Pathophysiology and Treatment Overview
Primary Open-Angle Glaucoma
Characteristics
Primary open-angle glaucoma (POAG) is the most common form of glaucoma in the United States. About 90% of people with glaucoma have this type. POAG is a leading cause of blindness in the United States.
POAG is characterized by progressive optic nerve damage with eventual impairment of vision. Visual loss develops first in the peripheral visual field. As the disease advances, loss occurs in the central visual field. The pathologic process that leads to optic nerve damage is not understood. IOP is often elevated, but it may also be normal. POAG is a painless, insidious disease in which injury develops over years. Symptoms are absent until extensive optic nerve damage has been produced.
Risk Factors
The major risk factors for POAG are the following:
Of these, elevated IOP is most important. Please note, however, that glaucomatous optic nerve damage can develop even when IOP is normal (i.e., below 20 mm Hg). Furthermore, some individuals can have very high IOP (e.g., 30 mm Hg) with no associated injury to the optic nerve. These individuals are said to have ocular hypertension—not glaucoma.
Screening
Because POAG has no symptoms (until significant and irreversible optic nerve injury has occurred), regular testing for early POAG is important among individuals at high risk. With early detection and treatment, blindness can usually be prevented.
Management
Treatment of POAG is directed at reducing elevated IOP, the only risk factor we can modify. Although POAG has no cure, reduction of IOP can slow or even stop disease progression. Management is usually initiated by specialists; however, primary care providers often play a role in ongoing monitoring and follow-up of patients taking these medications.
The principal method for reducing IOP is chronic therapy with drugs. Drugs lower IOP by either (1) facilitating aqueous humor outflow or (2) reducing aqueous humor production. As indicated in Table 84.1, the first-line drugs for glaucoma belong to three classes: beta-adrenergic blocking agents (beta blockers), alpha2-adrenergic agonists, and prostaglandin analogs. Other options—cholinergic drugs and carbonic anhydrase inhibitors—are considered second-line choices. All of the antiglaucoma drugs are available for topical administration, which is the preferred route. For more than 25 years, the beta blockers (e.g., timolol) have been considered drugs of first choice. However, the alpha2 agonists (e.g., brimonidine) and prostaglandin analogs (e.g., latanoprost) are just as effective as the beta blockers and have a more desirable side-effect profile. Accordingly, these drugs have joined the beta blockers as first-choice agents. Because drugs in different classes lower IOP by different mechanisms, combined therapy can be more effective than monotherapy. Because all of these drugs are applied topically, systemic effects are relatively uncommon. Nonetheless, serious systemic reactions can occur if sufficient absorption takes place.
TABLE 84.1
Topical Drugs for Open-Angle Glaucoma
| Class | Drugs | Mechanism | Adverse Effects |
| FIRST-LINE AGENTS | |||
| Beta blockers | Decreased aqueous humor formation | ||
| Nonselective | Timolol Carteolol Levobunolol Metipranolol | Heart block, bradycardia, bronchospasm | |
| Beta1 selective | Betaxolol | Heart block, bradycardia, hypotension | |
| Prostaglandin analogs | Latanoprost Travoprost Bimatoprost | Increased aqueous humor outflow | Heightened brown pigmentation of the iris and eyelid |
| Alpha2-adrenergic agonists | Apraclonidine* Brimonidine | Decreased aqueous humor formation | Headache, dry mouth, dry nose, altered taste, conjunctivitis, lid reactions, pruritus |
| SECOND-LINE AGENTS | |||
| Cholinergic drugs | Increased aqueous humor outflow | ||
| Muscarinic agonists | Pilocarpine | Miosis, blurred vision | |
| Cholinesterase inhibitors | Echothiophate | Miosis, blurred vision | |
| Carbonic anhydrase inhibitors | Dorzolamide Brinzolamide | Decreased aqueous humor formation | Ocular stinging, bitter taste, conjunctivitis, lid reactions |
If drugs are unable to reduce IOP to an acceptable level, surgical intervention to promote outflow of aqueous humor is indicated. Options include trabeculectomy and laser trabeculoplasty.
