http://evolve.elsevier.com/McCuistion/pharmacology
Objectives
• Discuss the metric and household systems of measurement.
• Convert larger units to smaller units and smaller units to larger units within the metric system.
• Convert larger units to smaller units and smaller units to larger units within the household system.
• Convert between metric and household measurements.
Metric System
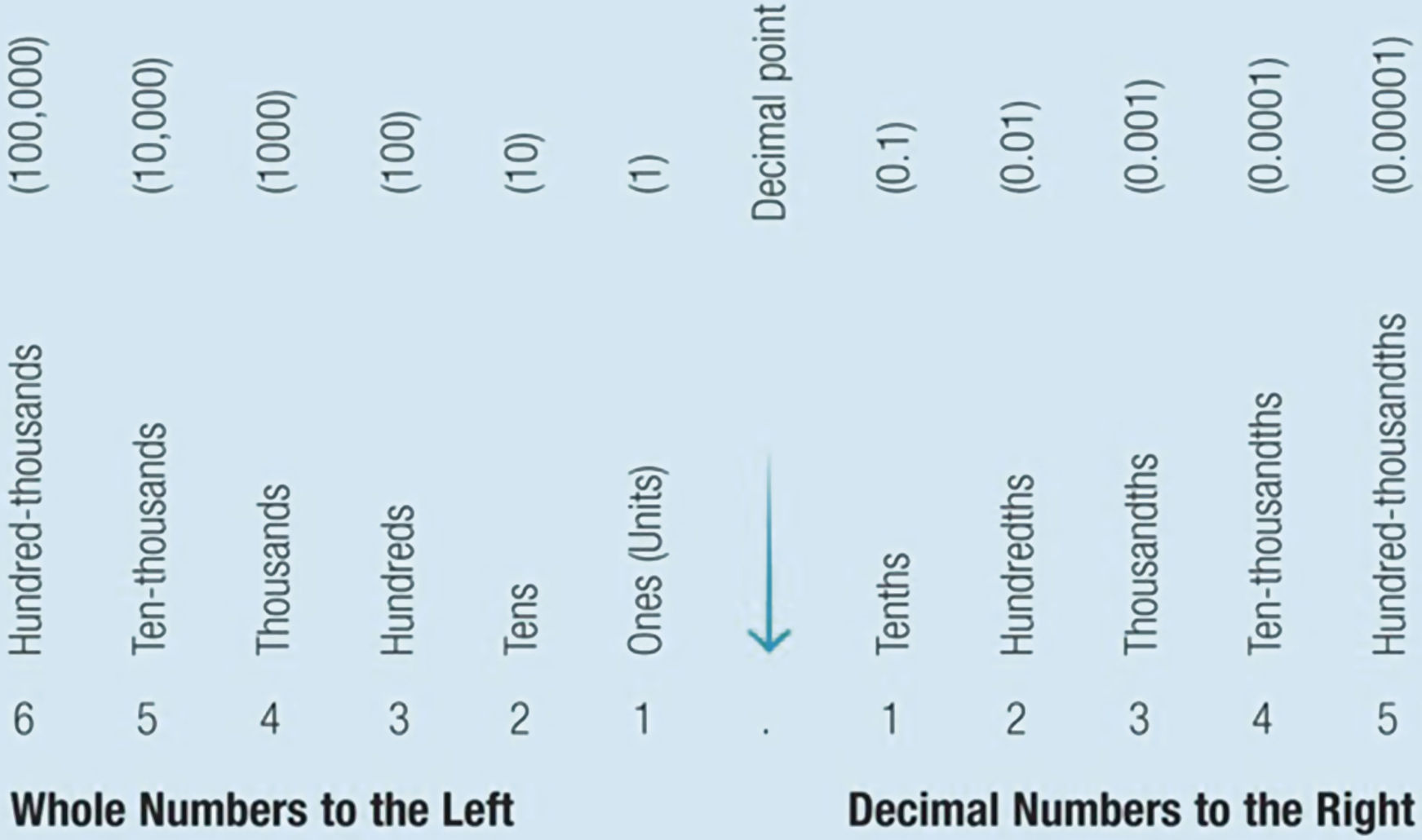
The metric system is a decimal system based on the power of 10. The basic units of measure used in dosage calculations include the gram (g, gm, G, Gm) for weight, liter (L) for volume, and meter (m, M) for linear measurement or length. Prefixes such as nano, micro, milli, centi, and kilo indicate the size of the units in powers of 10 of the base unit and stand for a specific degree of magnitude: for instance, kilo stands for thousands, milli for one thousandth, and centi for one hundredth. To be able to convert a quantity, one of the values must be known, such as a gram (g, G), liter (l, L), meter (m), milligram (mg), milliliter (mL), millimeter (mm), or microgram (mcg). Grams, liters, and meters are larger units, whereas milligrams, milliliters, millimeters, and micrograms are smaller units. Because the conversion between degrees of magnitude always involves multiplying by a power of 10, converting from one magnitude to another is relatively easy.
Conversions Within the Metric System
Common conversions used to calculate drug dosages using the metric system are listed in Table 11A.1.
Grams and milligrams are related by three factors of 10 according to this relationship. In the first illustration below, the larger unit (gram) is converted to the smaller unit (milligram). In the second illustration, the smaller unit is converted to the larger unit.
1g=1mg×103=1000mg
and
1000mg=1 g×10−3=1g
The easiest way to convert larger units to smaller units is to move the decimal point the appropriate number of spaces to the right. In the illustration below, grams have been converted to milligrams by moving the decimal point three spaces to the right:
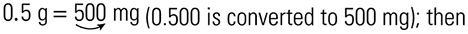
To convert smaller units to larger units, move the decimal point the appropriate number of spaces to the left. In the illustration below, milligrams have been converted to grams by moving the decimal point three spaces to the left (thousandths):
Remember: When changing larger units to smaller units, move the decimal point to the right; when changing smaller units to larger units, move the decimal point to the left. There should always be a zero (0) placed before the decimal point, called a leading zero, to alert the reader that the number is less than 1. For example, 0.5 clearly indicates a value of ½. If the number was to be written as .5, the reader could mistake the number for 5. Do not leave extraneous zeroes after a decimal point (trailing zeroes). The reader may perceive a number that is many times larger than the desired dose. For example, 1.0 could be misread as 10.
Household System
Because of the lack of standardization of spoons, cups, and glasses, household measurement is not as accurate as the metric system, therefore measurements are approximate (Table 11A.2). According to the official U.S. Pharmacopeia, a teaspoon (t) is considered to be equivalent to 5 mL in the metric system. Three teaspoons equal 1 tablespoon (T), therefore 1 T equals 15 mL. Ounces (oz) are fluid ounces in the household measurement system, and there are 2 T in 1 oz therefore 1 ounce equals 30 mL in the metric system.
TABLE 11A.2
| 1 measuring cup | = | 8 oz or 240 mL (1 oz = 30 mL) |
| 1 medium-size glass (tumbler size) | = | 8 oz or 240 mL |
| 1 ounce (oz) | = | 2 tablespoons or 30 mL |
| 1 tablespoon (T) | = | 3 teaspoons or 15 mL |
| 1 teaspoon (t) | = | 60 drops (60 gtt) |
Conversions Within the Household System
When converting larger units to smaller units within the household system, multiply the requested number by the basic equivalent value.
Because household measurements are not as accurate as the metric measurements, instruct patients and caregivers to obtain an approved drug-measuring device to dispense liquid medicine, such as the following:

Answers to Practice Problems
Section 11B
Calculation Methods—Enteral and Parenteral Drug Dosages
Key Terms
basic formula (BF), p. 117
body surface area (BSA), p. 125
body weight (BW), p. 124
controlled substance, p. 114
dimensional analysis (DA), p. 119
drug label, p. 117
fractional equation (FE), p. 118
ratio and proportion (RP), p. 117
square root method, p. 125
trade name, p. 114
units, p. 120
Objectives
• Interpret drug labels.
• Calculate drug dosages using the basic formula, the ratio and proportion/fractional equation method, and the dimensional analysis method.
• Convert all measures to the same system and unit of measure within the system before calculating final drug dosages.
• Calculate drug dosages according to body weight.
• Calculate drug dosages according the body surface area using the West nomogram.
• Calculate drug dosages according the body surface area using the square root method.
