16
Drug Therapy of Myocardial Ischemia
This chapter will be most useful after having a basic understanding of the material related to angina at the beginning of Chapter 27, Treatment of Myocardial Ischemia and Hypertension in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. In addition to the material presented here, the 12th Edition contains:
• Table 27-1 Organic Nitrates Available for Clinical Use, which provides information about the preparations, usual doses, and routes of administration of organic nitrates
• The molecular structures of drugs used to treat myocardial ischemia
LEARNING OBJECTIVES
 Understand the mechanisms of action of drugs used to treat myocardial ischemia and relieve symptoms of angina.
Understand the mechanisms of action of drugs used to treat myocardial ischemia and relieve symptoms of angina.
 Understand the goals of treatment based on a knowledge of the underlying cause(s) of angina.
Understand the goals of treatment based on a knowledge of the underlying cause(s) of angina.
 Know which drugs are most effective in treating different types of angina.
Know which drugs are most effective in treating different types of angina.
 Know which drugs are used in combination to treat angina.
Know which drugs are used in combination to treat angina.
 Know the untoward effects and contraindications of the major classes of drugs used to treat angina.
Know the untoward effects and contraindications of the major classes of drugs used to treat angina.
 Know the role of drug-eluting stents to treat patients with acute coronary syndromes.
Know the role of drug-eluting stents to treat patients with acute coronary syndromes.
DRUGS INCLUDED IN THIS CHAPTER
• Antithrombin agents (see Chapter 19)
• Antiplatelet drugs (see Chapter 19)
