Chapter 16 Drugs to Treat Asthma and Chronic Obstructive Pulmonary Disease
| Abbreviations | |
|---|---|
| ACh | Acetylcholine |
| BLT | Leukotriene B receptor |
| cAMP | Cyclic adenosine monophosphate |
| CNS | Central nervous system |
| COPD | Chronic obstructive pulmonary disease |
| CysLT | Cys-leukotriene |
| Epi | Epinephrine |
| FEV1 | Forced expiratory volume in 1 second (liters) |
| GCs | Glucocorticoids |
| GI | Gastrointestinal |
| IgE | Immunoglobulin type E |
| IL | Interleukin |
| IV | Intravenous |
| LOX | Lipoxygenase |
| LTs | Leukotrienes |
| LTMs | Leukotriene modulators |
| MDI | Metered-dose inhaler |
| PDE | Phosphodiesterase |
| PEF | Peak expiratory flow |
| TNF | Tumor necrosis factor |
Therapeutic Overview
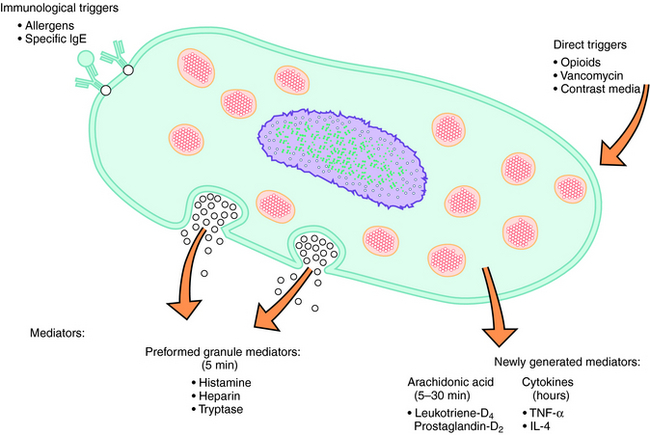
Normal bronchial smooth muscle tone is controlled by vagal innervation (see Chapter 9). Cholinergic activity or sensitivity is often increased in asthmatics, and increased cholinergic tone is the primary reversible component of COPD. However, most patients with asthma also have increased adrenergic activity (see Chapter 11), which manifests as increased wheezing if patients are treated with β adrenergic receptor blocking drugs (e.g., propranolol), which are contraindicated in asthma. A variety of agents can contribute to the inflammation of asthma; however, immediate hypersensitivity to common allergens is the most common cause. It is estimated that 80% of children and 50% of adults with asthma are allergic. The common allergens include seasonal outdoor allergens (e.g., ragweed pollen, grass pollen, and mold) or the year-round indoor allergens (dust mites, cockroaches, and domestic animal dander). Allergens cause release of the preformed granule mediator histamine, which can trigger bronchospasm. However, antihistamines (H1 receptor antagonists) are relatively ineffective in the treatment of asthma, demonstrating that other factors are key mediators of the asthma attack. In patients with asthma, in addition to the release of prestored mediators such as histamine from mast cells, other inflammatory mediators are synthesized and released including arachidonic acid, its metabolites, and several cytokines (Fig. 16-1). Leukotrienes (LTs), primarily LTD4, are implicated as major mediators of bronchoconstriction. Agents that inhibit the synthesis or action of the LTs, known as leukotriene modulators (LTMs), are useful for the treatment of asthma.
Asthma is treated using three main approaches. The first is avoidance of the causative factors, when possible, particularly for patients sensitive to indoor allergens. The second is the use of antiinflammatory drugs, including cromolyn and related agents, glucocorticoids (GCs) (see Chapter 39), and LTMs. If used regularly, these drugs can reduce the signs and symptoms of bronchial hyperactivity, characteristic of asthma. Third, drugs that can reverse or inhibit the development of bronchoconstriction are important; these compounds include methylxanthines, epinephrine (Epi) and selective adrenergic β2 receptor agonists (see Chapter 11), and the muscarinic receptor antagonists (see Chapter 10).
| Therapeutic Overview |
|---|
| Antiinflammatory Agents |
| Cromolyn and related agents control mediator release from mast and other cells and for their generalized membrane-stabilizing effects |
| Glucocorticoids, inhaled or systemic, for controlling transcription of mediator genes, and for controlling edema, mucus production, and eosinophil infiltration |
| Leukotriene modulators to decrease inflammatory mediator synthesis or antagonize inflammatory mediator receptors |
| Bronchodilators |
| Methylxanthines for reducing the frequency of recurrent bronchospasm |
| Adrenergic β2 receptor agonists for relaxing bronchial smooth muscle and decreasing microvascular permeability |
| Muscarinic receptor antagonists for inhibiting the bronchoconstrictor effects of endogenous acetylcholine |
Mechanisms of Action
Treatment of asthma and COPD involves the use of drugs with mechanisms that affect different aspects of these diseases. Table 16-1 summarizes these drugs and their mechanisms of action.