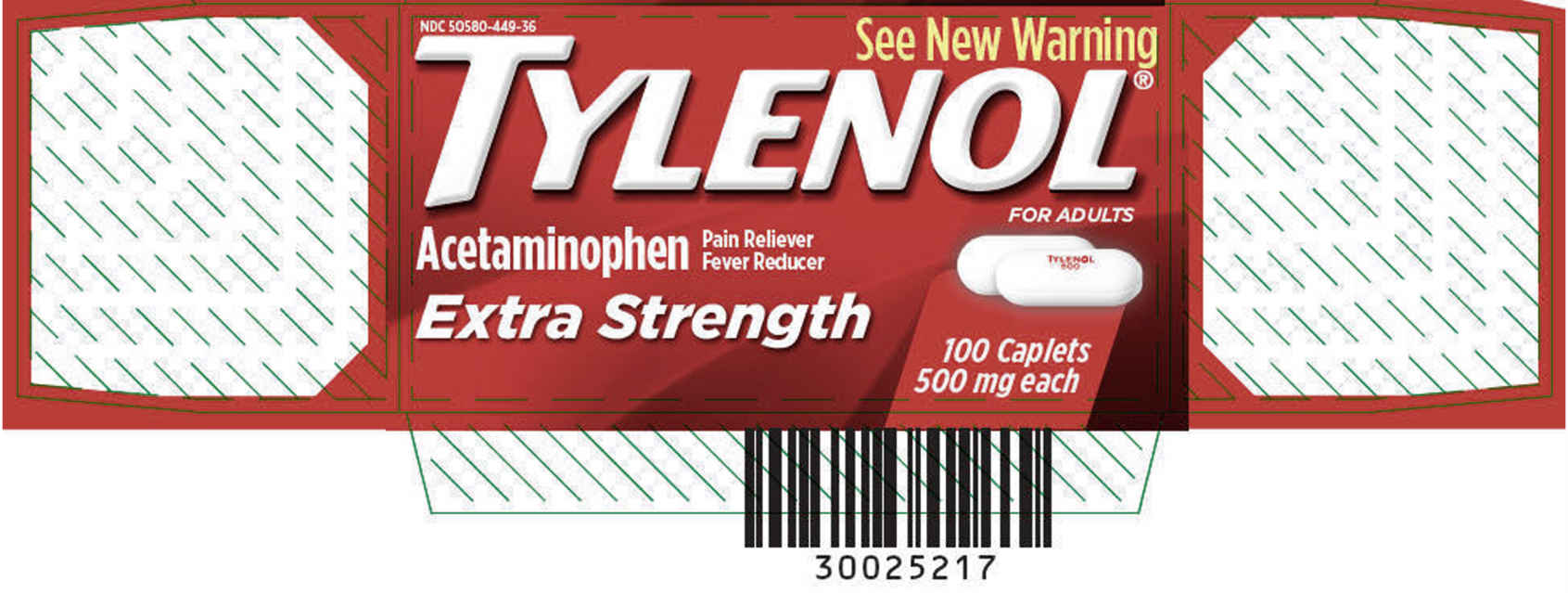
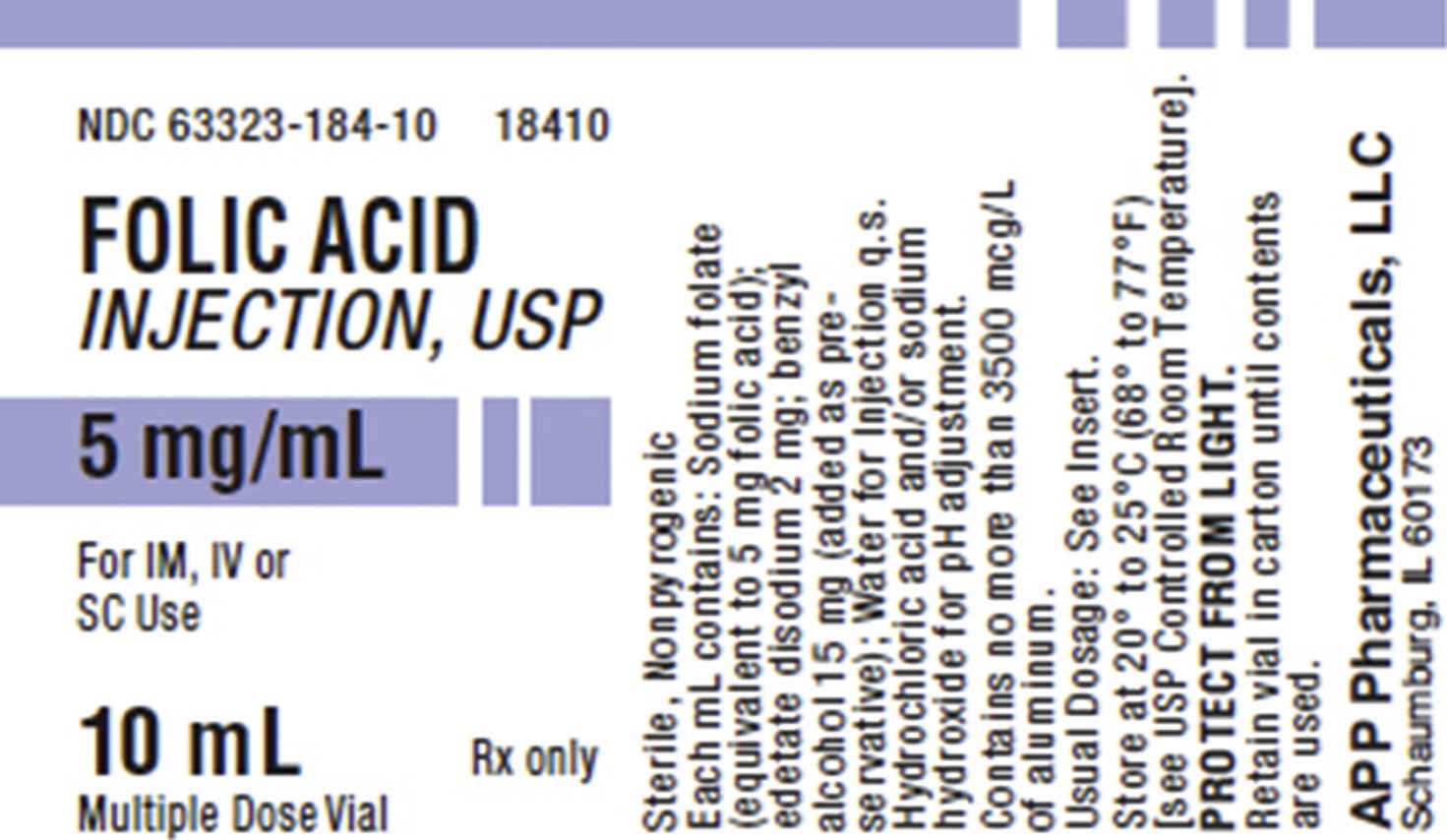
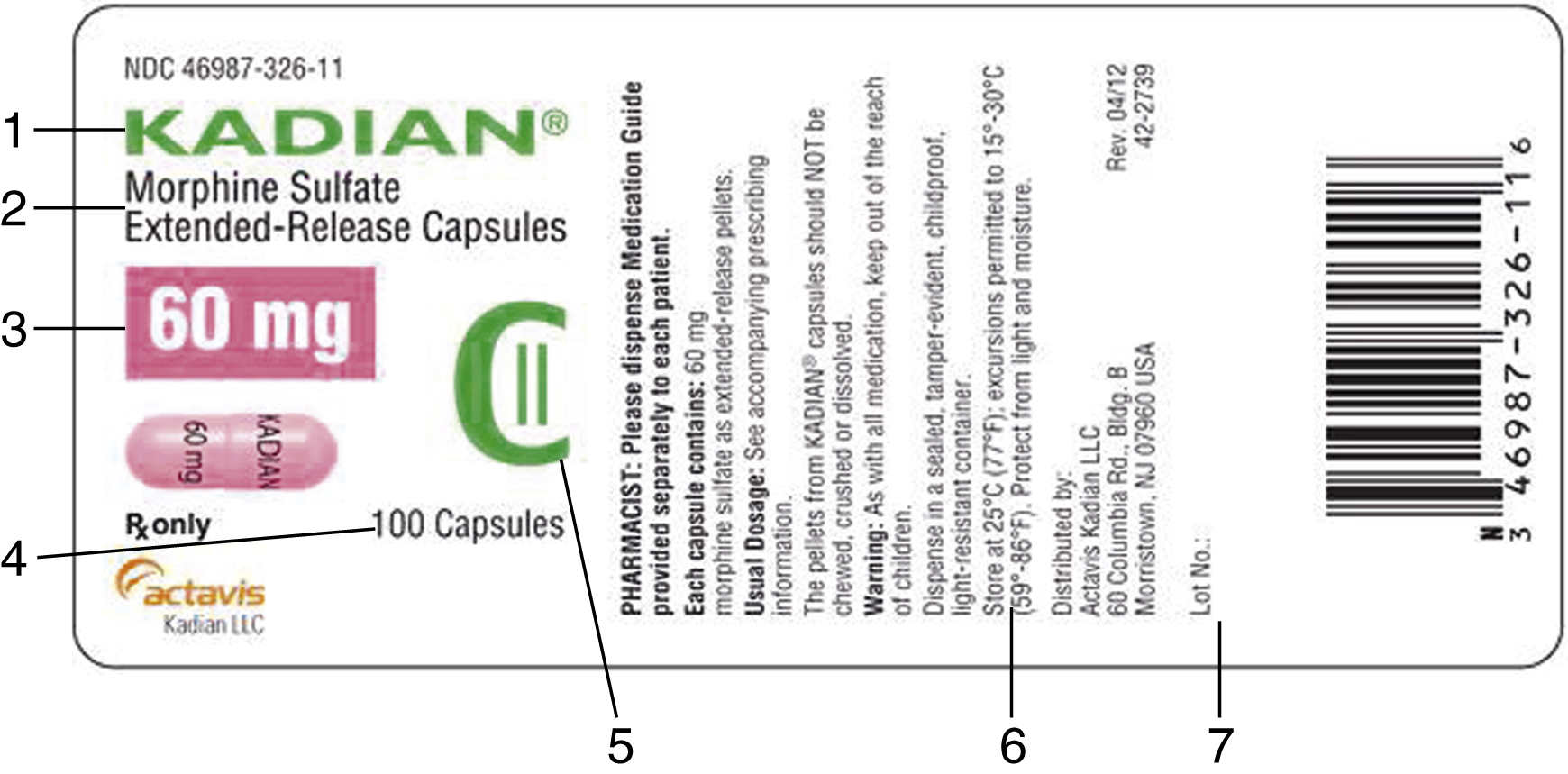
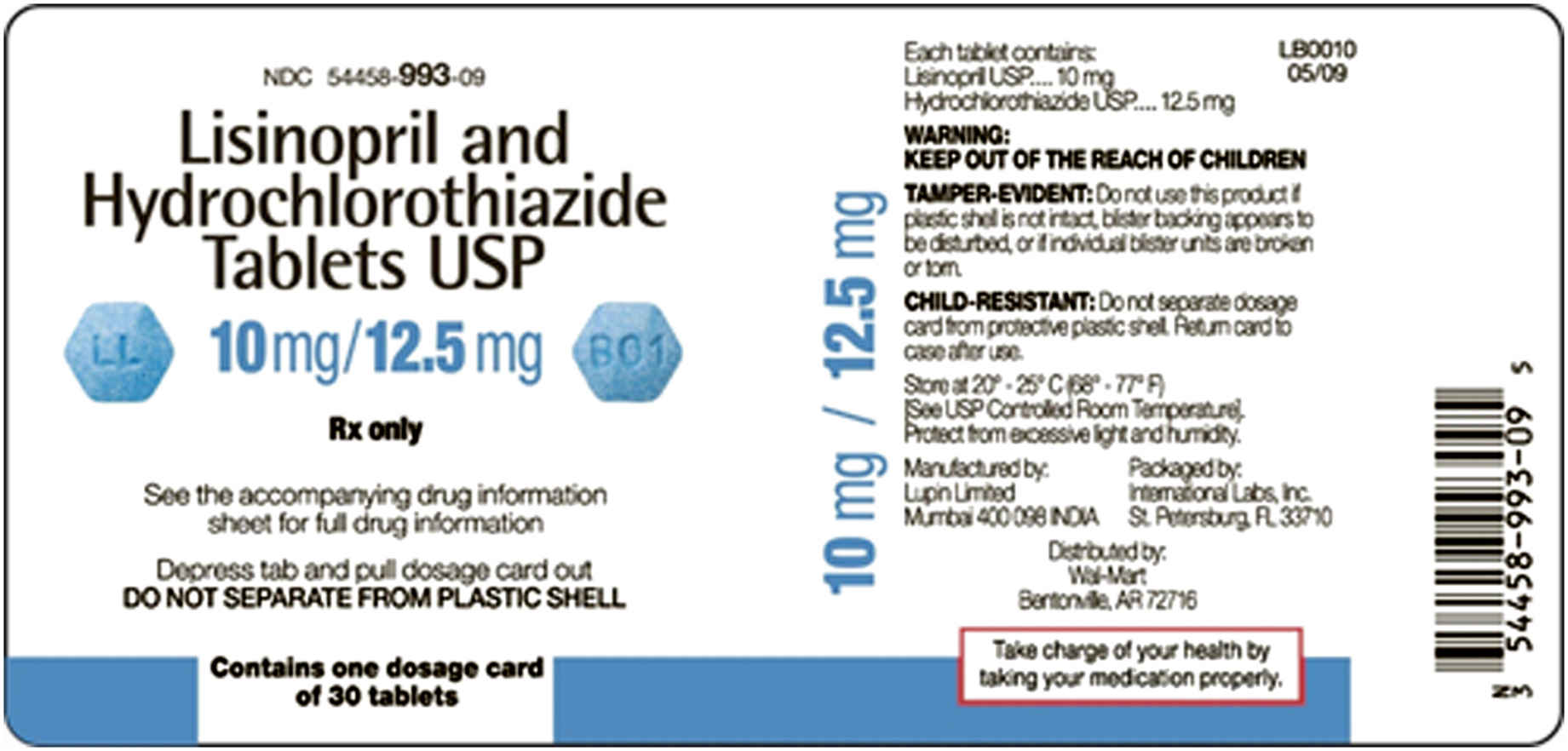
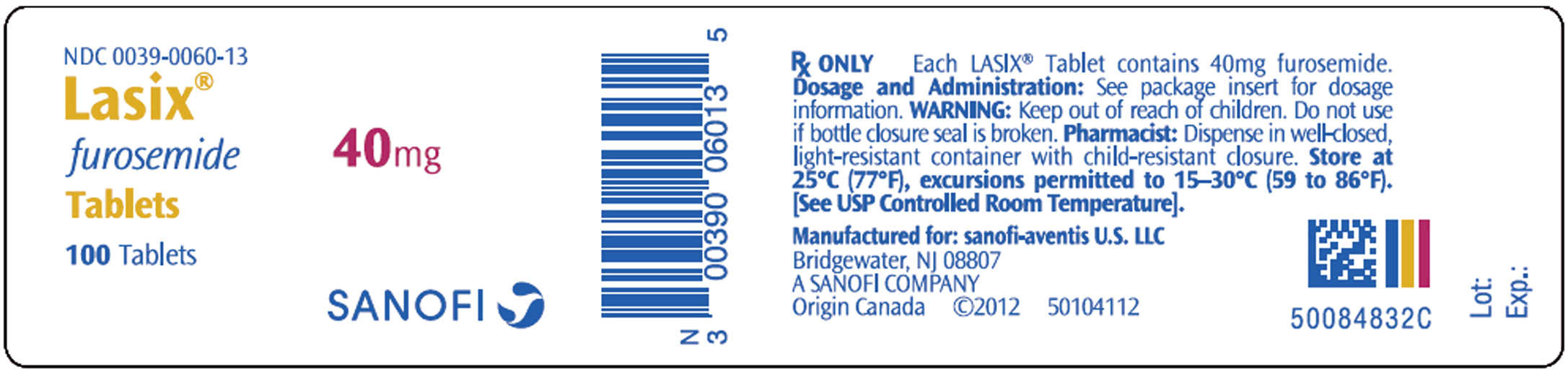
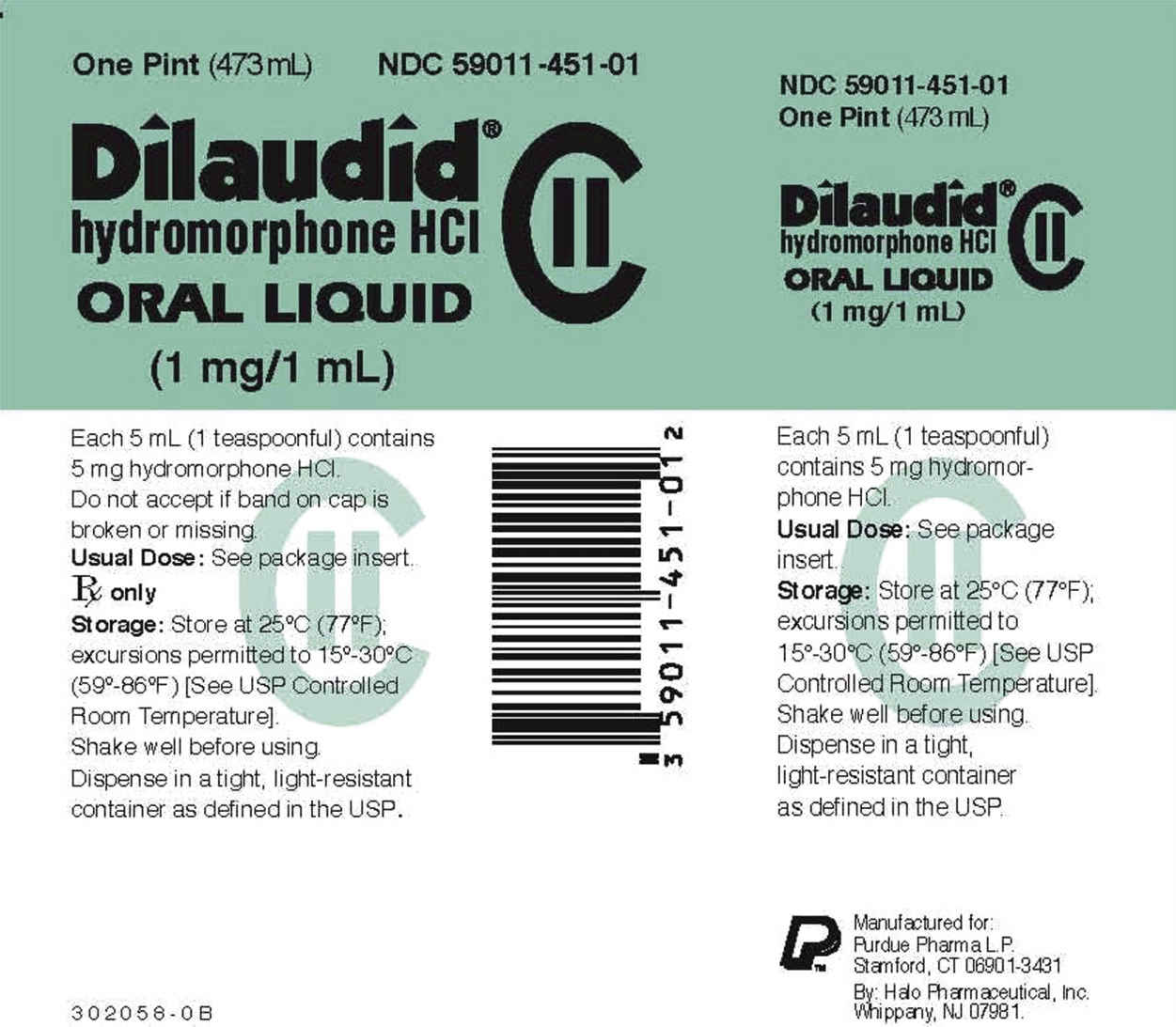
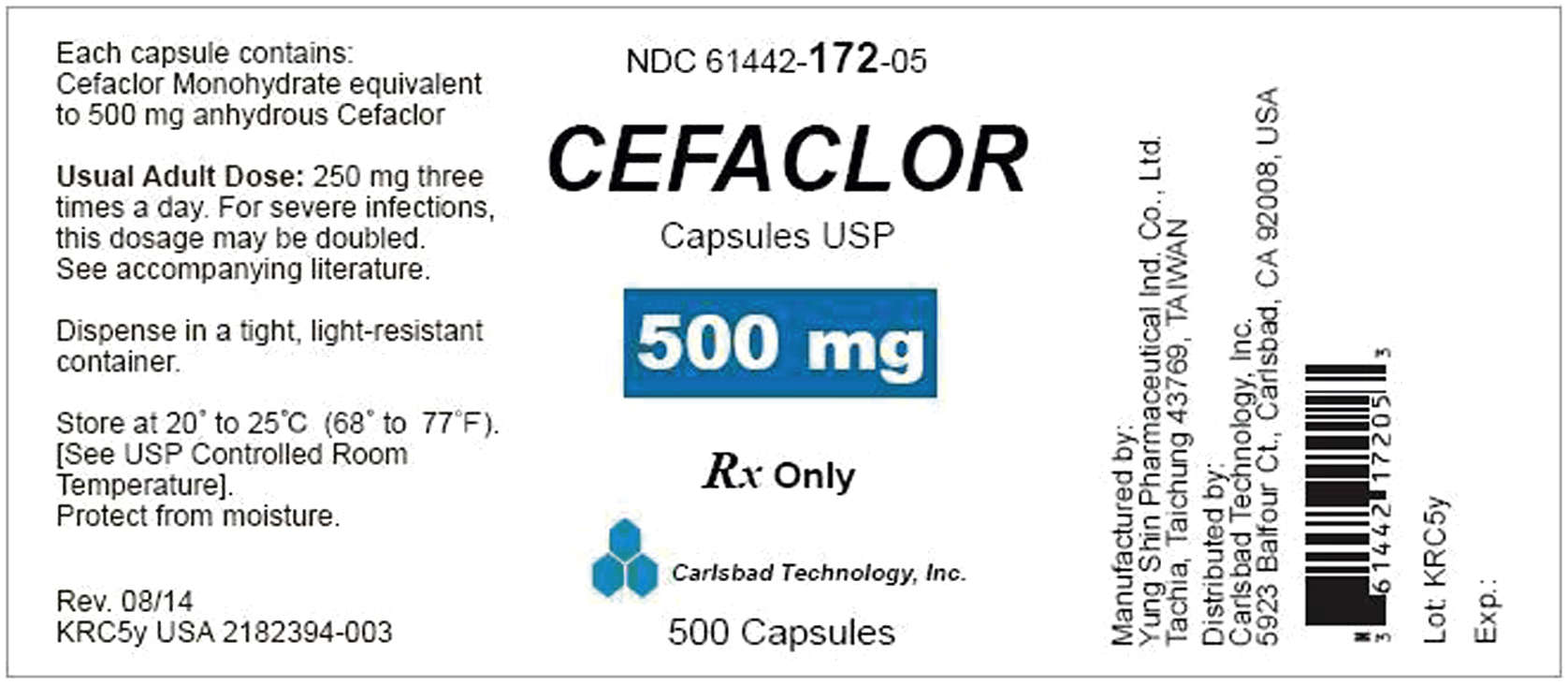
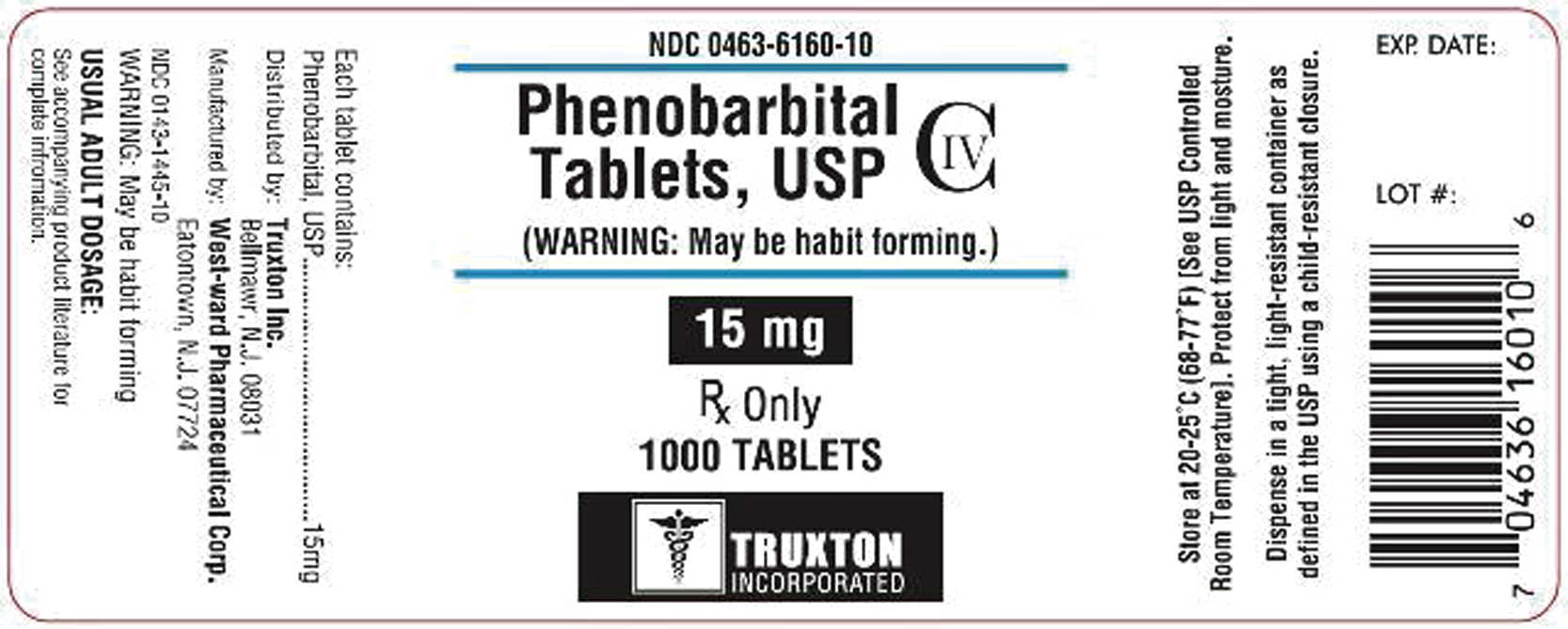
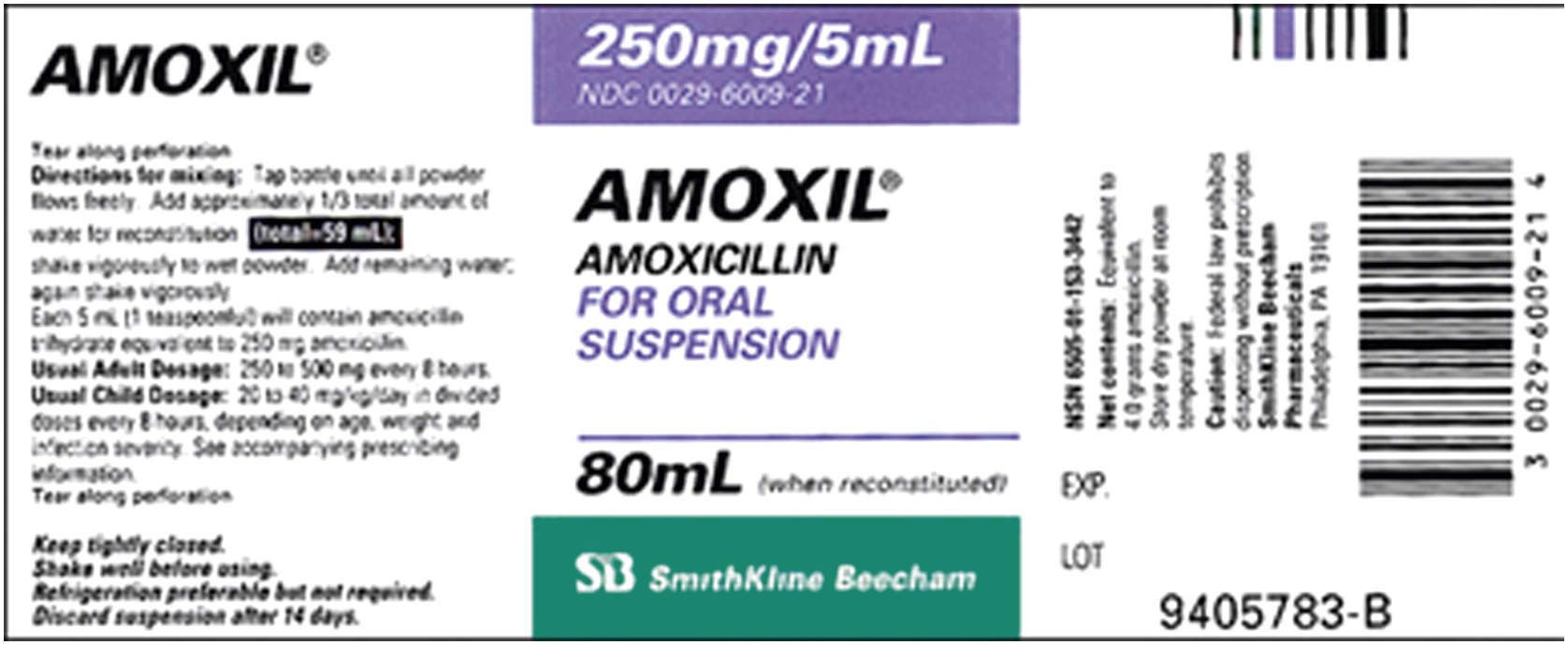
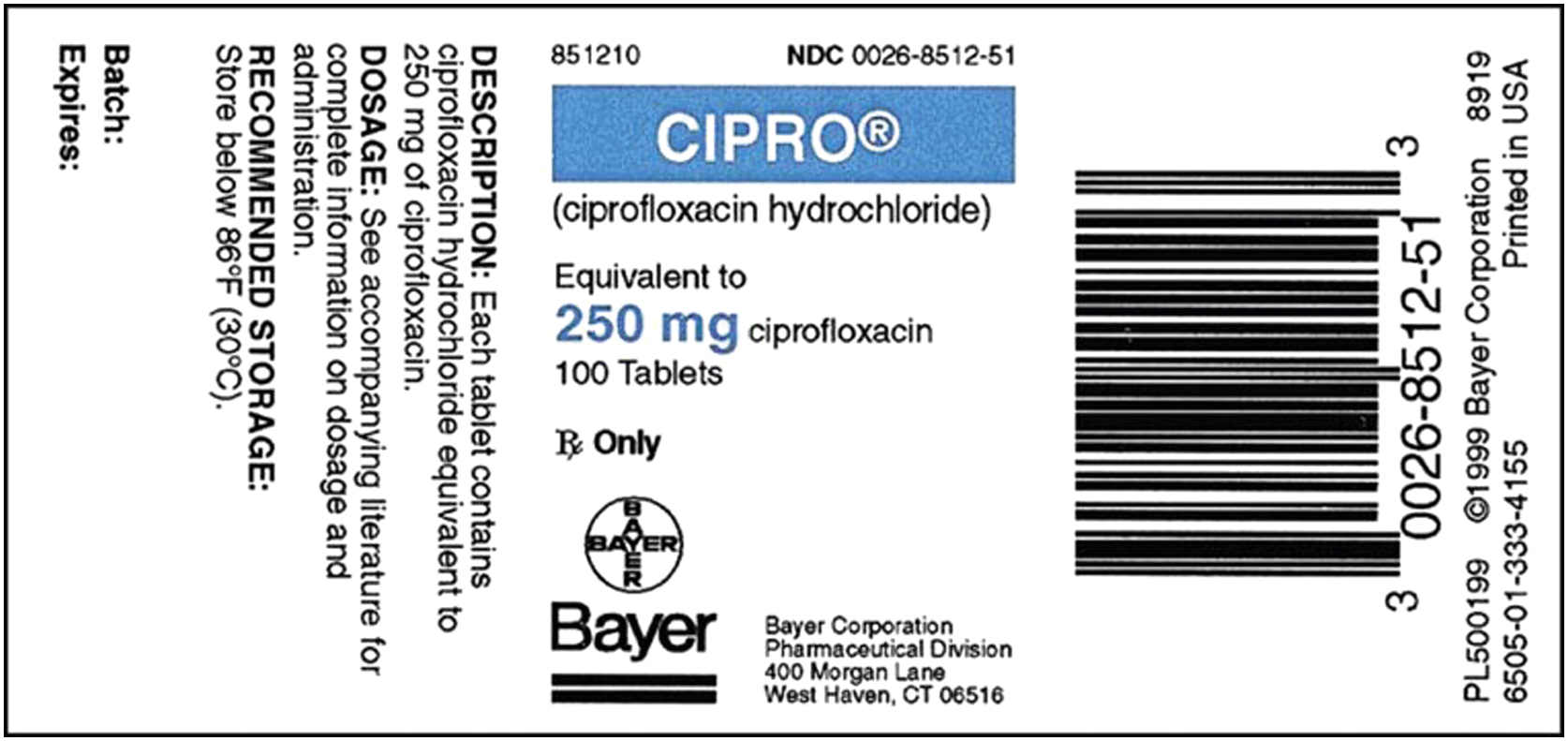
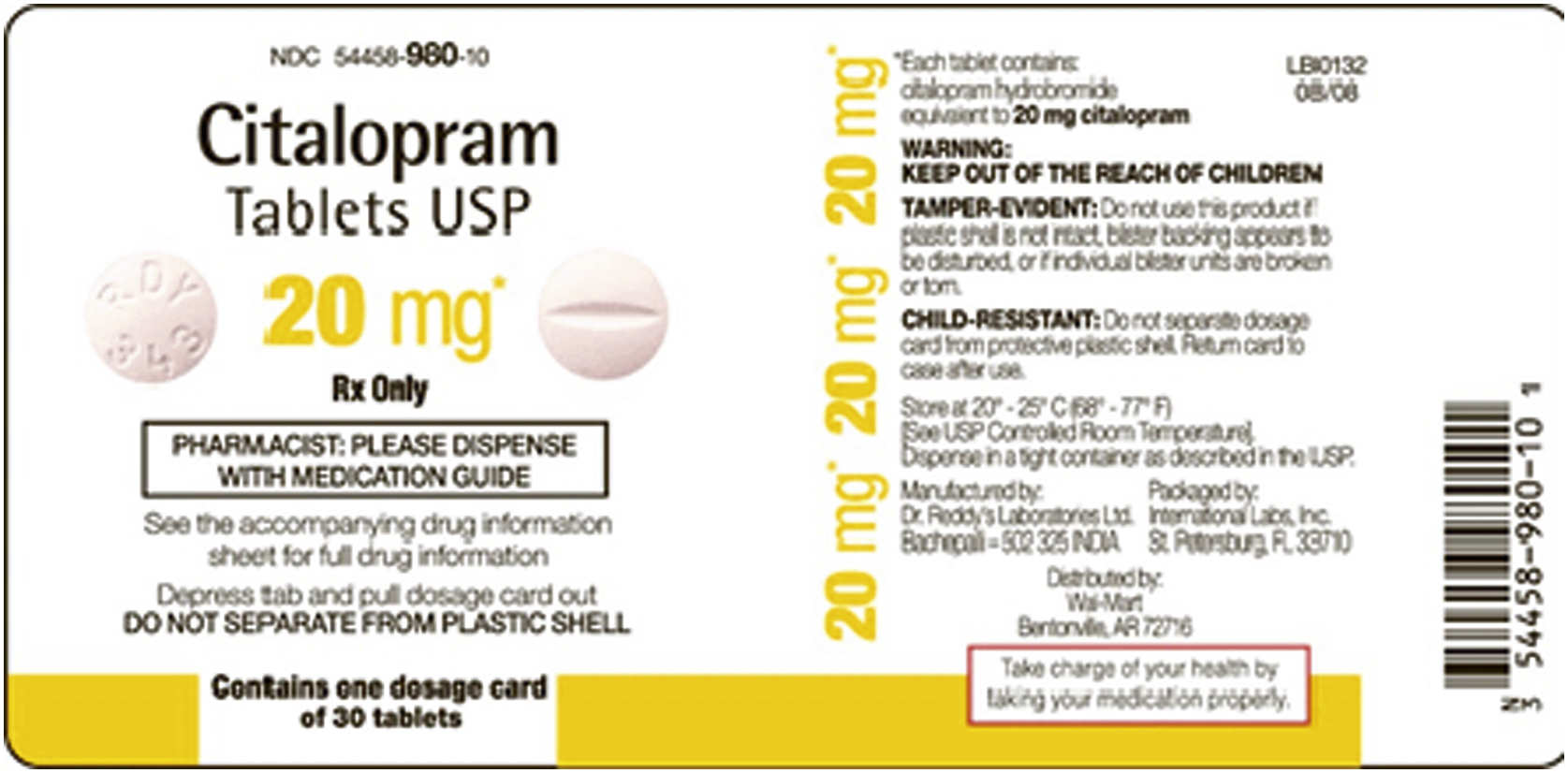
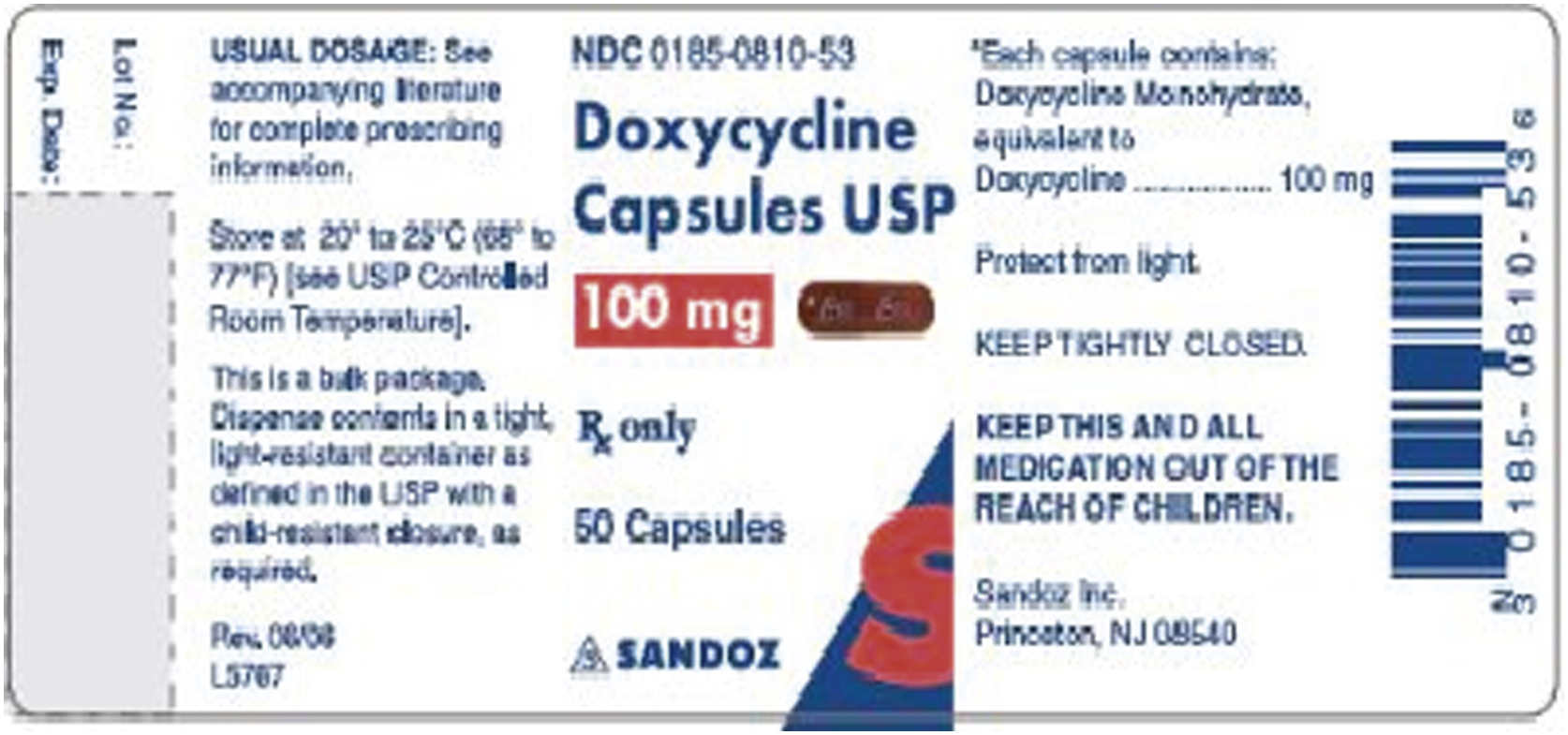
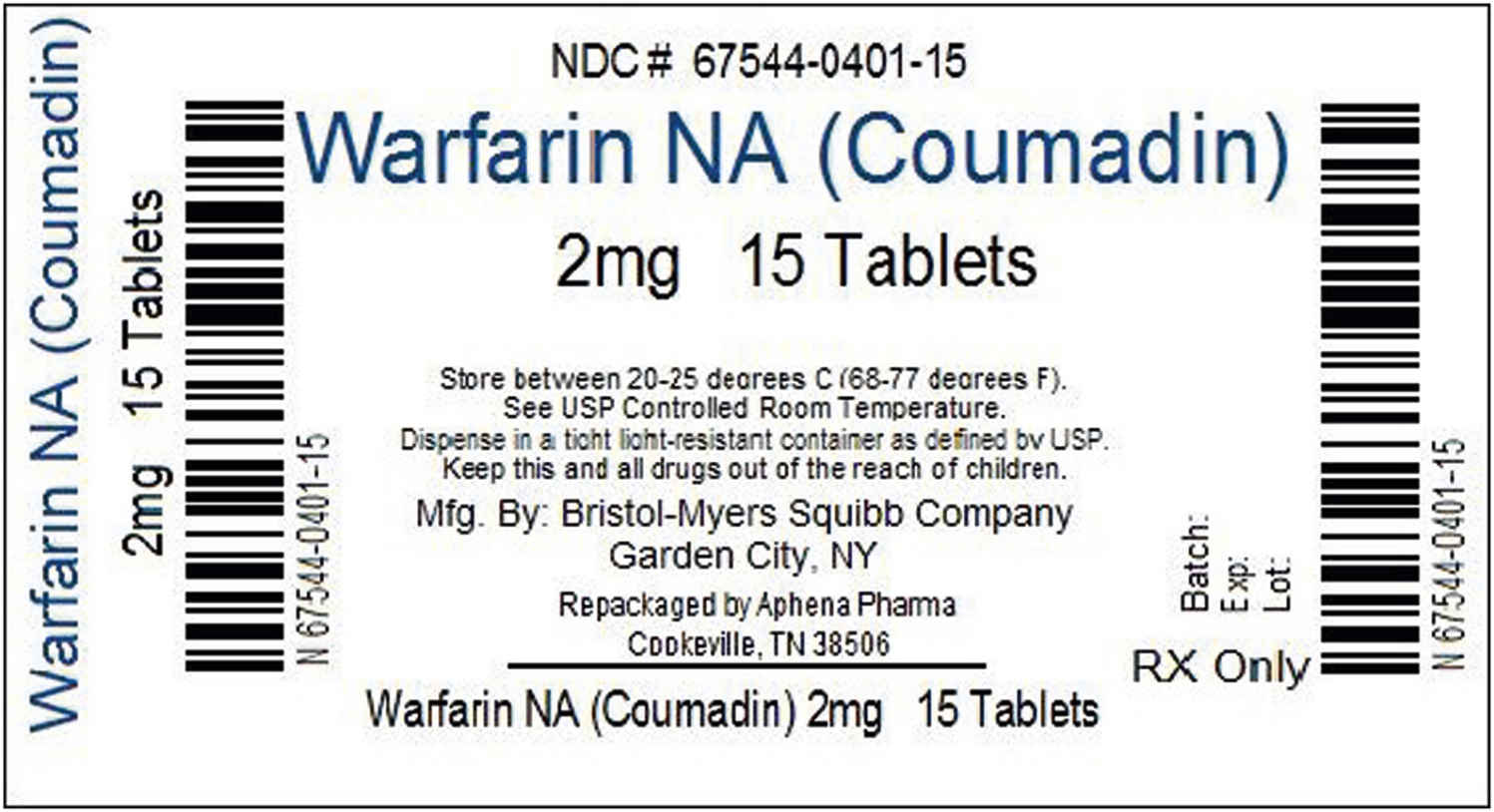
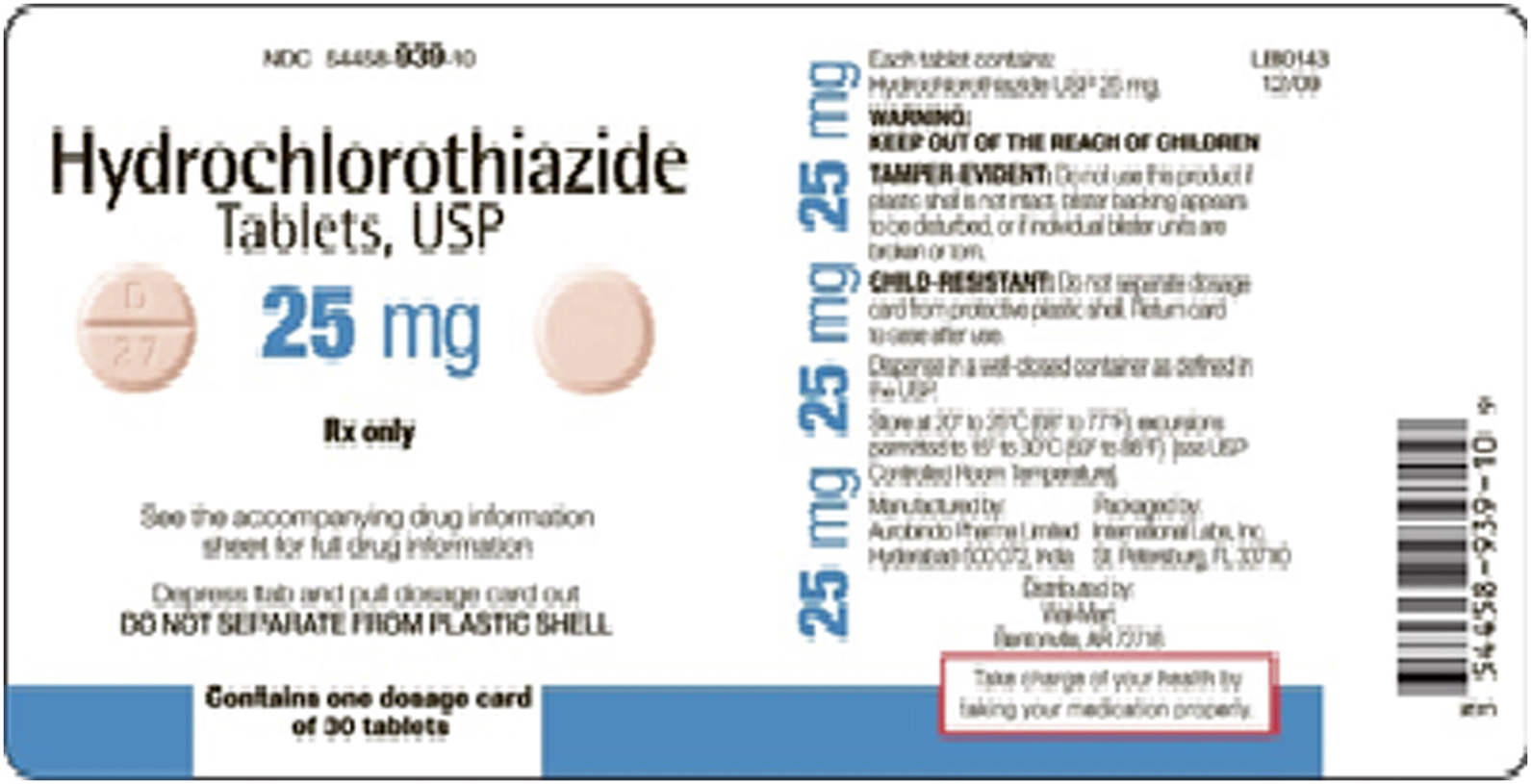
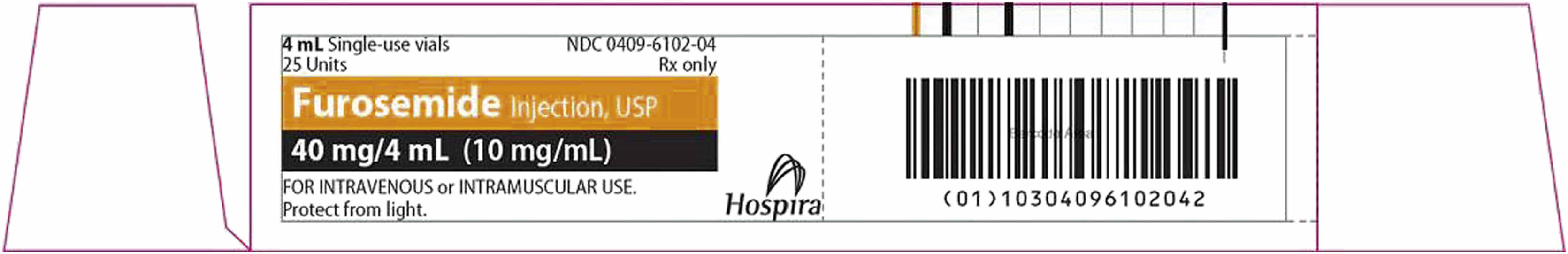
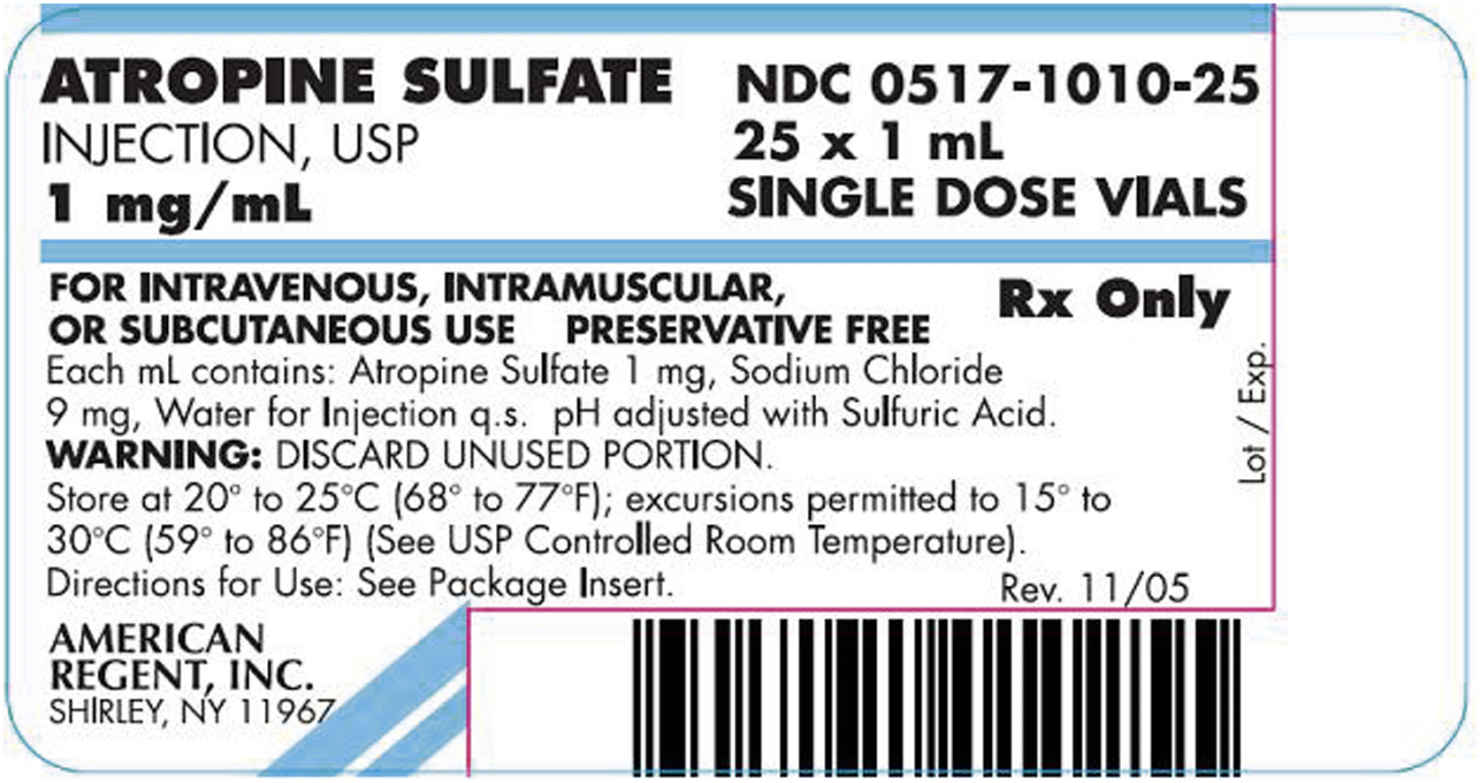
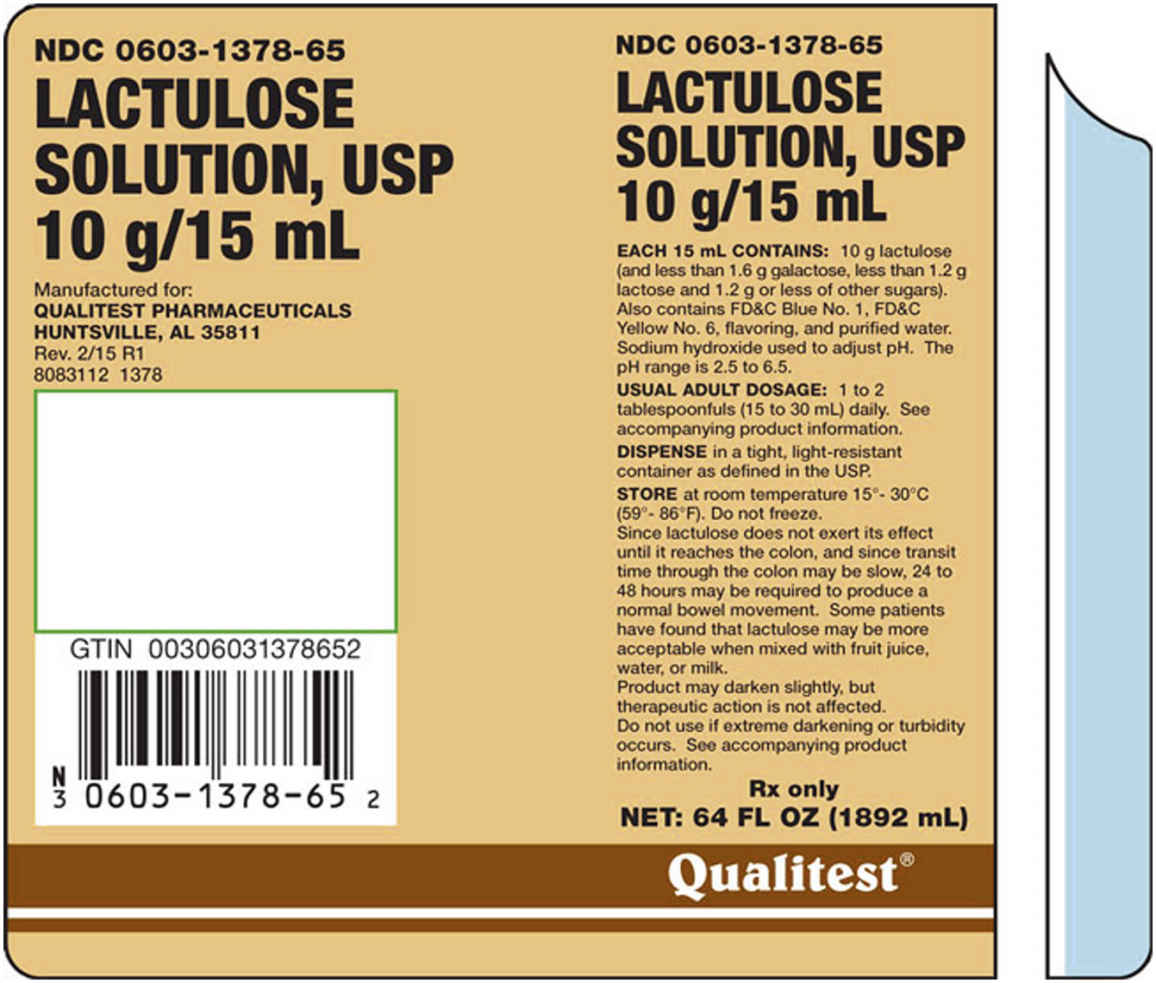
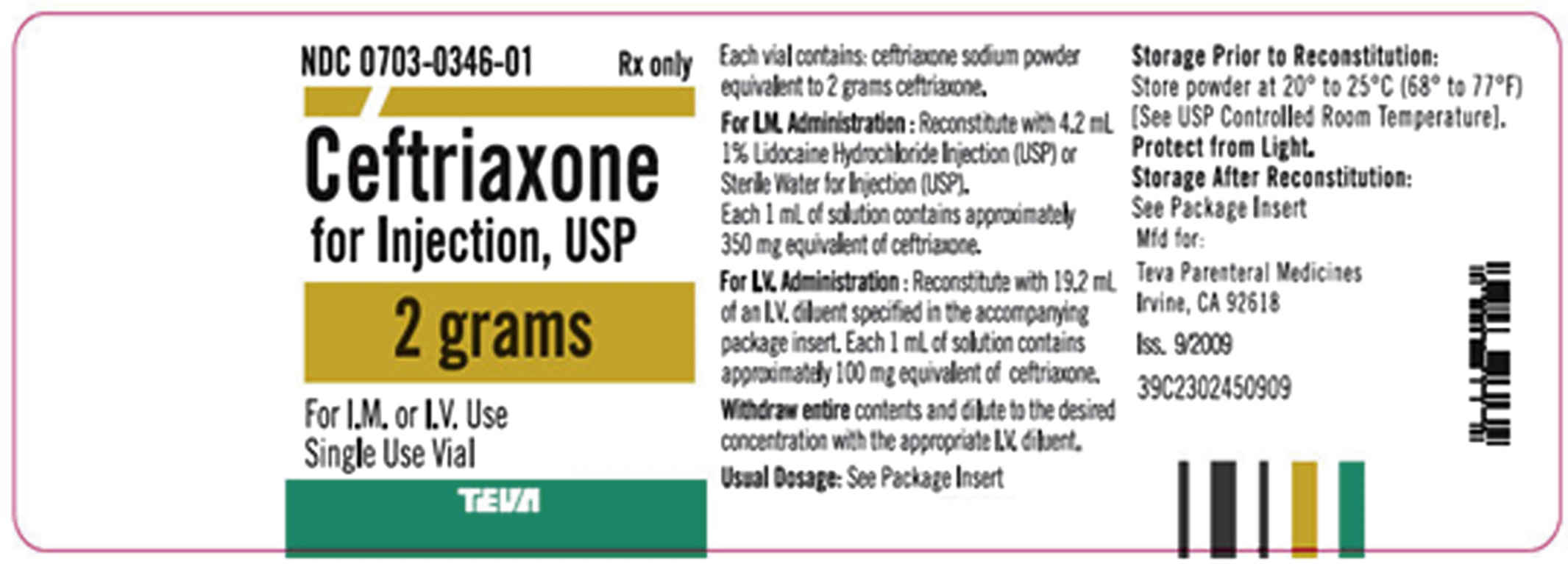
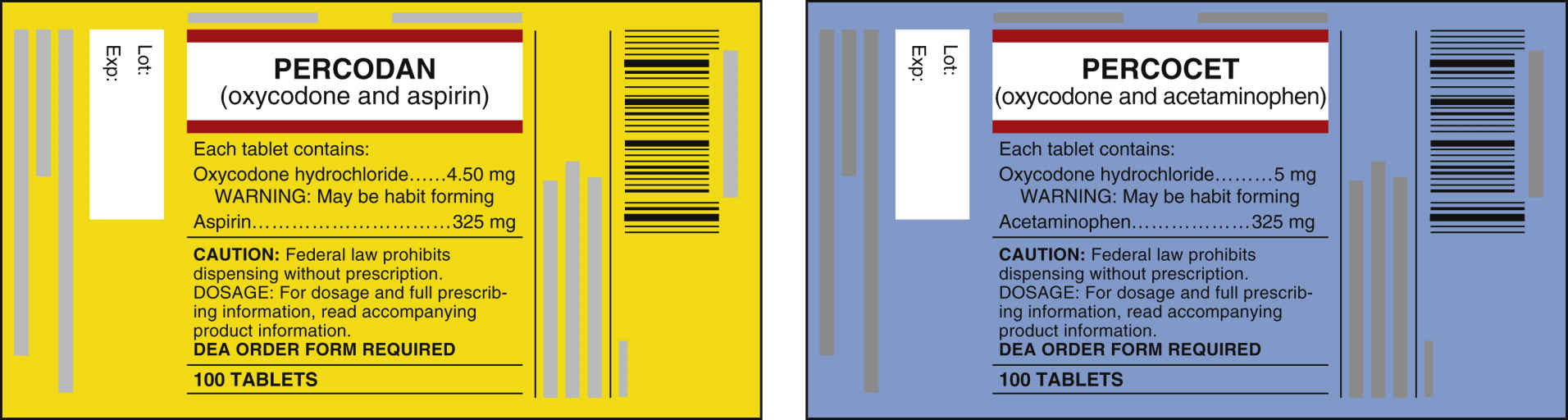
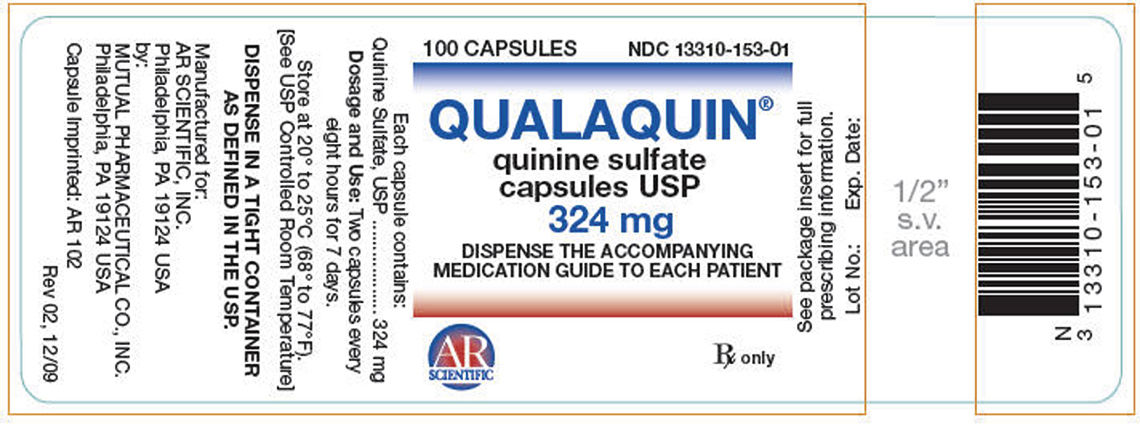