• β Adrenergic receptor antagonists (see Chapter 7)
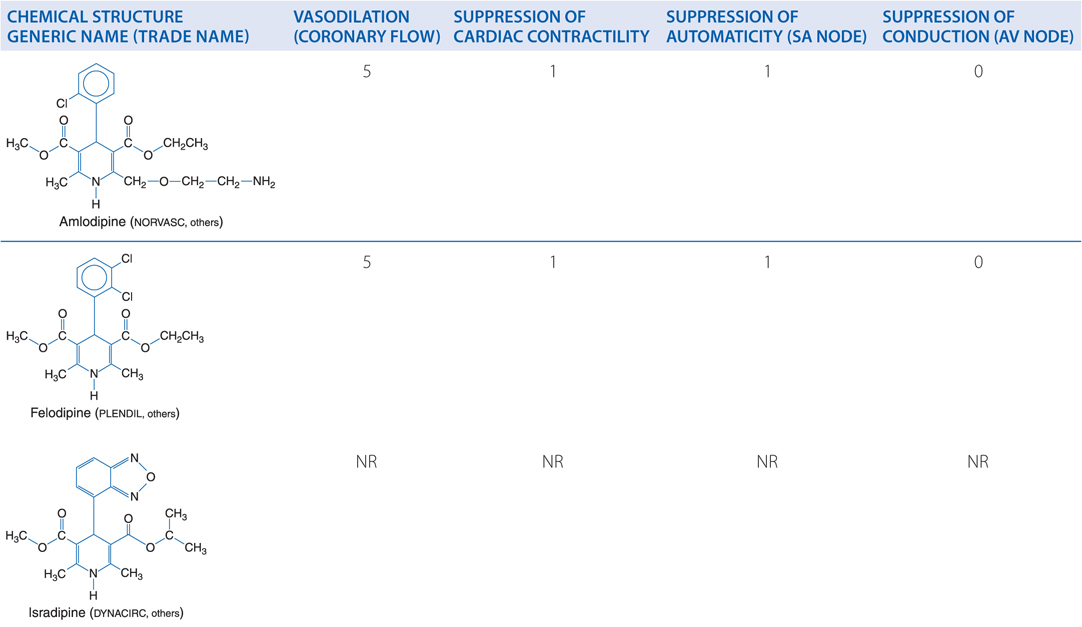
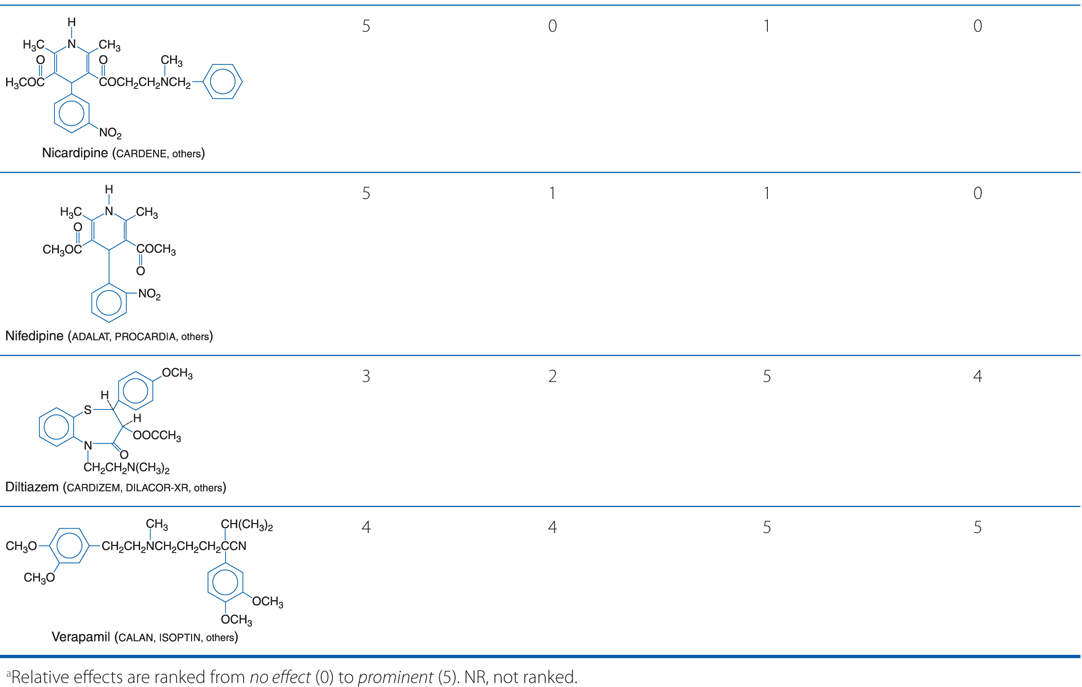
• Numerous dihydropyridines (nifedipine [ADALAT, PROCARDIA, others], amlodipine [NORVASC, others], felodipine [PLENDIL, others], isradipine [DYNACIRC, others], nicardipine [CARDENE, others], nisoldipine, nimodipine, clevidipine, others)
• Diltiazem (CARDIZEM, DILACOR-XR, others)
• Isosorbide dinitrate (ISDN; ISORDIL, SORBITRATE, DILATRATE-SR, others)
• Isosorbide-5-mononitrate (ISMN; IMDUR, ISMO, others)
• Nitroglycerin (glyceryl trinitrate; NITRO-BID, NITROSTAT, NITROL, NITRO-DUR, others)
• Paclitaxel drug-eluting stents
• Ranolazine (RANEXA)
• Sildenafil (VIAGRA, REVATIO)
• Sirolimus drug-eluting stents
• Tadalafil (CIALIS, ADCIRCA)
• Thrombolytic agents (see Chapter 19)
• Vardenafil (LEVITRA)
• Verapamil (CALAN, ISOPTIN, others)
SYMPTOMS OF MYOCARDIAL ISCHEMIA
• Angina pectoris, the primary symptom of ischemic heart disease, is caused by transient episodes of myocardial ischemia that are due to an imbalance in the myocardial oxygen supply–demand relationship (see Figure 16-1).
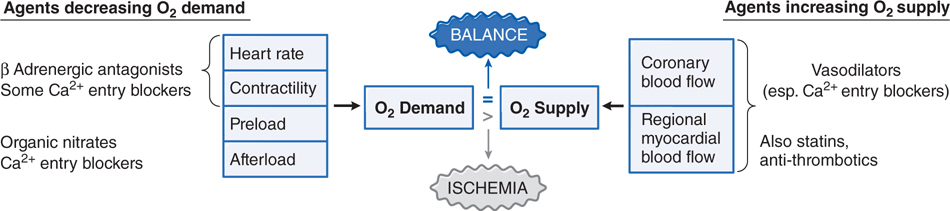
FIGURE 16-1 Pharmacological modification of the major determinants of myocardial O2 supply. When myocardial O2 requirements exceed O2 supply, an ischemic episode results. This figure shows the primary hemodynamic sites of actions of pharmacological agents that can reduce O2 demand (left side) or enhance O2 supply (right side). Some classes of agents have multiple effects. Stents, angioplasty, and coronary bypass surgery are mechanical interventions that increase O2 supply. Both pharmacotherapy and mechanotherapy attempt to restore a dynamic balance between O2 demand and O2 supply.
• Angina pectoris is a heavy, pressing substernal discomfort (rarely described as “pain”) often radiating to the
▶ Left shoulder
▶ Flexor aspect of the left arm
▶ Jaw
▶ Epigastrium
• A significant number of patients note discomfort in a different location or of a different character:
▶ Women, the elderly, and diabetics are more likely to experience myocardial ischemia with atypical symptoms.
▶ Some patients experience myocardial ischemia with no symptoms of angina (silent ischemia), but with electrocardiographic, echocardiographic, or radionuclide evidence of ischemia.
MECHANISMS OF ACTION OF DRUGS USED TO TREAT MYOCARDIAL ISCHEMIA
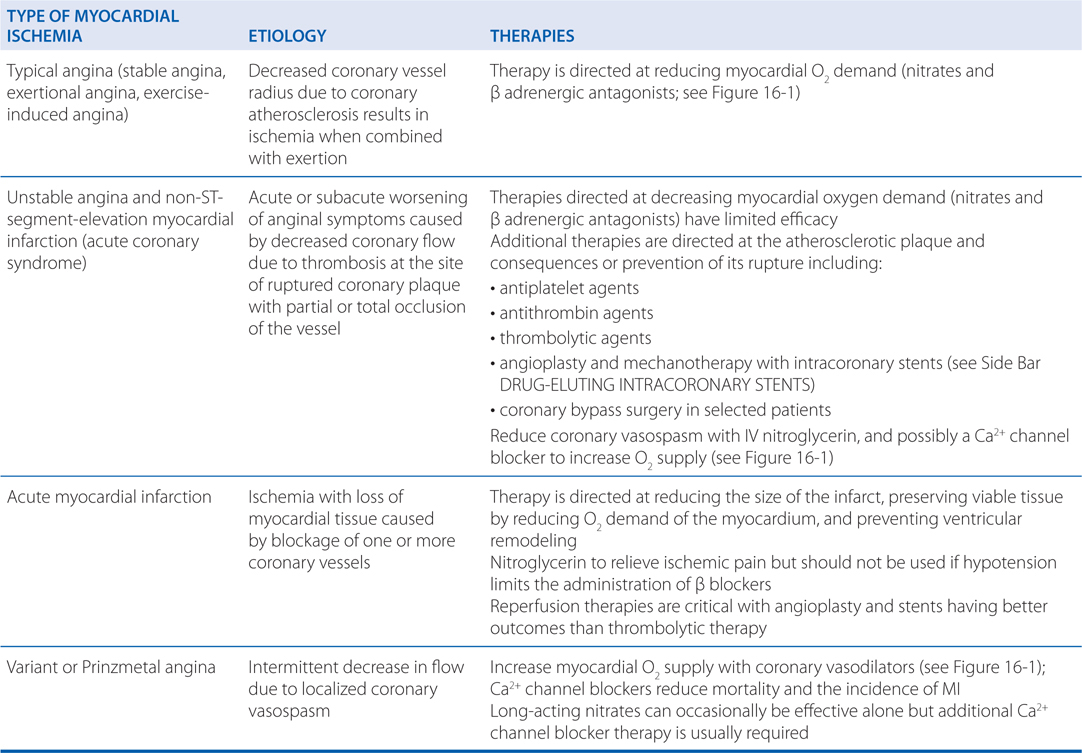
CLASSIFICATION OF MYOCARDIAL ISCHEMIA
INTERACTIONS OF NITRATES WITH PHOSPHODIESTERASE 5 (PDE5) INHIBITORS
• Erectile dysfunction is common in patients with coronary artery disease; thus many men desiring therapy for erectile dysfunction may be receiving antianginal therapy.
• The PDE5 inhibitors (sildenafil, tadalafil, and vardenafil) block the cyclic GMP-specific PDE5 family of phosphodiesterases which are widely expressed in vascular smooth muscle, including the smooth muscle of the corpus cavernosum and penile arteries.
• The accumulation of cyclic GMP in vascular smooth muscle that occurs with NO stimulation of guanylyl cyclase can be enhanced by inhibiting PDE5 activity.
• Given alone, the PDE5 inhibitors cause modest drops in blood pressure, but in men who are taking organic nitrate vasodilators, a fall in blood pressure of more than 25 mm Hg can occur.
• Because of the possibility of extreme hypotension, PDE5 inhibitors are contraindicated for patients receiving any form of nitrate and should not be prescribed to such patients.
• Patients should be questioned about the use of PDE5 inhibitors within the past 24 hours before nitrates are administered; a period longer than 24 hours may be needed to avoid drug interactions, especially with tadalafil which has the longest half-life.
A 52-year-old man who suffers from angina when he climbs stairs or participates in similar activities receives a prescription for nitroglycerin (glyceryl trinitrate). He is instructed to take a tablet 1 or 2 minutes before he expects to climb stairs to prevent the angina.
a. What is the mechanism of action of nitroglycerin that prevents angina from developing in this patient?
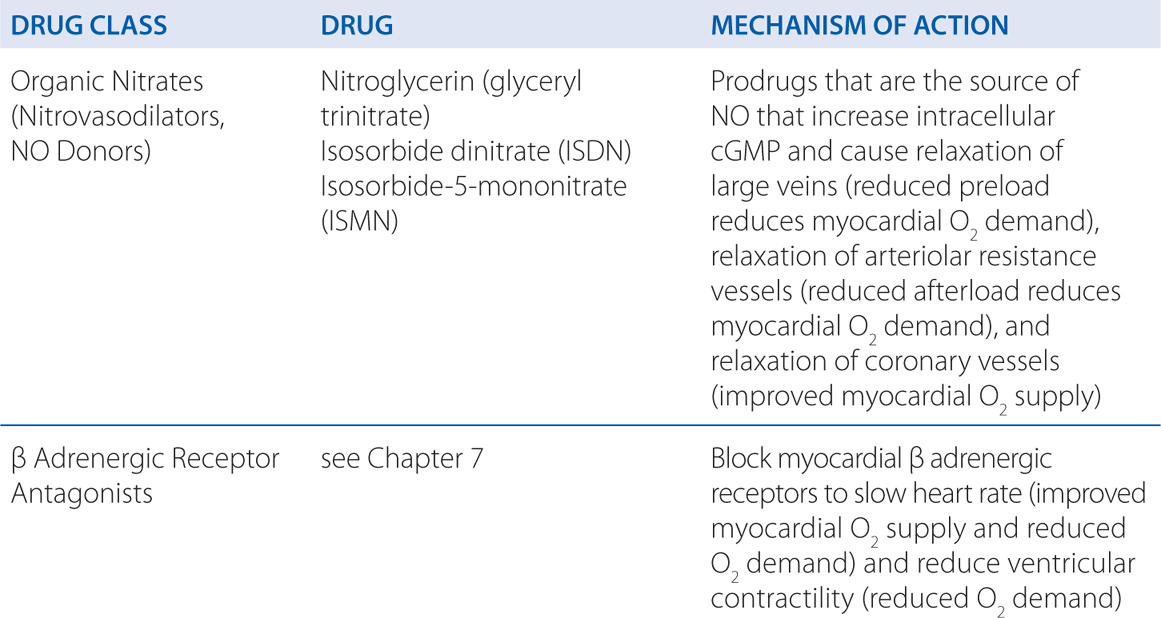
Nitroglycerin and the other organic nitrates used to treat angina are prodrugs that are sources of nitric oxide (NO). NO activates the soluble isoform of guanylyl cyclase, thereby increasing intracellular levels of cyclic GMP and leading to the relaxation of smooth muscle cells in a broad range of tissues. The NO-dependent relaxation of vascular smooth muscle leads to vasodilation. Low concentrations of nitroglycerin preferentially dilate veins more than arterioles. This venodilation decreases venous return, leading to a fall in left and right ventricular chamber size and end-diastolic pressures, but usually results in little change in systemic vascular resistance. Systemic arterial pressure may fall slightly, and heart rate is unchanged or may increase slightly in response to a decrease in blood pressure. Nitroglycerin can dilate epicardial stenoses and reduce the resistance to flow through such areas resulting in an increase in blood flow that would be distributed preferentially to ischemic myocardial regions as a consequence of vasodilation induced by autoregulation.
By their effects on the systemic circulation, the organic nitrates also can reduce myocardial O2 demand (see Figure 16-1). The major determinants of myocardial O2 consumption include left ventricular wall tension, heart rate, and myocardial contractility. Ventricular wall tension is affected by a number of factors that may be considered under the categories of preload and afterload. Organic nitrates decrease both preload and afterload as a result of respective dilation of venous capacitance and arteriolar resistance vessels. The ability of nitrates to dilate epicardial coronary arteries, even in areas of atherosclerotic stenosis, is modest, and the preponderance of evidence continues to favor a reduction in myocardial work, and thus in myocardial O2 demand, as their primary effect in chronic stable angina.
b. How and when should the nitroglycerin be administered to prevent anginal pain?
Anginal pain may be prevented when the drug is used prophylactically immediately prior to exercise or stress. The smallest effective dose should be prescribed. Sublingual organic nitrates should be taken at the time of an anginal attack or in anticipation of exercise or stress. Such intermittent treatment provides reproducible cardiovascular effects. Peak concentrations of nitroglycerin are found in plasma within 4 minutes of sublingual administration; the drug has a t1/2 of 1 to 3 minutes because of rapid and complete first-pass metabolism by the liver. The onset of action of nitroglycerin may be even more rapid if it is delivered as a sublingual spray rather than as a sublingual tablet.
Frequently repeated or continuous exposure to high doses of organic nitrates leads to a marked attenuation in the magnitude of most of their pharmacological effects. The magnitude of tolerance is a function of dosage and frequency of use. In patients who require constant administration of an organic nitrate to prevent symptoms of angina, tolerance can develop rapidly. An effective approach to preventing tolerance or restoring responsiveness is to interrupt therapy for 8 to 12 hours each day, which allows the return of efficacy. It is usually most convenient to omit dosing at night in patients with exertional angina either by adjusting dosing intervals of oral or buccal preparations or by removing cutaneous nitroglycerin.
Patients should be instructed to seek medical attention immediately if 3 tablets taken over a 15-minute period do not relieve a sustained attack because this situation may be indicative of myocardial infarction (MI), unstable angina, or another cause of the pain. Patients also should be advised that there is no virtue in trying to avoid taking sublingual nitroglycerin for anginal pain.
c. What are the expected adverse effects of nitroglycerin therapy?
Untoward responses to the therapeutic use of organic nitrates are almost all secondary to actions on the cardiovascular system. Headache is common and can be severe. It usually decreases over a few days if treatment is continued and often can be controlled by decreasing the dose. Transient episodes of dizziness, weakness, and other manifestations associated with postural hypotension may develop, particularly if the patient is standing immobile, and may progress occasionally to loss of consciousness, a reaction that appears to be accentuated by alcohol. It also may be seen with very low doses of nitrates in patients with autonomic dysfunction. Even in severe nitrate syncope, positioning and other measures that facilitate venous return are the only therapeutic measures required. All the organic nitrates occasionally can produce drug rash.
d. What drug combinations should be avoided?
Erectile dysfunction is a frequently encountered problem whose risk factors parallel those of coronary artery disease. Thus many men desiring therapy for erectile dysfunction already may be receiving (or may require, especially if they increase physical activity) antianginal therapy. The combination of a phosphodiesterase 5 (PDE5) inhibitor (sildenafil, tadalafil, vardenafil) used for erectile dysfunction with organic nitrate vasodilators can cause extreme hypotension (see Side Bar INTERACTIONS OF NITRATES WITH PHOSPHODIESTERASE 5 (PDE5) INHIBITORS). PDE5 inhibitors should not be prescribed to patients receiving any form of nitrate and patients should be questioned about the use of PDE5 inhibitors within 24 hours before nitrates are administered. A period of longer than 24 hours may be needed following administration of a PDE5 inhibitor for safe use of nitrates, especially with tadalafil because of its prolonged t1/2. In the event that patients develop significant hypotension following combined administration of a PDE5 inhibitor and a nitrate, fluids and α adrenergic receptor agonists, if needed, should be used for support.
A 67-year-old woman with mild heart failure (LVEF = 45%) has anginal pain with exercise and is prescribed a β adrenergic blocker.
a. How does therapy with a β adrenergic blocker prevent anginal pain?
The effectiveness of β adrenergic receptor antagonists in the treatment of exertional angina is attributable primarily to a fall in myocardial O2 consumption at rest and during exertion, although there also is some tendency for increased flow toward ischemic regions. The decrease in myocardial O2 consumption is due to a negative chronotropic effect (particularly during exercise), a negative inotropic effect, and a reduction in arterial blood pressure (particularly systolic pressure) during exercise (see Figure 16-1). The reduction in arterial blood pressure is secondary to a drop in cardiac output due to the negative chronotropic and inotropic effects of β blockers.
b. What is the rationale underlying the choice of a β adrenergic blocker for this patient?
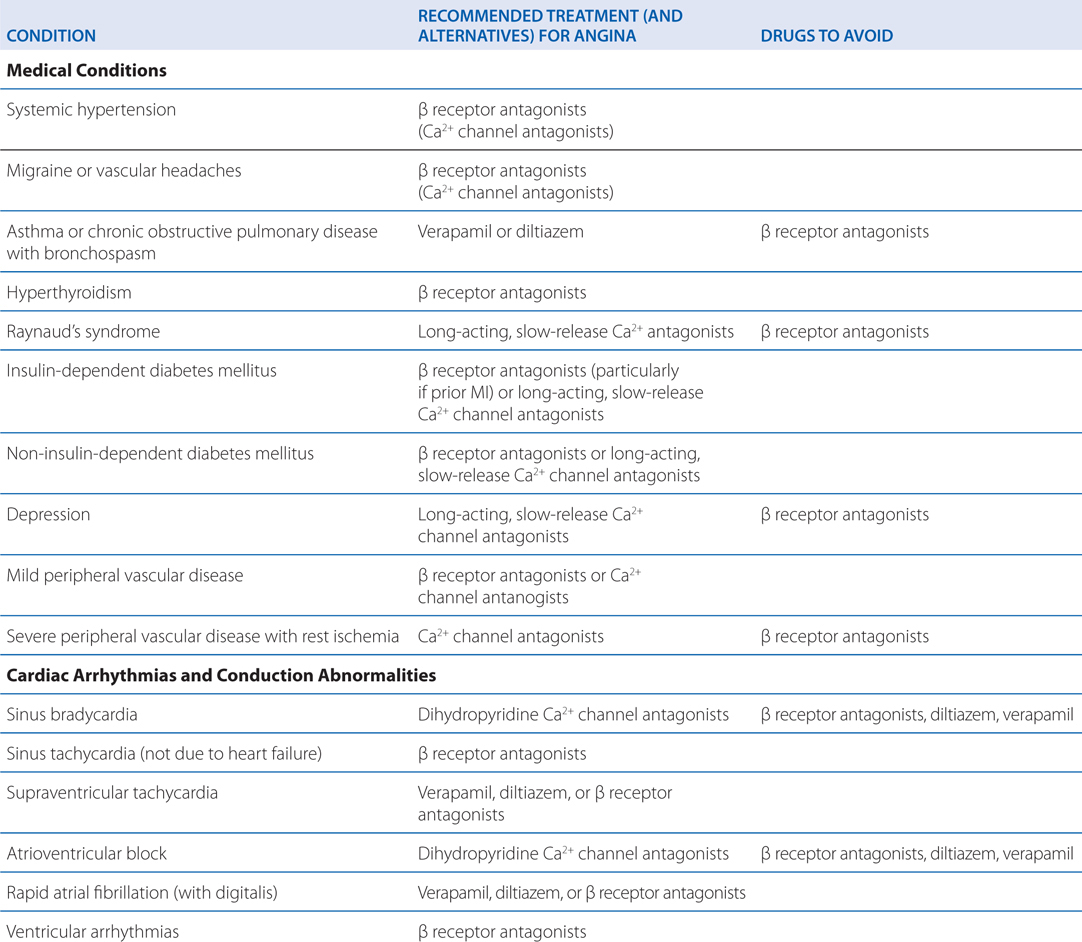
Because there is a proven mortality benefit from the use of β adrenergic receptor antagonists in patients with heart disease, this class of drugs represents the first line of therapy. β Adrenergic receptor antagonists are effective in reducing the severity and frequency of attacks of exertional angina and are recommended for patients with mild heart failure (LVEF ≥40%; Table 16-1). Moreover, several β adrenergic receptor antagonists have been shown to reduce mortality in patients with congestive heart failure and treatment of patients with heart failure with β adrenergic antagonist drugs has become standard therapy for many such patients (see Chapters 12 and 28 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition). Most β adrenergic receptor antagonists appear to be equally effective in the treatment of exertional angina. Timolol, metoprolol, atenolol, and propranolol have been shown to exert cardioprotective effects.
TABLE 16-1 Recommended Drug Therapy for Angina in Patients with Other Medical Conditions
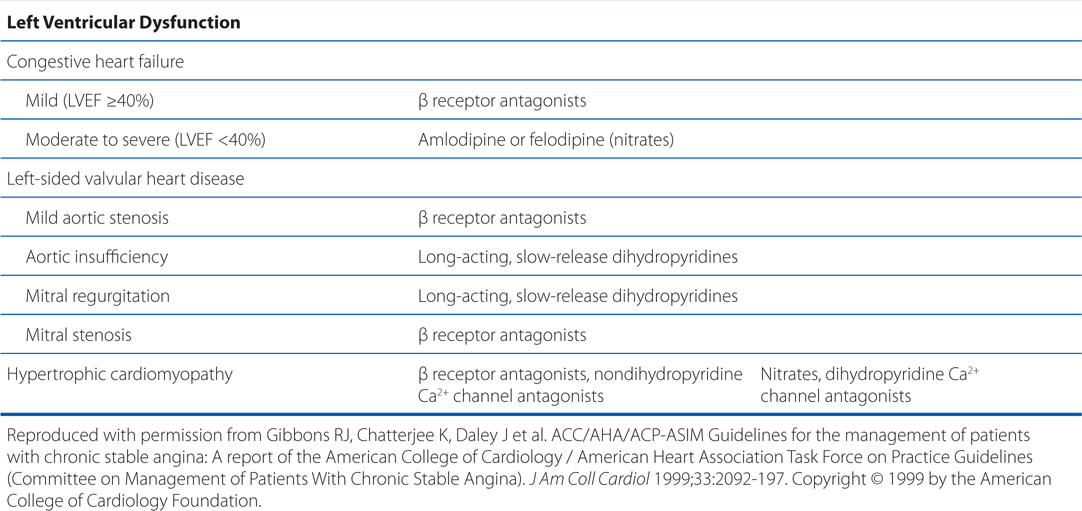
c. If the patient’s angina is not adequately controlled by monotherapy with a β adrenergic receptor antagonist, what other classes of antianginal drugs could be added to the β adrenergic blocker therapy in this patient?
The concurrent use of organic nitrates and β adrenergic receptor antagonists can be very effective in the treatment of typical exertional angina. The additive efficacy primarily is a result of the blockade by one drug of a reflex effect elicited by the other. β Adrenergic receptor antagonists can block the baroreceptor-mediated reflex tachycardia and positive inotropic effects that are sometimes associated with nitrates, whereas nitrates, by increasing venous capacitance, can attenuate the increase in left ventricular end-diastolic volume associated with β receptor blockade. Concurrent administration of nitrates also can alleviate the increase in coronary vascular resistance associated with blockade of β adrenergic receptors.
When angina is not controlled adequately by a β receptor antagonist plus nitrates, additional improvement sometimes can be achieved by the addition of a Ca2+ channel blocker, especially if there is a component of coronary vasospasm. The differences among the chemical classes of Ca2+ channel blockers can lead to important adverse or salutary drug interactions with β receptor antagonists (see text in Chapter 27 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition).
A man with hypertension and occasional symptoms of angina with exercise is prescribed amlodipine.
a. What is the mechanism of action of amlodipine that is beneficial in treating hypertension and angina?
Amlodipine inhibits L-type voltage-sensitive Ca2+ channels in vascular smooth muscle, especially in arterial beds. The basis for the use of Ca2+ channel antagonists in hypertension comes from the understanding that hypertension generally is the result of increased peripheral vascular resistance. All of the Ca2+ channel blockers lower blood pressure by relaxing arteriolar smooth muscle and decreasing peripheral vascular resistance. Ca2+ channel blockers are effective when used alone or in combination with other drugs for the treatment of hypertension.
The utility of Ca2+ channel antagonists in the treatment of exertional, or exercise-induced, angina results from an increase in coronary blood flow owing to coronary arterial dilation, from a decrease in myocardial O2 demand (secondary to a decrease in arterial blood pressure, heart rate, or contractility), or both (see Figure 16-1). Amlodipine, as with other dihydropyridine Ca2+ channel blockers, has potent vasodilator activity but minimal effects on cardiac contractility, SA nodal activity, or AV nodal activity at concentrations that cause vasodilation (Table 16-2). In contrast to the dihydropyridines, verapamil and diltiazem have direct negative inotropic and chronotropic effects (see Table 16-2).
TABLE 16-2 Ca2+ Channel Blockers: Chemical Structures and Some Relative Cardiovascular Effectsa
TREATMENT OF CLAUDICATION AND PERIPHERAL VASCULAR DISEASE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree