that the harmful use of alcohol results in the death of 2.5 million people annually. Rates of alcohol-related harm vary by place and time but have risen dramatically in the UK, with Scotland showing the highest rates. (Fig. 5.2 demonstrates the climbing rates during the 1990s, since when rates have stabilised at very high levels.) Why did Scotland experience this dramatic increase in alcohol deaths? The most likely explanation is that the environment changed. The price of alcohol fell in real terms and availability increased (more supermarkets sold alcohol and the opening times of public houses were extended). Also, the culture changed in a way that fostered higher levels of consumption and more binge drinking. These changes have caused a trebling of male and a doubling of female deaths due to alcohol. Public, professional and governmental concern has now led to a minimum price being charged for a unit of alcohol, tightening of licensing regulations and curtailment of some promotional activity (e.g. two-for-one offers in bars). Many experts judge that even more aggressive public health measures will be needed to reverse the levels of harm in the community. The approach for individual patients suffering adverse effects of alcohol is described on pages 240 and 252. The adverse health and social consequences of poverty are well documented: high birth rates, high death rates and short life expectancy (Box 5.5). Typically, with industrialisation, the pattern changes: low birth rates, low death rates and longer life expectancy (Box 5.6). Instead of infections, chronic conditions such as heart disease dominate in an older population. Adverse health consequences of excessive affluence are also becoming apparent. Despite experiencing sustained economic growth for the last 50 years, people in many industrialised countries are not growing any happier and the litany of socioeconomic problems – crime, congestion, inequality – persists. Living in societies that give pride of place to economic growth means that there is constant pressure to contribute by performing ever harder at work and by consuming as much as – or more than – we can afford. As a result, people become stressed and may adopt unhealthy strategies to mitigate their discomfort; they overeat, overshop, or use sex or drugs (legal and illegal) as ‘pain-killers’. These behaviours often lead to the problems listed in Box 5.5. Radiation includes ionising (Box 5.7) and non-ionising radiations (ultraviolet (UV), visible light, laser, infrared and microwave). Whilst global industrialisation and the generation of fluorocarbons have raised concerns about loss of the ozone layer, leading to an increased exposure to UV rays, and disasters such as the Chernobyl and Fukushima nuclear power station explosions have demonstrated the harm of ionising radiation, it is important to remember that it can be harnessed for medical benefit. Ionising radiation is used in X-rays, computed tomography (CT), radionucleotide scans and radiotherapy, and non-ionising UV for therapy in skin diseases and laser therapy for diabetic retinopathy. These include charged subatomic alpha and beta particles, uncharged neutrons or high-energy electromagnetic radiations such as X-rays and gamma rays. When they interact with atoms, energy is released and the resulting ionisation can lead to molecular damage. The clinical effects of different forms of radiation depend upon their range in air and tissue penetration (see Box 5.7). Body heat is generated by basal metabolic activity and muscle movement, and lost by conduction (which is more effective in water than in air), convection, evaporation and radiation (most important at lower temperatures when other mechanisms conserve heat) (Box 5.8). Body temperature is controlled in the hypothalamus, which is directly sensitive to changes in core temperature and indirectly responds to temperature-sensitive neurons in the skin. The normal ‘set-point’ of core temperature is tightly regulated within 37 ± 0.5°C, which is necessary to preserve the normal function of many enzymes and other metabolic processes. The temperature set-point is increased in response to infection (p. 296). Hypothermia exists when the body’s normal thermal regulatory mechanisms are unable to maintain heat in a cold environment and core temperature falls below 35°C (Fig. 5.3). Whilst infants are susceptible to hypothermia because of their poor thermoregulation and high body surface area to weight ratio, it is the elderly who are at highest risk (Box 5.9). Hypothyroidism is often a contributory factor in old age, while alcohol and other drugs (e.g. phenothiazines) commonly impede the thermoregulatory response in younger people. More rarely, hypothermia is secondary to glucocorticoid insufficiency, stroke, hepatic failure or hypoglycaemia. Diagnosis is dependent on recognition of the environmental circumstances and measurement of core (rectal) body temperature. Clinical features depend on the degree of hypothermia (see Fig. 5.3). In a cold patient, it is very difficult to diagnose death reliably by clinical means. It has been suggested that, in