TABLE 16–1 Mechanisms of Action of Drugs to Treat Asthma and COPD
| Beneficial Effect | Drug Class | Cellular Mechanisms |
|---|---|---|
| Decreased inflammation | Chromones | Prevent the release of inflammatory mediators |
| Alter chloride ion channel function | ||
| Glucocorticoids (GCs) | Regulate gene expression | |
| Leukotriene modulators (LTMs) | Decrease leukotriene (LT) synthesis or prevent LT receptor activation | |
| Antihistamines | Prevent activation of histamine receptors | |
| Bronchodilation | Methylxanthines | Increase cAMP |
| Adenosine receptor antagonist | ||
| Adrenergic β2 receptor agonists | Increase cAMP | |
| Muscarinic antagonists | Block activation of muscarinic receptors by endogenous acetylcholine |
The GCs have multiple actions that decrease inflammation in asthma, which is key to improving asthmatic symptoms and preventing exacerbations. In controlling the inflammation of asthma, the primary effect of the GCs is to alter gene expression. The GCs, through activation of GC receptors (see Chapter 39), suppress the expression of genes for many inflammatory proteins. Inflammation is mediated by the increased expression of multiple inflammatory proteins including cytokines, chemokines, adhesion molecules, and inflammatory enzymes and receptors. The expression of most of these inflammatory proteins is regulated by increased gene transcription, which is controlled by proinflammatory transcription factors. The GCs are believed to switch off only inflammatory genes and do not suppress all activated genes because of the selective binding to coactivators that are activated by proinflammatory transcription factors.
GCs decrease bone marrow production of eosinophils and enhance their removal from the circulation by mediating their adherence to capillary walls (margination). GCs also reduce the local accumulation of eosinophils by inhibiting the release of eosinophil chemotactic factors such as LTB4 and cytokine tumor necrosis factor-α (TNF-α). The effect of the GCs on neutrophils is opposite to that on eosinophils. By inhibiting margination and stimulating bone marrow production, GCs lead to an increase in circulating neutrophils.
The LTs are potent inflammatory mediators generated from the metabolism of arachidonic acid through the 5-lipoxygenase (5-LOX) pathway (Fig. 16-2). These compounds, along with prostaglandins and related compounds, belong to a group of substances termed the eicosanoids (see Chapter 15). The LTs are synthesized in many inflammatory cells in the respiratory system including eosinophils, mast cells, macrophages, and basophils and are responsible for mediating numerous asthmatic symptoms via stimulation of specific LT receptors. LTB4 is a potent neutrophil chemotactic agent whose actions result from stimulation of members of the LTB receptor (BLT) family. Similarly, LTC4 and LTD4 cause bronchoconstriction, mucus hypersecretion, and mucosal edema and increase bronchial reactivity through activation of the Cys-leukotriene (CysLT, formerly known as the LTD4) receptor family. The effects of the LTs can be modulated either by inhibiting LT biosynthesis or by blocking activation of CysLT receptors. Zileuton* is an inhibitor of 5-LOX, thereby decreasing LT synthesis, whereas zafirlukast and montelukast are antagonists at Cys-LT1 receptors, thereby blocking receptor activation. These drugs are less effective antiinflammatory agents than the corticosteroids, but are preferable to long-term GC therapy because they have fewer adverse effects (see Chapter 39). They are used prophylactically in combination products.
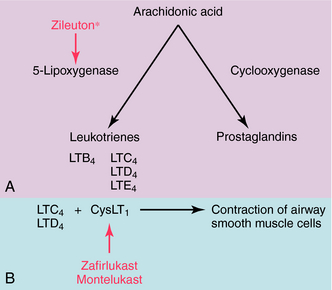
FIGURE 16–2 Newly generated lipid mast cell mediators depicting the sites of action of the LTMs. Zileuton* inhibits 5-lipoxygenase, thereby inhibiting the synthesis of the leukotrienes, whereas zafirlukast and montelukast are antagonists at the CysLT1 receptor. The inhibitory actions of the LTMs are shown in red.