Angle-Closure Glaucoma
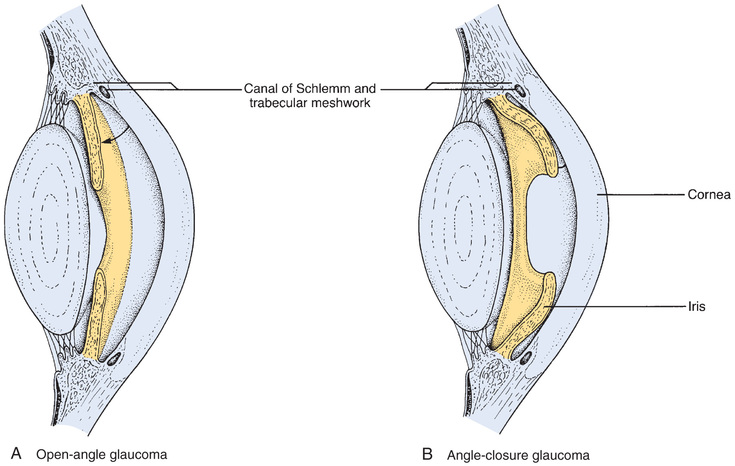
Angle-closure glaucoma is precipitated by displacement of the iris such that it covers the trabecular meshwork, thereby preventing exit of aqueous humor from the anterior chamber. As a result, IOP increases rapidly and to dangerous levels. This disorder is referred to as angle-closure or narrow-angle glaucoma because the angle between the cornea and the iris is greatly reduced (Fig. 84.2). Angle-closure glaucoma develops suddenly and is extremely painful. In the absence of treatment, irreversible loss of vision occurs in 1 to 2 days. This disorder is much less common than open-angle glaucoma.
Treatment consists of drug therapy (to control the acute attack) followed by corrective surgery. A combination of drugs (osmotic agents, short-acting miotics, carbonic anhydrase inhibitors, topical beta-adrenergic blocking agents) is employed to suppress symptoms. After IOP has been reduced with drugs, definitive treatment can be rendered with surgery. Options include iridectomy and laser iridotomy. Both procedures alter the iris to permit unimpeded outflow of aqueous humor.
Drugs Used to Treat Glaucoma
Beta-Adrenergic Blocking Agents
Actions and Use in Glaucoma
Five beta blockers—betaxolol, carteolol, levobunolol, metipranolol, and timolol—are approved for use in glaucoma. Dosing is topical. These agents cause minimal disturbance of vision and are considered first-line drugs for glaucoma, although prostaglandin analogs are becoming favored. Formulations and dosages of the beta blockers are shown in Table 84.2.
TABLE 84.2
Beta Blockers Used in Glaucoma
| Drug | Receptor Specificity | Formulation | Usual Dosage |
| Betaxolol [Betoptic S] | Beta1 | 0.25% suspension | 1 drop twice a day |
| Carteolol | Beta1, beta2 | 1% solution | 1 drop twice a day |
| Levobunolol [Betagan Liquifilm, AKBeta] | Beta1, beta2 | 0.25% solution | 1 drop twice a day |
| 0.5% solution | 1 drop once or twice a day | ||
| Metipranolol [OptiPranolol] | Beta1, beta2 | 0.3% solution | 1 drop twice a day |
| Timolol [Timoptic, Betimol, Istalol] | Beta1, beta2 | 0.25% solution | 1 drop once or twice a day |
| 0.5% solution | 1 drop once or twice a day | ||
| 0.25% gel | 1 drop once a day | ||
| 0.5% gel | 1 drop once a day |
The beta-adrenergic blockers lower IOP by decreasing production of aqueous humor. Reductions in IOP occur with “nonselective” beta blockers (drugs that block beta1 and beta2 receptors) as well as with “cardioselective” beta blockers (drugs that block beta1 receptors only).
Beta blockers are used primarily for open-angle glaucoma. They are suitable for initial therapy as well as maintenance therapy. Beta blockers, in combination with other drugs, are also employed for emergency management of acute angle-closure glaucoma.
The basic pharmacology of the beta blockers is discussed in Chapter 14.
Adverse Effects
Local.
Local effects are generally minimal, although patients commonly complain of transient ocular stinging. Beta blockers occasionally cause conjunctivitis, blurred vision, photophobia, and dry eyes.
Systemic.
Beta blockers can be absorbed in amounts sufficient to cause systemic effects. For example, instilling 1 drop of 0.5% timolol in each eye can produce the same blood level as taking 10 mg of timolol by mouth (the usual starting dose for hypertension). Effects on the heart and lungs are of greatest concern.
Blockade of cardiac beta1 receptors can produce bradycardia and atrioventricular (AV) heart block. Pulse rate should be monitored. Because of their ability to depress cardiac function, beta blockers are contraindicated for patients with AV heart block, sinus bradycardia, and cardiogenic shock. In addition, they should be used with caution in patients with heart failure.
Blockade of beta2 receptors in the lung can cause bronchospasm. Constriction of the bronchi can occur with beta1-selective antagonists as well as with “nonselective” beta-adrenergic blockers—although the risk is greatest with the nonselective agents. Only one ophthalmic beta blocker—betaxolol—is beta1 selective. This drug is preferred to other beta blockers for patients with asthma or chronic obstructive pulmonary disease.
Prostaglandin Analogs
Four prostaglandin analogs are approved for topical therapy of glaucoma. These drugs are as effective as the beta blockers and cause fewer side effects. Accordingly, they are considered first-line medications for glaucoma. Formulations and dosages are shown in Table 84.3.