extreme environmental conditions, irreversible hypothermia is probably present if there is asystole (no carotid pulse for 1 minute), the chest and abdomen are rigid, the core temperature is below 13°C and serum potassium is > 12 mmol/L. However, in general, resuscitative measures should continue until the core temperature is normal and only then should a diagnosis of brain death be considered (p. 1161). Blood gases, a full blood count, electrolytes, chest X-ray and electrocardiogram (ECG) are all essential investigations. Haemoconcentration and metabolic acidosis are common, and the ECG may show characteristic J waves, which occur at the junction of the QRS complex and the ST segment (Fig. 5.4). Cardiac dysrhythmias, including ventricular fibrillation, may occur. Although the arterial oxygen tension may be normal when measured at room temperature, the arterial PO2 in the blood falls by 7% for each 1°C fall in core temperature. Serum aspartate aminotransferase and creatine kinase may be elevated secondary to muscle damage and the serum amylase is often high due to subclinical pancreatitis. If the cause of hypothermia is not obvious, additional investigations for thyroid and pituitary dysfunction (p. 737), hypoglycaemia (p. 807) and the possibility of drug intoxication (p. 209) should be performed. Outdoors, continued heat loss is prevented by sheltering the patient from the cold, replacing wet clothing, covering the head and insulating him or her from the ground. Once in hospital, even in the presence of profound hypothermia, if there is an effective cardiac output then forced-air rewarming, heat packs placed in axilla, groin and around the abdomen, inhaled warmed air and correction of fluid and electrolyte disturbances are usually sufficient. Rewarming rates of 1–2°C per hour are effective in leading to a gradual and safe return to physiological normality. Underlying conditions should be treated promptly (e.g. hypothyroidism with triiodothyronine 10 µg IV 3 times daily; p. 743). In the case of severe hypothermia with cardiopulmonary arrest (non-perfusing rhythm), the aim is to restore perfusion, and rapid rewarming at a rate greater than 2°C per hour is required. This is best achieved by cardiopulmonary bypass or extracorporeal membrane oxygenation. If these are unavailable, then veno–veno haemofiltration, and pleural, peritoneal, thoracic or bladder lavage with warmed fluids are alternatives. Monitoring of cardiac rhythm and arterial blood gases, including H+ (pH) is essential. Significant acidosis may require correction (p. 445). This represents the direct freezing of body tissues and usually affects the extremities: in particular, the fingers, toes, ears and face. Risk factors include smoking, peripheral vascular disease, dehydration and alcohol consumption. The tissues may become anaesthetised before freezing and, as a result, the injury often goes unrecognised at first. Frostbitten tissue is initially pale and doughy to the touch and insensitive to pain (Fig. 5.5). Once frozen, the tissue is hard. Acclimatisation mechanisms to environmental heat include stimulation of the sweat mechanism with increased sweat volume, reduced sweat sodium content and secondary hyperaldosteronism to maintain body sodium balance. The risk of heat-related illness falls as acclimatisation occurs. Heat illness can be prevented to a large extent by adequate replacement of salt and water, although excessive water intake alone should be avoided because of the risk of dilutional hyponatraemia (p. 437). A spectrum of illnesses occurs in the heat (see Fig. 5.3). The cause is usually obvious but the differential diagnosis should be considered (Box 5.10). Heat exhaustion occurs with prolonged exertion in hot and humid weather, profuse sweating and inadequate salt and water replacement. There is an elevation in core (rectal) temperature to between 37°C and 40°C, leading to the clinical features shown in Figure 5.3. Blood analyses may show evidence of dehydration with mild elevation of the blood urea, sodium and haematocrit. Treatment involves removal of the patient from the heat, and active evaporative cooling using tepid sprays and fanning (strip–spray–fan). Fluid losses are replaced with either oral rehydration mixtures or intravenous isotonic saline. Up to 5 L positive fluid balance may be required in the first 24 hours. Untreated, heat exhaustion may progress to heat stroke. The physiological effects of high altitude are significant. On Everest, the barometric pressure of the atmosphere falls from sea level by approximately 50% at base camp (5400 m) and approximately 70% at the summit (8848 m). The proportions of oxygen, nitrogen and carbon dioxide in air do not change with the fall in pressure but their partial pressure falls in proportion to barometric pressure (Fig. 5.6). Oxygen tension within the pulmonary alveoli is further reduced at altitude because the partial pressure of water vapour is related to body temperature and not barometric pressure, and so is proportionately greater at altitude, accounting for only 6% of barometric pressure at sea level, but 19% at 8848 m. Reduction