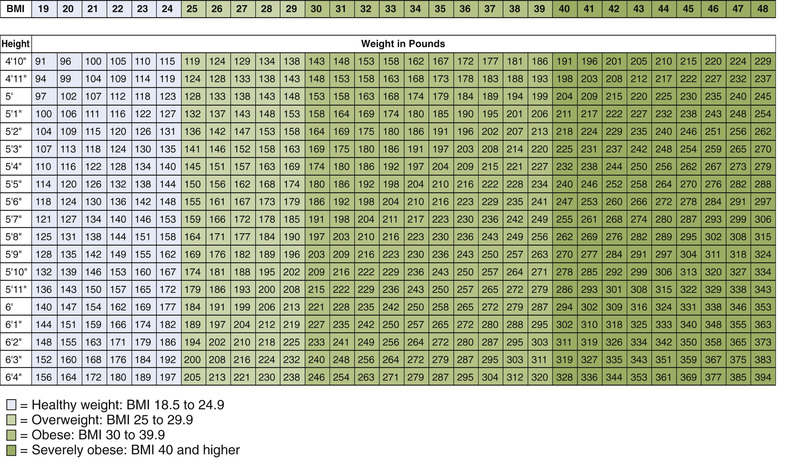
According to the federal guidelines, a BMI of 30 or higher indicates obesity. Individuals with a BMI of 25 to 29.9 are considered overweight, but not obese. There is evidence that the risk for cardiovascular disease and other disorders rises when the BMI exceeds 25. These associations between BMI and health risk do not apply to older adults, growing children, or women who are pregnant or lactating. Nor do they apply to competitive athletes or bodybuilders, who are heavy because of muscle mass rather than excess fat.
Waist Circumference
Waist circumference (WC) is an indicator of abdominal fat content, an independent risk factor for obesity-related diseases. Accumulation of fat in the upper body, and especially within the abdominal cavity, poses a greater risk to health than does accumulation of fat in the lower body (hips and thighs). People with too much abdominal fat are at increased risk for insulin resistance, diabetes, hypertension, coronary atherosclerosis, ischemic stroke, and dementia. Fat distribution can be estimated simply by looking in the mirror: an apple shape indicates too much abdominal fat, whereas a pear shape indicates fat on the hips and thighs. Measurement of WC provides a quantitative estimate of abdominal fat. A WC exceeding 40 inches (102 cm) in men or 35 inches (88 cm) in women signifies an increased health risk—but only for people with a BMI between 25 and 34.9.
Risk Status
Overall weight-related health risk is determined by BMI, WC, and the presence of weight-related diseases and cardiovascular risk factors. Certain weight-related diseases—established coronary heart disease, other atherosclerotic diseases, type 2 diabetes, and sleep apnea—confer a risk for complications and mortality. Other weight-related diseases—gynecologic abnormalities, osteoarthritis, gallstones, and stress incontinence—confer less risk. Cardiovascular risk factors—smoking, hypertension, high levels of low-density lipoprotein (LDL) cholesterol, low levels of high-density lipoprotein (HDL) cholesterol, high fasting glucose, family history of premature coronary heart disease, physical inactivity, and advancing age—confer a high risk when three or more of these factors are present.
Health risk rises as BMI gets larger. In addition, the risk is increased by the presence of an excessive WC. The risk is further increased by weight-related diseases and cardiovascular risk factors. In the absence of an excessive WC and other risk factors, health risk is minimal with a BMI below 25 and relatively low with a BMI below 30. Conversely, a BMI of 30 or more indicates significant risk. In the presence of an excessive WC, health risk is high for all individuals with a BMI above 25.
Overview of Obesity Treatment
The strategy for losing weight is simple: take in fewer calories per day than are burned. Of course, implementation is much more challenging. The key components of a weight-loss program are diet and exercise. Drugs and other measures are employed only as adjuncts.
Benefits of Treatment
In overweight and obese people, weight reduction may confer these benefits:
• Reduction of high blood pressure in patients with hypertension
• Improvement of blood lipid status (elevation of HDL cholesterol and reduction of LDL cholesterol, total cholesterol, and triglycerides)
• Reduction in development of type 2 diabetes mellitus (DM) and, in patients with type 2 DM, reduction of elevated blood glucose
Treatment Goal
The goal of treatment is to promote and maintain weight loss. The initial objective is to reduce weight by 10% over 6 months. For patients with a BMI of 27 to 35, this can usually be achieved by reducing energy intake by 300 to 500 kcal/day, which should allow a loss of 0.5 to 1 pound a week—or 13 to 26 pounds in 6 months. People with a BMI above 35 require greater caloric restriction (500–1000 kcal/day) to lose 10% of their weight in 6 months. After 6 months, the goal for all patients is to prevent lost weight from returning. This may be accomplished by a combination of diet, physical activity, and behavioral therapy. If appropriate, additional weight reduction can be attempted.