TABLE 84.3
Prostaglandin Analogs Used in Glaucoma
| Generic Name | Trade Name | Formulation | Usual Dosage |
| Latanoprost | Xalatan | 0.005% solution | 1 drop once daily in the evening |
| Travoprost | Travatan | 0.004% solution | 1 drop once daily in the evening |
| Bimatoprost | Lumigan | 0.01% solution | 1 drop once daily in the evening |
| 0.03% solution | 1 drop once daily in the evening | ||
| Tafluprost | Zioptan | 0.0015% solution | 1 drop once daily in the evening |
Latanoprost
Latanoprost [Xalatan], an analog of prostaglandin F2 alpha, was the first prostaglandin approved for glaucoma and will serve as our prototype for the group. The drug is applied topically to lower IOP in patients with open-angle glaucoma and ocular hypertension. Latanoprost lowers IOP by facilitating aqueous humor outflow, in part by relaxing the ciliary muscle. The recommended dosage is 1 drop (0.005% solution) applied once daily in the evening. At this dosage, latanoprost produces the same reduction in IOP as does timolol twice daily.
Latanoprost is generally well tolerated, and systemic reactions are rare. The most significant side effect is a harmless heightened brown pigmentation of the iris, which is most noticeable in patients whose irides are green-brown, yellow-brown, or blue/gray-brown. The effect is rare in patients whose irides are blue, green, or blue-green. Heightened pigmentation stops progressing when latanoprost is discontinued but does not usually regress. Topical latanoprost may also increase pigmentation of the eyelid and may increase the length, thickness, and pigmentation of the eyelashes. Other side effects include blurred vision, burning, stinging, conjunctival hyperemia, and punctate keratopathy. Rarely, latanoprost may cause migraine.
Other Prostaglandin Analogs
In addition to latanoprost, three other topical prostaglandins are approved for topical therapy of glaucoma. Like latanoprost, these drugs—travoprost [Travatan], bimatoprost [Lumigan], and tafluprost [Zioptan]—reduce IOP by increasing aqueous humor outflow. In clinical trials, these agents were at least as effective as timolol, a representative beta blocker. Interestingly, one drug—travoprost—was more effective in blacks than in nonblacks. Like latanoprost, these prostaglandins can cause a gradual increase in brown pigmentation of the iris, which may be irreversible. In addition, these drugs can increase pigmentation of the eyelid and growth of the eyelashes. In fact, bimatoprost, marketed as Latisse, is used for the specific purpose of increasing eyelash length, darkness, and thickness. With prostaglandins used to treat glaucoma, the most common adverse effect is ocular hyperemia (engorgement of ocular blood vessels). Less commonly, these drugs cause blurred vision, eye discomfort, ocular pruritus, conjunctivitis, dry eye, light intolerance, and tearing.
Alpha2-Adrenergic Agonists
Two alpha2 agonists are approved for glaucoma. One agent—apraclonidine—is used only for short-term therapy. The other agent—brimonidine—has emerged as a first-line drug for long-term therapy.
Brimonidine
Brimonidine [Alphagan P, Alphagan  ] is the first and only topical alpha2-adrenergic agonist approved for long-term reduction of elevated IOP in patients with open-angle glaucoma or ocular hypertension. Effects on IOP are similar to those achieved with timolol. The drug lowers IOP by reducing aqueous humor production and perhaps by increasing outflow. In addition to lowering IOP, brimonidine may delay optic nerve degeneration and may protect retinal neurons from death. This possibility arises from the ability of alpha2 agonists to protect neurons from injury caused by ischemia. The most common adverse effects are dry mouth, ocular hyperemia, local burning and stinging, headache, blurred vision, foreign body sensation, and ocular itching. In contrast to apraclonidine (see later), brimonidine can cross the blood-brain barrier and hence can cause drowsiness, fatigue, and hypotension. (Recall from Chapter 13 that activation of alpha2 receptors in the brain decreases sympathetic outflow to blood vessels, and thereby lowers blood pressure.) Brimonidine can be absorbed onto soft contact lenses. Accordingly, at least 15 minutes should elapse between drug administration and lens installation.
] is the first and only topical alpha2-adrenergic agonist approved for long-term reduction of elevated IOP in patients with open-angle glaucoma or ocular hypertension. Effects on IOP are similar to those achieved with timolol. The drug lowers IOP by reducing aqueous humor production and perhaps by increasing outflow. In addition to lowering IOP, brimonidine may delay optic nerve degeneration and may protect retinal neurons from death. This possibility arises from the ability of alpha2 agonists to protect neurons from injury caused by ischemia. The most common adverse effects are dry mouth, ocular hyperemia, local burning and stinging, headache, blurred vision, foreign body sensation, and ocular itching. In contrast to apraclonidine (see later), brimonidine can cross the blood-brain barrier and hence can cause drowsiness, fatigue, and hypotension. (Recall from Chapter 13 that activation of alpha2 receptors in the brain decreases sympathetic outflow to blood vessels, and thereby lowers blood pressure.) Brimonidine can be absorbed onto soft contact lenses. Accordingly, at least 15 minutes should elapse between drug administration and lens installation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