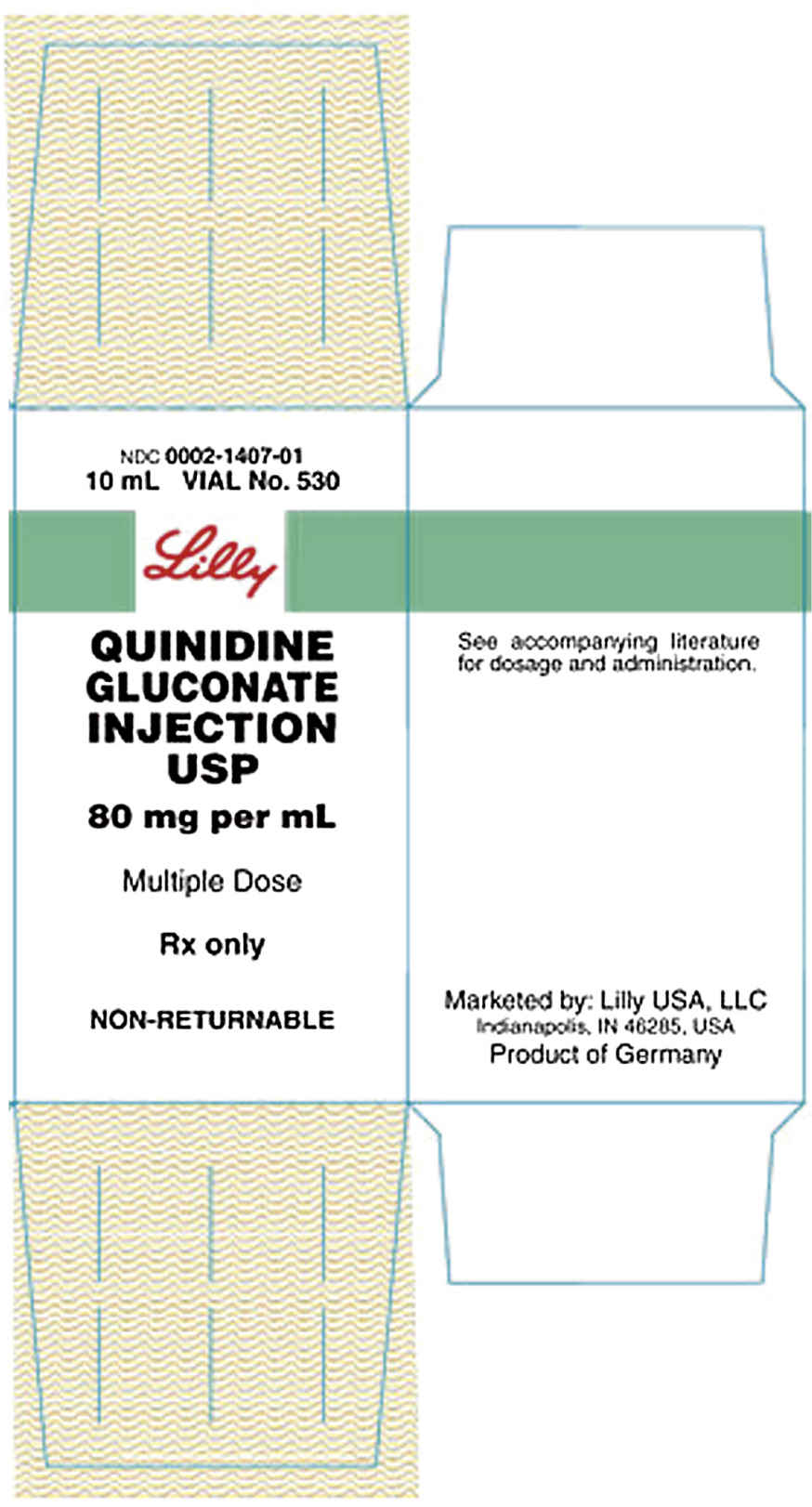
Interpreting Drug Labels
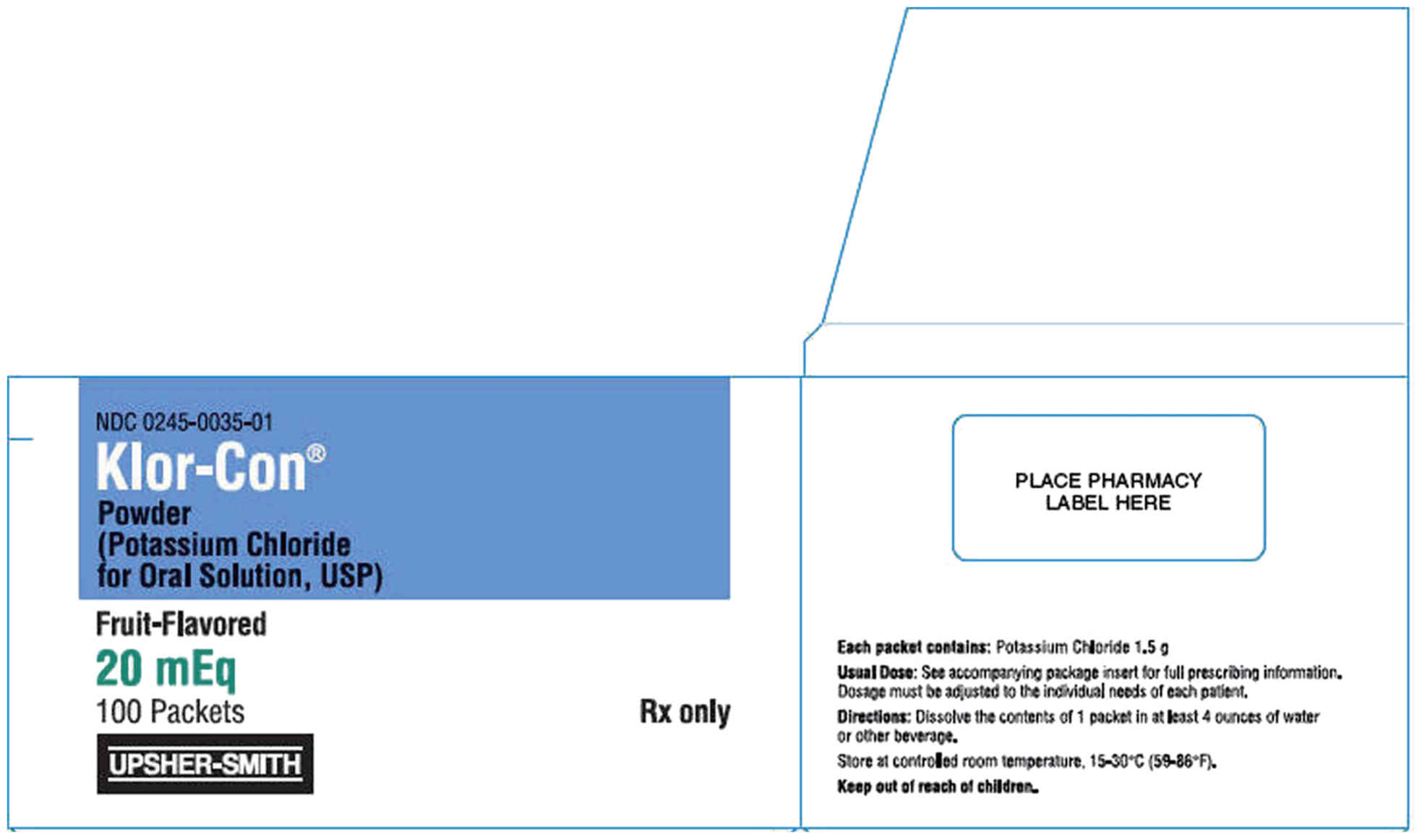
Pharmaceutical companies usually label their drugs with the brand name, also called the trade name, first in large letters with the generic name, then in smaller letters. Labels for generic drugs may have only the generic name of the drug listed. The formulation or the drug amount per tablet, capsule, or unit of liquid (for oral and parenteral doses) is printed on the drug label. Other information found on drug labels includes lot number, expiration date, proper storage of the drug, and whether it is a controlled substance. Two examples of drug labels are given below, the first for an oral drug and the second for a parenteral drug. The third example shows additional information provided on drug labels.