Although these goals are laudable and a return to a normal BMI is desirable, this is rarely achieved in obese individuals, even with drug therapy. A more realistic goal is to target a percentage of body weight at which risk is decreased and comorbidities prevented. A weight loss of 10% to 15% is typical for those who diligently adhere to medication and lifestyle regimen, whereas a loss greater than 15% is exceptional.
Treatment Modalities
Weight loss can be accomplished with five treatment modalities: caloric restriction, physical activity, behavioral therapy, drug therapy, and surgery. For any individual, the treatment mode is determined by the degree of obesity and personal preference.
Caloric Restriction
A reduced-calorie diet is central to any weight-loss program. As noted, the only way to lose weight is to take in fewer calories than are burned. Depending on the individual, the caloric deficit should range from 300 to 1000 kcal/day. Because fats contain more calories than either carbohydrates or proteins (on an ounce-for-ounce basis), reducing dietary fat is the easiest way to reduce calorie intake.
To succeed at losing weight, it helps to know just how many calories are taken in each day and how many you burn. The following websites, which are free, have databases on foods and physical activities, along with tools to calculate and log calories taken in and calories burned:
Exercise
Physical activity should be a component of all weight-loss and weight-maintenance programs. Exercise makes a modest contribution to weight loss by increasing energy expenditure. In addition, exercise can help reduce abdominal fat, increase cardiorespiratory fitness, and maintain weight once loss has occurred. According to the American College of Sports Medicine, people trying to lose weight should exercise at least 150 minutes per week (and preferably more), and those trying to maintain weight loss should exercise 200 to 300 minutes per week.
Behavior Modification
Behavioral therapy is directed at modifying eating and exercise habits. As such, behavioral therapy can strengthen a program of diet and exercise. Techniques of behavioral therapy include self-monitoring of eating and exercise habits, stress management (because stress can trigger eating), and stimulus control (limiting exposure to stimuli that promote eating). There is no evidence that any one of these techniques is superior to others.
Drug Therapy
In theory, drugs can promote weight loss in three ways: they can suppress appetite, reduce absorption of nutrients, or increase metabolic rate. Drugs can be used as an adjunct to diet and exercise—but only for people at increased health risk, and only after a 6-month program of diet and exercise has failed. Drugs should never be used alone; rather, they should be part of a comprehensive weight-reduction program—one that includes exercise, behavior modification, and a reduced-calorie diet.
Drugs should be reserved for patients whose BMI is 30 or greater or 27 or greater in the presence of additional risk factors. Drugs are not appropriate for patients whose BMI is relatively low. Drugs are also not appropriate for women who are pregnant. The American College of Obstetricians and Gynecologists recommends weight gain, not loss, for obese women who are pregnant, although the total amount of gain is less than that of women who are within normal limits for weight.
Benefits of drugs are usually modest. Weight loss attributable to drugs generally ranges between 4.4 and 22 pounds, although some people lose significantly more. As a rule, most weight loss occurs during the first 6 months of treatment.
Duration of therapy varies depending on the drug selected. Today, long-term treatment is recommended more often than in the past because we now know that, when drugs are discontinued, most patients regain lost weight. Accordingly, when treatment has been effective and well tolerated, it may need to continue indefinitely. Unfortunately, not all drugs are approved for long-term use.
Not everyone responds to drugs, so regular assessment is required. Patients should lose at least 4 pounds during the first 4 weeks of drug treatment. If this initial response is absent, further drug use should be questioned. For patients who do respond, ongoing assessment must show that (1) the drug is effective at maintaining weight loss and (2) serious adverse effects are absent. Otherwise, drug therapy should cease.
Bariatric Surgery
Surgical procedures can produce significant weight loss by reducing food intake. However, they are indicated only for patients with a BMI of 40 or more (in the absence of severe comorbidity). The two most widely used procedures are gastric bypass surgery (Roux-en-Y procedure) and laparoscopic implantation of an adjustable gastric band, which reduces the effective volume of the upper part of the stomach. Surgery is effective: in 6 months to a year, patients can lose between 110 and 220 pounds. Unfortunately, the surgery can carry significant risk: in one study, mortality rates at 30 days, 90 days, and 1 year after gastric surgery were 2%, 2.8%, and 4.6%, respectively.
