Fig. 22.1
Proximal nail fold epithelium (200×)
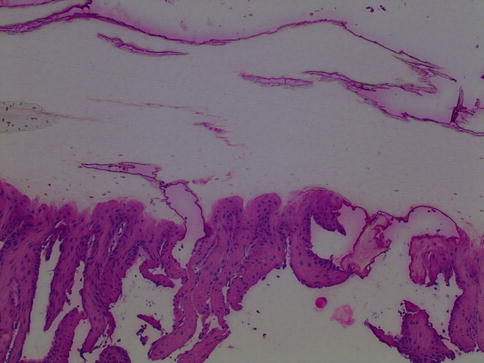
Fig. 22.2
Nail plate with nail bed epithelium (1000×)
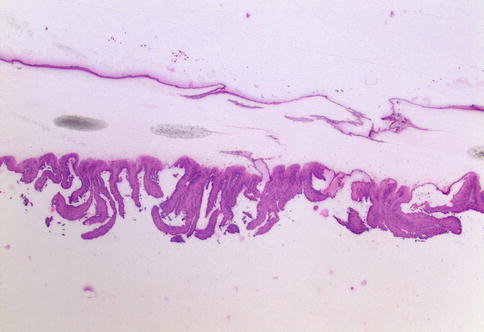
Fig. 22.3
Nail plate with nail bed epithelium (400×)
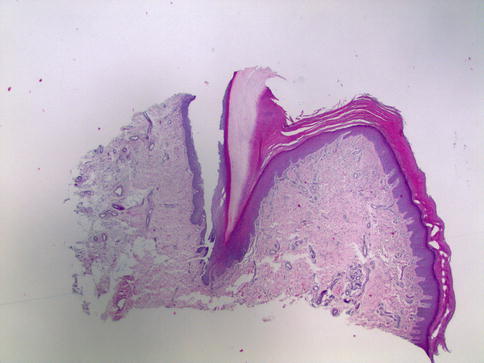
Fig. 22.4
Nail matrix lining the proximal portion of the nail fold invagination (200×)
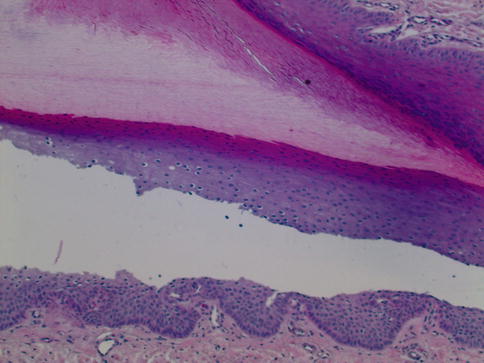
Fig. 22.5
Nail matrix epithelium (1000×)
Generalized Nail Changes
Beau’s Lines/Onychomadesis
The eponymously named dystrophy was first described in 1846 by Joseph Honore Simone Beau. Beau’s lines can be described as a “hiccup” in the mitotic machinery of the nail, the matrix epithelium (Fig. 22.6). A pause or halt of mitotic activity manifests as a depression along the transverse axis of the nail plate. As mitotic activity resumes, the line will progress, as many other nail disorders such as splinter hemorrhages do, as the nail plate extends. The significance of Beau’s lines is their ability to document the insult by the depth and length of the depression. Depth indicates the amount of damage to the matrix, and the length of the depression indicates the insult’s duration.


Fig. 22.6
Beau’s lines bordering on onychomadesis
Beau’s lines can result singly from trauma. Suspicion for a drug-related or systemic cause should arise when Beau’s lines arise in multiple, (up to all 20) nails simultaneously, or present with repeated episodes. Beau’s lines are most often created by drugs that target the nail matrix epithelium or affect its highly active mitotic turnover. Therapeutic measures most commonly responsible for these events are chemoradiation therapy and retinoids. Theoretically, any chemotherapeutic drug can affect the body’s highly active epithelium, such as the gastrointestinal tract or nail matrix.
Onychomadesis is detachment of the nail plate occurring at the proximal nail bed or fold and subsequent shedding for the nail. Onychomadesis can occur when an insult, such as one creating Beau’s lines, is carried to its inevitable conclusion. In this setting, the insult creating mitotic arrest has become severe enough to result in structural instability of the nail plate, and the nail plate is detached while the new nail grows out.
Onychomadesis can occur spontaneously or after infections such as hand, foot, and mouth disease. Drug-induced onychomadesis can be due to a lengthening list of potential causes. Chemotherapeutics and retinoids inducing Beau’s lines can also be a cause of onychomadesis. There have also been reports of anticonvulsants such as carbamazepine and valproic acid causing onychomadesis.
While drugs have been well documented to cause onychomadesis, the possibility exists that severe drug allergy can also induce the process via an inflammatory route. Cases have been shown to occur, such as during critical illness. There exists a documented case of onychomadesis occurring following an allergic response to penicillin.
Onycholysis
Onycholysis means the detachment of the nail plate from the nail bed. This process can occur from destruction of the nail bed’s viable epithelium or destruction of cell-to-cell adhesion molecules. Onycholysis, in contrast to onychomadesis, occurs distally from the nail bed or hyponychium, rather than proximally at the nail fold and nail matrix. It manifests as transverse white discoloration of the nail and is common in psoriasis.
Onycholysis has been associated with infection, trauma, psoriasis, photo reactions, and drugs (Table. 22.1). Drugs have been shown to cause onycholysis in combination with photo exposure, or as a sole agent. Therapeutics causing onycholysis include tetracyclines, fluoroquinolones, and psoralens.
Table 22.1
Causes/manifestations of onycholysis
Cause | Nail clues |
|---|---|
Psoriasis | Erythematous border Oil spots, salmon spots, pitting |
Lichen planus | Nail thinning and fissuring Pterygium (winged nails with central groove) |
Connective tissue disease | Proximal nail fold capillary abnormalities |
Onychomycosis | Yellow discoloration/streaks Toenails |
Pompholyx | Fingernails, most digits |
Tumors | One digit, subungual mass |
Drugs | All/most nails Hemorrhagic changes |
Trauma | Usually fingernails Transverse leukonychia |
Idiopathic | Usually fingernails Chronic paronychia frequently |
Drug-induced Nail Dyspigmentation
A wide range of medications can cause pigmentary changes of the nail, affecting several to all nails. The color changes range from leukonychia (true and apparent) to brown pigmentation. Nail pigmentation may occur from deposition of the drug within either the nail plate or dermis (the latter of which may also be associated with cutaneous and mucosal pigmentation).
Leukonychia
True leukonychia (transverse) results from damage to keratinocytes in the distal nail matrix, which causes failure of maturation and retention of nuclei. Thus, transverse leukonychia occurs from the reflection of light, and is characterized by 1–2 mm transverse bands (each nail can have one or more). Affected nails will present with transverse leukonychia at the same site, indicating simultaneous damage to matrix keratinocytes (Fig. 22.7). The most common cause of transverse leukonychia is chemotherapy agents, most commonly doxorubicin, cyclophosphamide, and vincristine. Other agents include arsenic, fluorine, retinoids, cortisone, sulfonamides, pilocarpine, and trazodone. Arsenic and thallium poisoning will both present with transverse leukonychia involving the entire width of the nail plate.


Fig. 22.7
Leukonychia bands on multiple nails
Apparent leukonychia results from drug-induced damage to the nail bed. Alterations of blood flow to the nail bed will cause changes from the normal pink color seen. Half-and-half nails show proximal white discoloration of the nail that blends with the lunula (and distal portion retains the pink color). Muehrcke’s lines are transverse white bands that alternate with bands of normal pink colored nail bed (Fig. 22.8).


Fig. 22.8
Muehrke’s nails showing transverse white bands
Muerhcke’s Nails
Multiple paired white transverse lines
Oriented parallel to the lunula
Associations: Chronic hypoalbuminemia, nephrotic syndrome
Both leukonychia and Muehrcke’s nail changes are asymptomatic, and the mechanism is poorly understood. They occur most commonly during chemotherapy administration and resolve upon discontinuation.
Brown Nail Dyspigmentation (Melanin-Induced)
Drug-induced damage to melanocytes in the nail matrix can stimulate melanin production, particularly in darker-skinned individuals (Figs. 22.9 and 22.10). Longitudinal melanonychia results from stimulation of a small cluster of melanocytes, whereas the entire nail plate develops pigmentation if there is diffuse melanocyte activation. This is a common side effect of chemotherapy; in fact, repeated cycles can produce transverse leukonychia (suggesting intermittent melanocyte stimulation corresponding to the rounds of chemotherapy). Bleomycin, cyclophosphamide, doxorubicin, daunorubicin, fluorouracil (also lunular pigmentation), and hydroxyurea (also lunular pigmentation) are most commonly associated with melanonychia. Other sources of melanonychia include psoralens, methotrexate, radiation therapy, imatinib, and zidovudine (which can present with diffuse dark brown melanonychia or blue lunula).
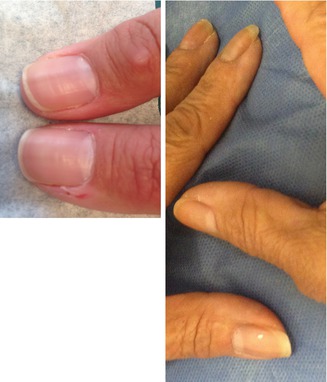
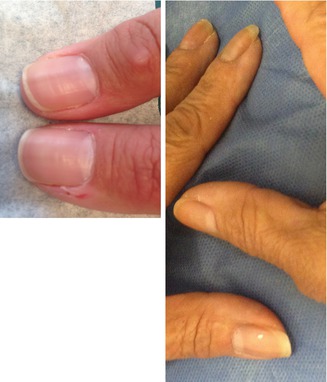
Figs. 22.9 and 22.10
Examples of melanonychia
Drug-induced melanonychia is generally reversible, though the clinician should be aware that it can takes years after cessation of the offending drug for melanin production to stop. This has to be distinguished from melanoma of the nail unit (subungual melanoma) that also presents with melanonychia (Fig. 22.11). The clinical presentation with the irregular pigmentation and involvement of the adjacent nail fold (Hutchinson sign) can help to distinguish melanoma from drug-induced pigmentation. In clinically ambiguous cases, a biopsy of the nail matrix and nail bed can be useful.
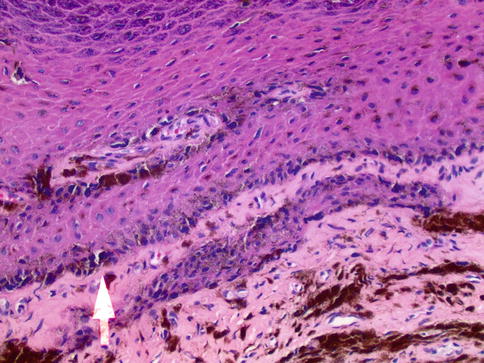
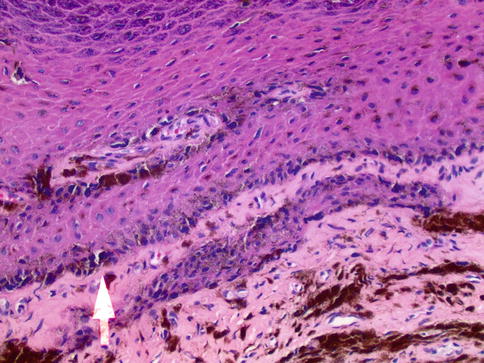
Fig. 22.11
Melanoma of the nail bed. Arrow shows contiguous proliferation of Hyperchromatic, enlarged melanocytes in the nail bed epithelium
Non-Melanin-induced Nail Dyspigmentation
Drug excretion of deposition within the nail plate can cause pigmentation changes independent of melanocyte stimulation. Discoloration occurs in the nail plate and/or the nails (Tables. 22.2 and 22.3).
Table 22.2
Exogenous agents causing discoloration of the nail plate
Agent | Discoloration |
|---|---|
Mercury products | Gray-black |
Resorcinol
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|