20
Drug Therapy of Dyslipidemias
This chapter will be most useful after having a basic understanding of the material in Chapter 31, Drug Therapy for Hypercholesterolemia and Dyslipidemia in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. In addition to the material presented here, the 12th Edition contains:
• Table 31-1 Characteristics of Plasma Lipoproteins which lists the major classes of lipoproteins and their properties
• Table 31-2 Apolipoproteins which describes the properties and functions of apolipoproteins that have well-defined roles in plasma protein metabolism
• Table 31-6 Assessing 10-Year Risk of CVD Events which provides an algorithm for estimating a patient’s risk of a cardiovascular disease (CVD) event (ie, myocardial infarction [MI], stroke, transient ischemic attack [(TIA)], peripheral vascular disease, heart failure)
• Table 31-8 Clinical Identification of the Metabolic Syndrome which provides levels of the five CHD risk factors that define metabolic syndrome
• Table 31-9 Guidelines Based on the LDL-C and Total Cholesterol:HDL-C Ratio for Treatment of Low HDL-C Patients which provides an algorithm for treating patients with low high-density lipoprotein cholesterol (HDL-C) levels
• Table 31-10 Dose (mg) of Stains Required to Achieve Various Reductions in Low-Density-Lipoprotein Cholesterol From Baseline which provides an algorithm for initiating dosing of statins based on baseline low-density lipoprotein cholesterol (LDL-C) levels
• The molecular structures of drugs used to treat dyslipidemias
LEARNING OBJECTIVES
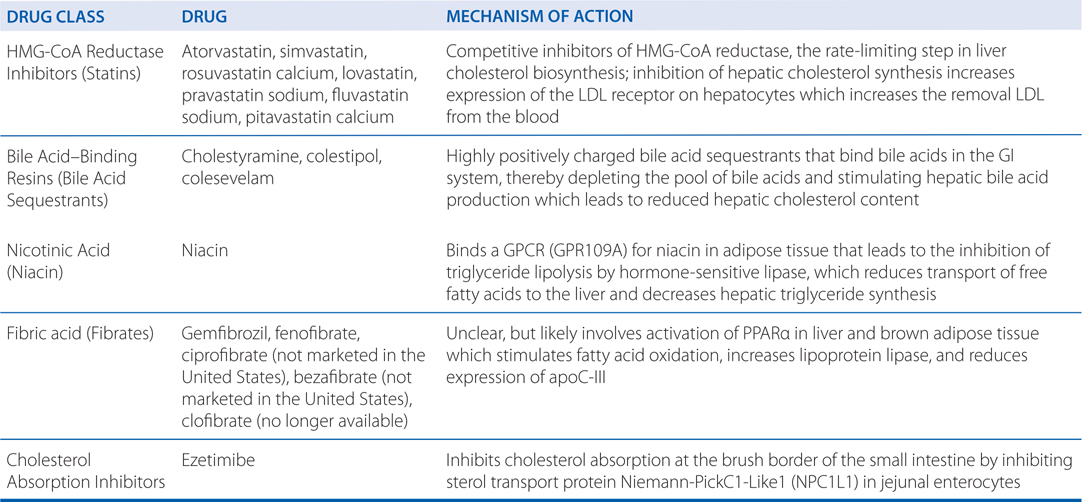
 Understand the mechanisms of action of drugs used to treat dyslipidemia.
Understand the mechanisms of action of drugs used to treat dyslipidemia.
 Know the untoward effects of drugs used to treat dyslipidemias.
Know the untoward effects of drugs used to treat dyslipidemias.
 Know which patients with dyslipidemias should be treated and when treatment should be initiated.
Know which patients with dyslipidemias should be treated and when treatment should be initiated.
 Know which drugs are most effective in treating patients with different dyslipidemias.
Know which drugs are most effective in treating patients with different dyslipidemias.
 Know which drugs can be used in combination to treat dyslipidemias.