Weight-Loss Drugs
As previously mentioned, weight loss drugs vary in their ability to promote weight loss. The combination drug topiramate/phentermine is associated with the greatest amount of weight loss (greater than 5% of body weight). This is followed by phentermine as monotherapy and another combination drug naltrexone/bupropion, which generally achieve a weight loss of greater than 3% to 5%. Orlistat provides the least weight loss (2%–3%). The individual classes of weight loss drugs are discussed next. Dosages and administration guidelines are summarized in Table 66.1.
TABLE 66.1
Dosages and Administration
| Drug Class and Drug | Preparation | Dosage | Administration |
| LIPASE INHIBITOR | |||
| Orlistat (Alli, Xenical) | Alli: 60-mg tablet (over the counter) Xenical: 120-mg tablet | Alli: 60-mg 3 times daily with meals Xenical: 120-mg 3 times daily with meals | Take with, or 1 hour after, meals that contain fat. Omit dose if a meal is missed or if a meal does not contain fat. Fat-soluble vitamins (A, D, E, K) should be taken at least 2 hours before or after orlistat. |
| SEROTONIN 5-HT2C RECEPTOR AGONIST | |||
| Lorcaserin (Belviq) | 10-mg tablet | 10 mg twice daily | Oral administration. May be taken with or without food. |
| SYMPATHOMIMETIC AMINES | |||
| Diethylpropion (generic) | 25-mg immediate-release tablet 75-mg extended-release tablet | Immediate release: 25 mg 3 times daily Extended release: 75 mg daily | Oral administration. Administer immediate release tablets 1 hour before meals. Administer extended-release tablets at midmorning. Avoid evening or nighttime administration to prevent insomnia. |
| Phentermine (Adipex-P, Suprenza) | Adipex-P: 37.5-mg tablet; 37.5-mg capsule Suprenza: 15-, 30-, or 37.5-mg disintegrating tablet | Adipex-P: Usual dosage is 37.5 mg daily. Alternate dosing schedules are Suprenza: Individualize dosage to the lowest effective dose. | Oral administration. May be taken with or without food. Administer before breakfast or 1–2 hours after breakfast. Avoid evening or night time administration to prevent insomnia. |
| GLUCAGON-LIKE PEPTIDE-1 AGONIST | |||
| Liraglutide (Saxenda) | Prefilled multidose pens hold 3 mL of a 6-mg/mL solution. Pen contains a dose selector that allows delivery of specific doses at 0.6-, 1.2-, 1.8-, 2.4-, and 3-mg doses | Week 1: 0.6 mg daily Week 2: 1.2 mg daily Week 3: 1.8 mg daily Week 4: 2.4 mg daily Week 5 and thereafter: 3 mg daily | Injected subcutaneously in upper arm, abdomen, or thigh. Does not need to be coordinated with intake. |
| COMBINATION PRODUCTS | |||
| Phentermine/topiramate (Qsymia) | 24-hour extended-release tablet in four strengths 3.75/23 (Phentermine 3.75 mg/topiramate 23 mg) 7.5/46 (Phentermine 7.5 mg/topiramate 46 mg) 11.25/69 (Phentermine 11.25 mg/topiramate 69 mg) 15/92 (Phentermine 15 mg/topiramate 92 mg) | Weeks 1 and 2: One 3.75/23 tablet daily, followed by one 75/46 tablet daily for 12 weeks Evaluate weight loss. If 3% of baseline body weight has not occurred, discontinue or increase to one 11.25/69 tablet once daily for 2 weeks followed by one 15/92 tablet for 12 weeks. Evaluate weight loss. If 5% of baseline weight has not been lost, taper off therapy. | Administer in the morning. May be taken with or without food. Avoid evening or nighttime administration to prevent insomnia. |
| Naltrexone/bupropion (Contrave) | 12-hour extended-release tablet containing naltrexone 8 mg/bupropion 90 mg | Week 1: one tablet in the morning Week 2: one tablet in the morning; one tablet in the evening Week 3: two tablets in the morning; one tablet in the evening Week 4 and thereafter: two tablets in the morning; two tablets in the evening | Substantial increases in bupropion and naltrexone occur when taken with high-fat meals, so this should be avoided. If a dose is skipped, wait until the next scheduled dose to resume schedule. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 tablet (18.75 mg) daily or
tablet (18.75 mg) daily or  tablet twice daily. Lowest effective dose is recommended.
tablet twice daily. Lowest effective dose is recommended.