in oxygen tension results in a fall in arterial oxygen saturation (see Fig. 5.6). This varies widely between individuals, depending on the shape of the sigmoid oxygen–haemoglobin dissociation curve (see Fig. 8.3, p. 183) and the ventilatory response. Acclimatisation to hypoxaemia at high altitude involves a shift in this dissociation curve (dependent on 2,3-diphosphoglycerate (DPG)), erythropoiesis, haemoconcentration, and hyperventilation resulting from hypoxic drive (which is then sustained despite hypocapnia by restoration of cerebrospinal fluid pH to normal in prolonged hypoxia). This process takes several days, so travellers need to plan accordingly. Commercial aircraft usually cruise at 10 000–12 000 m, with the cabin pressurised to an equivalent of around 2400 m. At this altitude, the partial pressure of oxygen is 16 kPa (120 mmHg), leading to a PaO2 in healthy people of 7.0–8.5 kPa (53–64 mmHg). Oxygen saturation is also reduced, but to a lesser degree (see Fig. 5.6). Although well tolerated by healthy people, this degree of hypoxia may be dangerous in patients with respiratory disease. On long-haul flights, patients with diabetes mellitus may need to adjust their insulin or oral hypoglycaemic dosing according to the timing of in-flight and subsequent meals (p. 825). Advice is available from Diabetes UK and other websites. Patients should be able to provide documentary evidence of the need to carry needles and insulin. Air travellers have an increased risk of venous thrombosis (p. 1008), due to a combination of factors, including loss of venous emptying because of prolonged immobilisation (lack of muscular activity) and reduced barometric pressure on the tissues, together with haemoconcentration as a result of oedema and perhaps a degree of hypoxia-induced diuresis. Drowning is defined as death due to asphyxiation following immersion in a fluid, whilst near-drowning is defined as survival for longer than 24 hours after suffocation by immersion. Drowning remains a common cause of accidental death throughout the world and is particularly common in young children (Box 5.11). In about 10% of cases, no water enters the lungs and death follows intense laryngospasm (‘dry’ drowning). Prolonged immersion in cold water, with or without water inhalation, results in a rapid fall in core body temperature and hypothermia (p. 104). Those rescued alive (near-drowning) are often unconscious and not breathing. Hypoxaemia and metabolic acidosis are inevitable features. Acute lung injury usually resolves rapidly over 48–72 hours, unless infection occurs (Fig. 5.7). Complications include dehydration, hypotension, haemoptysis, rhabdomyolysis, renal failure and cardiac dysrhythmias. A small number of patients, mainly the more severely ill, progress to develop the acute respiratory distress syndrome (ARDS; p. 192). Initial management requires cardiopulmonary resuscitation with administration of oxygen and maintenance of the circulation (p. 558). It is important to clear the airway of foreign bodies and protect the cervical spine. Continuous positive airways pressure (CPAP; p. 193) should be considered for spontaneously breathing patients with oxygen saturations below 94%. Observation is required for a minimum of 24 hours. Prophylactic antibiotics are only required if exposure was to obviously contaminated water. Ambient pressure under water increases by 101 kPa (1 atmosphere) for every 10 metres of seawater (msw) depth. As divers descend, the partial pressures of the gases they are breathing increase (Box 5.12), and the blood and tissue concentrations of dissolved gases rise accordingly. Nitrogen is a weak anaesthetic agent, and if the inspiratory pressure of nitrogen is allowed to increase above −320 kPa (i.e. a depth of approximately 30 msw), it produces ‘narcosis’, resulting in impairment of cognitive function and manual dexterity, not unlike alcohol intoxication. For this reason, compressed air can only be used for shallow diving. Oxygen is also toxic at inspired pressures above approximately 40 kPa (inducing apprehension, muscle twitching, euphoria, sweating, tinnitus, nausea and vertigo), so 100% oxygen cannot be used as an alternative. For dives deeper than approximately 30 msw, mixtures of oxygen with nitrogen and/or helium are used. Exposure of individuals to increased partial pressures of nitrogen results in additional nitrogen being dissolved in body tissues; the amount dissolved depends on the depth/pressure and on the duration of the dive. On ascent, the tissues become supersaturated with nitrogen, and this places the diver at risk of producing a critical quantity of gas (bubbles) in tissues if the ascent is too fast. The gas so formed may cause symptoms locally, by bubbles passing through the pulmonary vascular bed (Box 5.13) or by embolisation elsewhere. Arterial embolisation may occur if the gas load in the venous system exceeds the lungs’ abilities to excrete nitrogen, or when bubbles pass through a patent foramen ovale (present asymptomatically in 25–30% of adults; p. 528). Although DCS and AGE can be indistinguishable, their early treatment is the same.
Environmental and nutritional factors in disease
Principles and investigation of environmental factors in disease
Environmental effects on health
The hierarchy of systems – from molecules to ecologies
Investigations in environmental health
Incidence and prevalence
Establishing cause and effect
Preventive medicine
Environmental diseases
Alcohol
Poverty and affluence
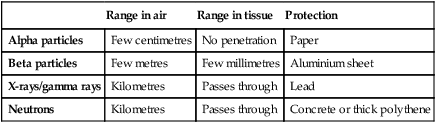
Radiation exposure
Types of ionising radiation
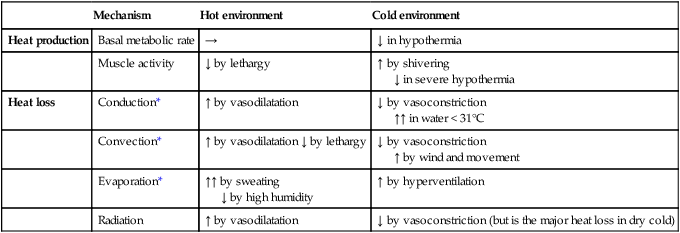
Extremes of temperature
Thermoregulation
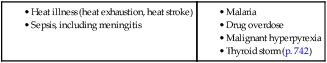
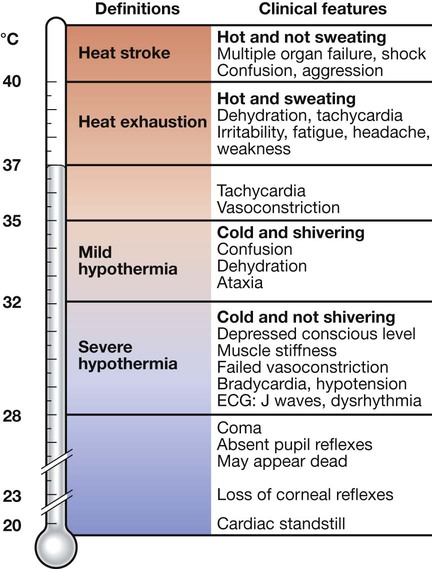
Hypothermia
The hypothalamus normally maintains core temperature at 37°C, but this set-point is altered – for example, in fever (pyrexia, p. 296) – and may be lost in hypothalamic disease (p. 785). In these circumstances, the clinical picture at a given core temperature may be different.
Clinical features
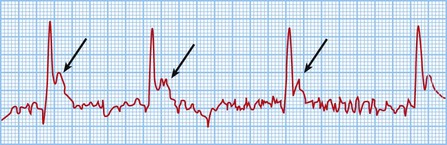
Investigations
Management
Mild hypothermia
Severe hypothermia
Cold injury
Freezing cold injury (frostbite)
Heat-related illness
Heat exhaustion
High altitude
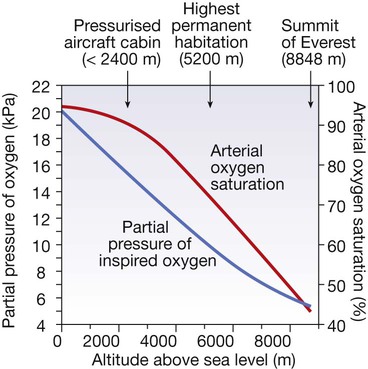
The blue curve shows changes in oxygen availability at altitude and the red curve shows the typical resultant changes in arterial oxygen saturation in a healthy person. Oxygen saturation varies between individuals according to the shape of the oxygen–haemoglobin dissociation curve and the ventilatory response to hypoxaemia. (To convert kPa to mmHg, multiply by 7.5.)
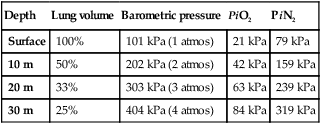
Physiological effects of high altitude
Air travel
Advice for other patients
Deep venous thrombosis
Under water
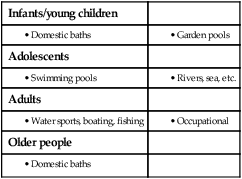
Drowning and near-drowning
Clinical features
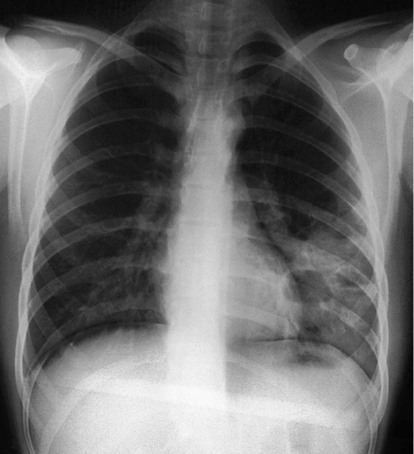
Chest X-ray of a 39-year-old farmer, 2 weeks after immersion in a polluted freshwater ditch for 5 minutes before rescue. Airspace consolidation and cavities in the left lower lobe reflect secondary staphylococcal pneumonia and abscess formation.
Management
Diving-related illness
Clinical features
Decompression illness