Know which drugs can be used in combination to treat dyslipidemias.
 Know the effects of treatment on lowering the 10-year risk of a CVD event, and how to set treatment goals based on primary and secondary prevention of a CVD event.
Know the effects of treatment on lowering the 10-year risk of a CVD event, and how to set treatment goals based on primary and secondary prevention of a CVD event.
DRUGS INCLUDED IN THIS CHAPTER
• Atorvastatin (LIPITOR)
• Bezafibrate (not marketed in the United States)
• Cholestyramine (QUESTRAN, CHOLYBAR, others)
• Ciprofibrate (not marketed in the United States)
• Clofibrate (no longer available)
• Colesevelam (WELCHOL)
• Colestipol (COLESTID, others)
• Ezetimibe (ZETIA)
• Ezetimibe/simvastatin (VYTORIN)
• Fenofibrate (TRICOR, TRIGLIDE)
• Fluvastatin (LESCOL)
• Gemfibrozil (LOPID)
• Lovastatin (MEVACOR)
• Niacin (NIACOR, NIASPAN, others)
• Pitavastatin (LIVALO)
• Pravastatin (PRAVACHOL)
• Rosuvastatin (CRESTOR)
• Simvastatin (ZOCOR)
MECHANISMS OF ACTION OF DRUGS USED TO TREAT DYSLIPIDEMIAS
A 58-year-old man sees his physician for a routine checkup. He is in good health with no symptoms or complaints. He does not have a family history of premature heart disease, although his paternal grandfather suffered a nonfatal heart attack when he was 67. Just prior to the checkup, he provides fasting blood samples for lipid profiles. His plasma cholesterols are: total cholesterol, 203 mg/dL; HDL cholesterol, 52 mg/dL; LDL cholesterol, 130 mg/mL; VLDL cholesterol, 21 mg/dL. His triglycerides are 148 mg/dL. His fasting serum glucose is in the normal range and his blood pressure is 128/75. He is not currently taking any medications, has never smoked, and usually has 1 or 2 glasses of wine with dinner, but consumes no other alcoholic beverages.
a. What is this patient’s 10-year risk of a CVD event?