Precautions when Reading Drug Labels
Be aware of drug names that sound or look alike; for example, note the similarity between the trade names Percodan and Percocet. Percocet, which contains oxycodone and acetaminophen, is the preparation most commonly prescribed.
Percodan contains oxycodone and aspirin, and a patient may be allergic to aspirin or should not take aspirin because of a stomach ulcer. Acetaminophen can cause liver toxicity; in persons with normal liver function, the maximum dosage of acetaminophen is 3000 mg per 24 hours.
Note the similarity between quinine sulfate and quinidine gluconate. These drugs differ greatly. Quinine is prescribed for malaria, whereas quinidine is prescribed for cardiac arrhythmias.
To decrease medication errors, the nurse administering the drug should perform a minimum of three label checks with the patient’s medication administration record (MAR).
Methods of Drug Calculation
Generally, calculations are made for one dose. For example, if the order states that a patient is to be given 500 mg of a drug three times a day, you would calculate the amount of drug that is equivalent to 500 mg. Occasionally, nurses calculate the full daily dose, which in this case would be 1500 mg (500 mg times three doses).
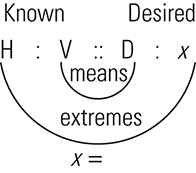
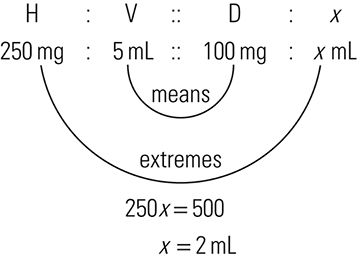
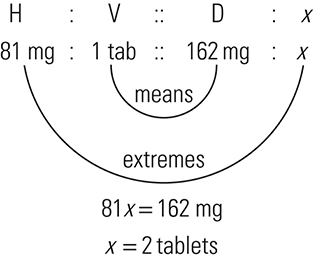
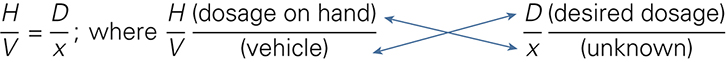
The three general methods for the calculation of drug dosages are the (1) basic formula (BF), (2) ratio and proportion/fractional equation (RP/FE), and (3) dimensional analysis (DA). These methods are used to calculate most enteral and parenteral drug dosages. The nurse should select one of the methods to calculate drug dosages and use that method consistently. All but the dimensional analysis requires using the same units of measure. It is most helpful to convert to the system used on the drug label. If the drug is ordered in grams (g, G) and the drug label gives the dose in milligrams (mg), convert grams to milligrams (the measurement on the drug label) and proceed with the drug calculation.
For drugs that require individualized dosing, calculation by body weight (BW) or by body surface area (BSA) may be necessary. These last two methods are mostly used for the calculation of pediatric dosages and for drugs used in the treatment of cancer (antineoplastic drugs). BW and BSA methods of calculation are also useful for individuals whose BW is low, who are obese, or who are older adults.
Rounding Rules
Notice when to round. Tablets and caplets can be rounded to the nearest half if they are scored (see the image for citalopram). Some tablets are scored in fourths. In this case, the dosage can be rounded to the nearest fourth. However, tablets and caplets that are extended release, sustained release, controlled release, or enteric coated should not be split because splitting or crushing these preparations destroys the properties that render the drug long lasting. For this reason, capsules are rounded to the nearest whole number. Liquid drugs can be rounded to the nearest tenth; the exception to this rule is when calculating dosages of drops, which are rounded to the nearest whole number.
When rounding, determine how many places beyond the decimal point are appropriate. The general rounding rules are:
1. If a number to the right of the digit needs to be rounded and is 4 or less, round down. For example, when rounding 1.343 to the hundredth place, the number becomes 1.34. Rounding 1.343 to the tenth place, it becomes 1.3. Rounding 1.343 to a whole number, it becomes 1.
2. If a number to the right of the digit needs to be rounded and is 5 or greater, round up. For example, when rounding 1.745 to the hundredth place, the number becomes 1.75. Rounding 1.745 to the tenth place, it becomes 1.7. Rounding 1.745 to a whole number, it becomes 2.
Calculating Dosages for Drugs Measured in Units or Milliequivalents
Some medications, such as heparin and insulin, are measured in units. Typically, units are not converted into any other measure.