Table 31-6 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition provides an algorithm for estimating the 10-risk of coronary vascular disease (CVD) events based on data from the Framingham Heart Study. The risk prediction for a CVD event will exceed the risk of a coronary heart disease (CHD) event. For this patient, the risk factors and CVD points associated with each risk factor are: age (10 points); HDL (–1 point); total cholesterol (2 points); systolic blood pressure (0 points); smoker (0 points), diabetic (0 points). The total number of CVD points is 11, placing his 10-year risk of a CVD event at 11.2%.
TRADITIONAL MAJOR RISK FACTORS FOR CORONARY HEART DISEASE
• Elevated LDL-C (>160 mg/dL; see Tables 20-1 and 20-2)
TABLE 20-1 Treatment Based on LDL-C Levels (2004 Revision of NCEP Adult Treatment Panel III Guidelines)
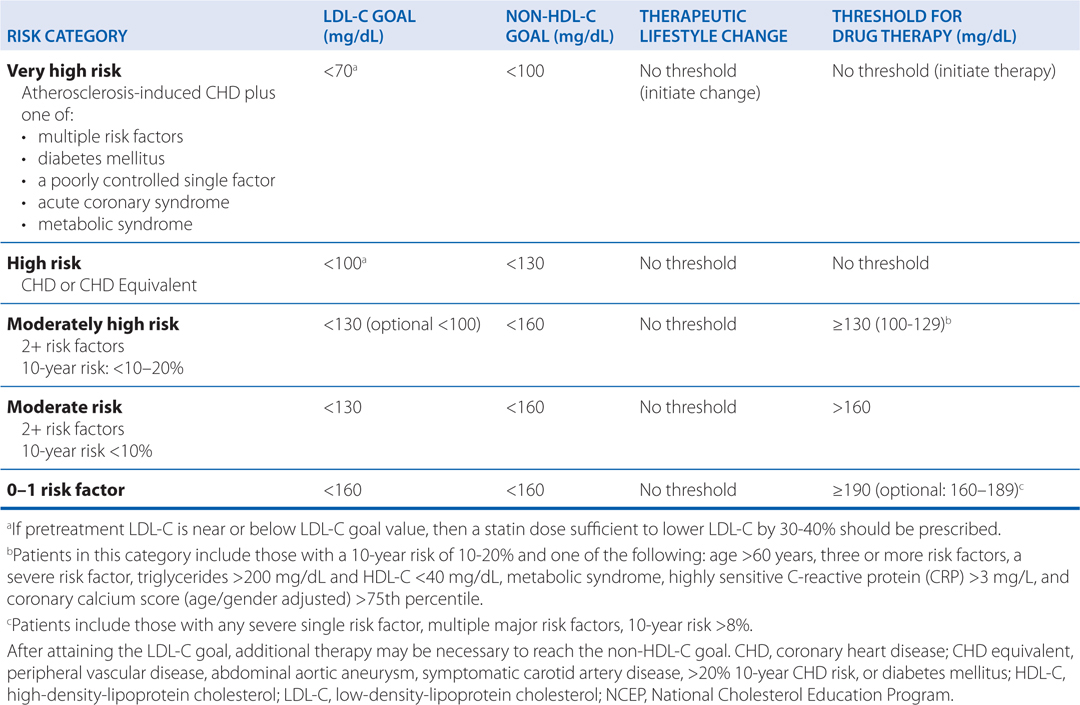
TABLE 20-2 Classification of Plasma Lipid Levels (mg/dL)a
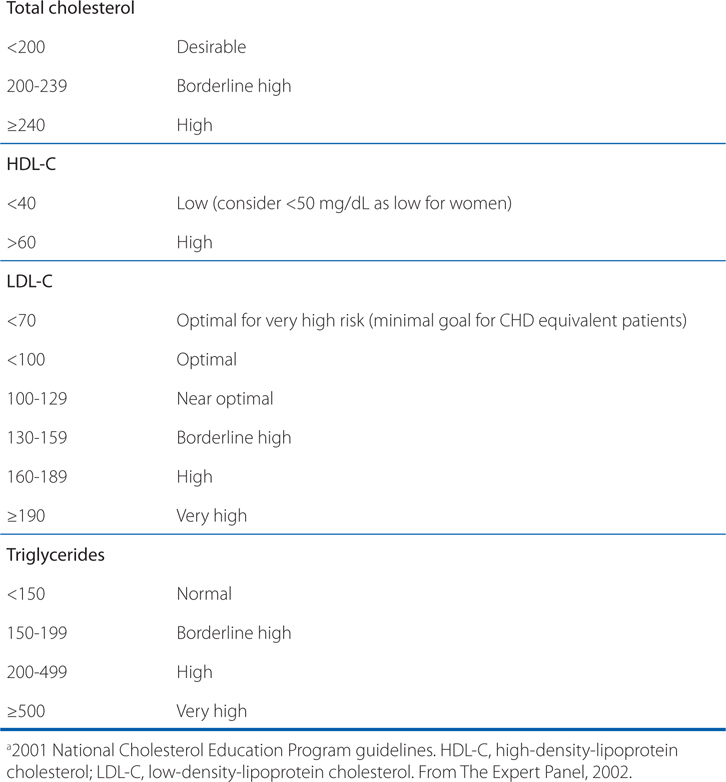
• Reduced HDL-C (<40 mg/dL; see Table 20-2)
• Cigarette smoking (within the preceding 30 days)
• Hypertension (blood pressure ≥140/90 mm Hg or use of antihypertensive medication, regardless of blood pressure)
• Type 2 diabetes mellitus
• Advancing age (men >45 years of age or women >55 years of age)
• Family history of premature coronary heart disease (CHD) events (men <55 years; women <65 years) in a first-degree relative
• Obesity (body mass index [BMI] >25 kg/m2 and waist circumference >40 in [men] or >35 in [women])
HIGH-RISK DYSLIPIDEMIAS (SEE TABLE 20-2)
• High total cholesterol (≥240 mg/dL)
• High LDL-C (>160 mg/dL)
• Low HDL-C (<40 mg/dL)
• Severe hypertriglyceridemia (≥500 mg/dL)
PRIMORDIAL PREVENTION GUIDELINES (TO PREVENT DEVELOPMENT OF CVD RISK FACTORS)
• 150 min/wk of moderate intensity exercise (walking 20-30 min/d)
• Reducing total calories from fat to less than 30%, with saturated and transfat to less than 7%
• Consuming less than 300 mg cholesterol/d
• Eat a variety of oily fish at least twice a week
• Eat oils/foods rich in α-linolenic acid
• Restricting sugary beverages to less than 36 oz/wk for a person consuming 2000 Kcal daily
b. What, if anything, can be done to reduce this patient’s risk of a CVD event?
This patient’s largest CVD risk is his age, which is not a modifiable risk factor. Another risk factor which cannot be modified is his sex; a woman of the same age with all the same lipid, blood pressure, and history would have a 10-year risk of a CVD event of 6.3%. Based on Table 31-6 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition, the modifiable risk factors for this patient are his blood lipids and his systolic blood pressure. With optimal blood lipids and systolic blood pressure, his CVD points would be reduced to 6 points and his 10-year risk of a CVD event would be reduced to 4.7%.
c. What are the treatment options to maximally reduce this patient’s 10-year CVD risk?
The first option is for the patient to adopt changes in exercise and diet (see Side Bar PRIMORDIAL PREVENTION GUIDELINES). Such lifestyle changes can be effective in lowering blood pressure and improving blood lipid profiles. If lifestyle changes do not adequately improve blood lipid profiles, it may be prudent to start the patient on drugs that lower serum cholesterol (based on Table 20-1). To reach optimal levels of total cholesterol and LDL-C in this patient (<200 mg/dL and <100 mg/dL, respectively; see Table 20-2), the lowest dose of a statin drug should be sufficient (see Table 31-10 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition).
d. What is the mechanism(s) by which statins reduce CVD risk?
The statins competitively inhibit 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, the early rate-limiting step in hepatic cholesterol biosynthesis. They are the most effective and best-tolerated agents for treating dyslipidemias. By inhibiting hepatocyte cholesterol synthesis, the statins induce an increase in the expression of LDL receptors on hepatocytes. The greater number of LDL receptors on the surface of hepatocytes facilitates the removal of LDL from the blood, which lowers LDL-C levels. High levels of LDL-C are associated with a high risk of CVD.
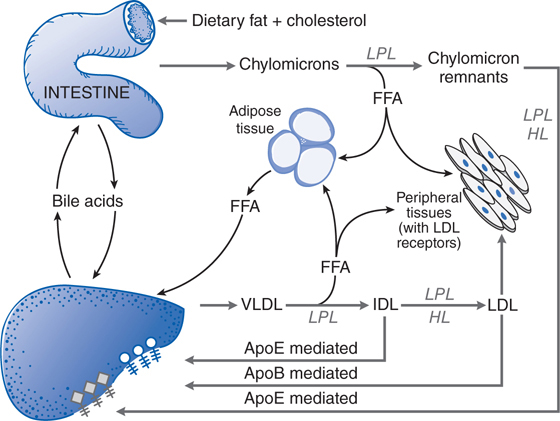
There is also evidence that statin-induced increases in hepatocyte LDL receptors also enhance the removal of circulating LDL precursors, VLDL, and IDL (see Figure 20-1). Statin-mediated reduction in hepatic cholesterol synthesis also reduces hepatic production of VLDL, which can reduce serum triglyceride levels.
FIGURE 20-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree