DRUG CLASSES
Loop diuretics
Thiazides and related diuretics
Potassium-sparing diuretics
Osmotic diuretics
Carbonic anhydrase inhibitors
Many conditions or diseases, such as heart failure (HF), endocrine disturbances, and kidney and liver diseases, can cause fluid overload or edema (retention of excess fluid). When the patient shows signs of excess fluid retention, the primary health care provider may order a diuretic to reduce the increased fluid. A diuretic is a drug that increases the excretion of urine (i.e., water, electrolytes, and waste products) by the kidneys. There are various types of diuretic drugs, and the primary health care provider selects the one that best suits the patient’s needs and effectively reduces the amount of excess fluid in body tissues.
Hypertension is frequently treated with the administration of an antihypertensive drug and a diuretic. The diuretics used for this combination therapy include the loop diuretics and the thiazides. The specific uses of each type of diuretic drug are discussed in the following sections.
PHARMACOLOGY IN PRACTICE

You are concerned about Mrs. Moore because of the increase in calls from her out-of-town daughter. It is time to do a medication reconciliation. When she brings in a bag of pills you find that a prescription bottle for a daily diuretic filled 3 weeks ago is almost full. As you read on, see if you can determine what questions to ask Mrs. Moore.
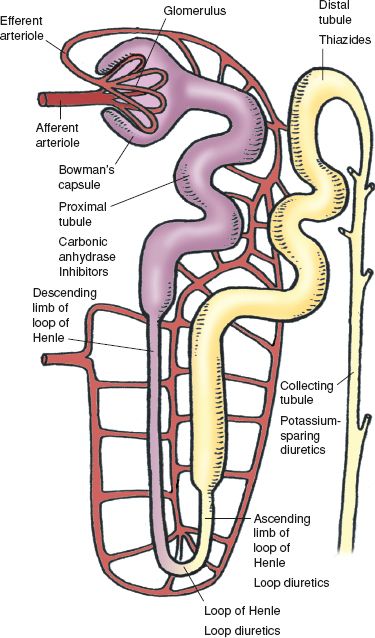
Figure 33.1 The nephron is the functional unit of the kidney. Note the various tubules, the site of most diuretic activity.
Actions
Diuretics work by altering the excretion or reabsorption of electrolytes (sodium and chloride) in the kidney. In turn, this determines the amount of water that becomes urine and is eliminated in the genitourinary system. Refer to the illustration of the kidney nephron (Fig. 33.1) for a better understanding of the actions as you read about the diuretics.
• Loop diuretics inhibit reabsorption of sodium and chloride in the distal and proximal tubules of the kidney and in the loop of Henle. Acting at three sites increases their effectiveness as diuretics.
• Thiazide and related diuretics inhibit the reabsorption of sodium and chloride ions in the ascending portion of the loop of Henle and the early distal tubule of the nephron. This action results in the excretion of sodium, chloride, and water.
Both of these types of diuretics will also cause the electrolyte potassium to be excreted in urine. If there is an issue of maintaining potassium in the body, another type of diuretic may be used.
• Potassium-sparing diuretics (or potassium saving) reduce the excretion of potassium from the kidney. Potassium-sparing diuretics work by blocking the reabsorption of sodium in the kidney tubules, thereby increasing sodium and water in the urine; this reduces the excretion of potassium. Spironolactone (Aldactone) works to antagonize the action of aldosterone. Aldosterone, a hormone produced by the adrenal cortex, enhances the reabsorption of sodium in the distal convoluted tubules of the kidney. When this is blocked by the drug, sodium (but not potassium) and water are excreted.
• Osmotic diuretics increase the density of the filtrate in the glomerulus. This prevents selective reabsorption of water, and it passes out as urine. Sodium and chloride excretion is also increased.
• Carbonic anhydrase inhibitors are sulfonamides, without bacteriostatic action, that inhibit the enzyme carbonic anhydrase. Carbonic anhydrase inhibition results in the excretion of sodium, potassium, bicarbonate, and water.
Uses
Diuretic drugs are used in the treatment of the following:
• Edema (fluid retention) associated with HF, corticosteroid/estrogen therapy, and cirrhosis of the liver
• Hypertension
• Renal disease (acute failure, renal insufficiency, and nephrotic syndrome)
• Cerebral edema
• Acute glaucoma (topically) and increased intraocular pressure (IOP; before and after eye surgery)
• Seizures and altitude sickness
Ethacrynic acid (a loop diuretic) is also used for the short-term management of ascites caused by a malignancy, idiopathic edema, or lymphedema. When patients are at risk for potassium loss, the potassium-sparing diuretics may be used with or in place of other categories of diuretics.
Adverse Reactions
Adverse reactions associated with any category of diuretics involve various body systems.
Neuromuscular System Reactions
• Dizziness, lightheadedness, headache
• Weakness, fatigue
Cardiovascular System Reactions
• Orthostatic hypotension
• Electrolyte imbalances, glycosuria
Gastrointestinal System Reactions
• Anorexia
• Nausea, vomiting
Other System Reactions
Dermatologic reactions include rash and photosensitivity. Extremity paresthesias (numbness or tingling) or flaccid muscles may indicate hypokalemia (low blood potassium). Hyperkalemia (an increase in potassium in the blood), a serious event, may occur with the administration of potassium-sparing diuretics. Hyperkalemia is most likely to occur in patients with an inadequate fluid intake and urine output, those with diabetes or renal disease, older adults, and those who are severely ill.
In male patients taking spironolactone, gynecomastia (breast enlargement) may occur. This reaction appears to be related to both dosage and duration of therapy. The gynecomastia is usually reversible when therapy is discontinued, but in rare instances some breast enlargement may remain.
Additional adverse reactions of these drugs are listed in the Summary Drug Table: Diuretics. When a potassium-sparing diuretic and another diuretic are given together, the adverse reactions associated with both drugs may be greater.
Contraindications
Diuretics are contraindicated in patients with known hypersensitivity to the drugs, electrolyte imbalances, severe kidney or liver dysfunction, and anuria (cessation of urine production). Mannitol (an osmotic diuretic) is contraindicated in patients with active intracranial bleeding (except during craniotomy). The potassium-sparing diuretics are contraindicated in patients with hyperkalemia and are not recommended for pediatric patients.
Precautions
Diuretics are used cautiously in patients with renal dysfunction. Most of the diuretics are pregnancy category C drugs (although ethacrynic acid, torsemide, isosorbide, amiloride, and triamterene are in pregnancy category B) and must be used cautiously during pregnancy and lactation. All of the thiazide diuretics are pregnancy category B drugs, with the exception of benzthiazide and methyclothiazide, which are pregnancy category C drugs. The safety of these drugs for use during pregnancy and lactation has not been established, so they should be used only when the drug is clearly needed and when the potential benefits to the patient outweigh the potential hazards to the fetus.
The thiazide and loop diuretics are used cautiously in patients with liver disease, diabetes, systemic lupus erythematosus (may exacerbate or activate the disease), or diarrhea. A cross-sensitivity reaction may occur with the thiazides and sulfonamides. Some of the thiazide diuretics contain tartrazine (a yellow food dye), which may cause allergic-type reactions or bronchial asthma in individuals sensitive to tartrazine. Patients with sensitivity to sulfonamides may show allergic reactions to loop diuretics (furosemide, torsemide, or bumetanide). The potassium-sparing diuretics should be used cautiously in patients with liver disease, diabetes, or gout.
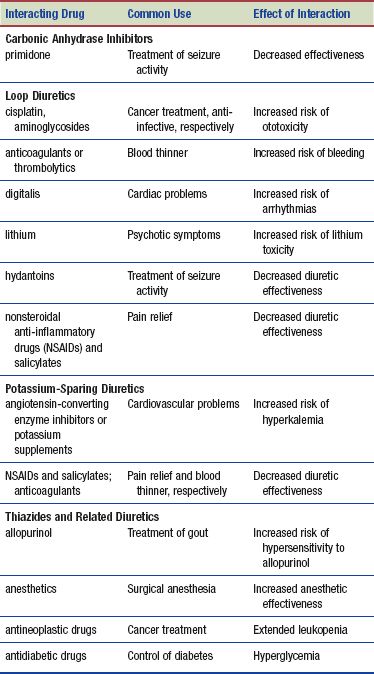
Interactions
All the diuretics may cause an increased risk of hypotension when taken with antihypertensive drugs. The interactions for specific diuretic categories are listed here.
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Numerous herbal diuretics are available as over-the-counter (OTC) products. Most plant and herbal extracts available as OTC diuretics are nontoxic. The following herbals are believed to possess diuretic activity: celery, chicory, sassafras, juniper berries, St. John’s wort, foxglove, horsetail, licorice, dandelion, digitalis purpurea, ephedra, hibiscus, parsley, and elderberry. However, most are either ineffective or no more effective than caffeine. There is very little scientific evidence to justify the use of these plants as diuretics. For example, dandelion root was once believed to be a strong diuretic. However, research has found dandelion root to be safe but ineffective as a diuretic. No herbal diuretic should be taken without discussing with your primary health care provider. Diuretic teas such as juniper berries and shave grass or horsetail are contraindicated. Juniper berries have been associated with renal damage, and horsetail contains severely toxic compounds. Teas with ephedrine should be avoided, especially by individuals with hypertension (DerMarderosian, 2003).
NURSING PROCESS
PATIENT RECEIVING AN UPPER RESPIRATORY SYSTEM DRUG
ASSESSMENT
Preadministration Assessment
Before administering a diuretic, taking vital signs and measuring weight gives you baseline information to compare fluid loss. Laboratory results such as serum electrolytes are carefully reviewed. Patients with renal dysfunction should have blood urea nitrogen (BUN) and creatinine clearance levels monitored as well. If the patient has peripheral edema, inspect and measure the involved areas and document in the patient’s chart the degree and extent of edema.
If the patient is to receive an osmotic diuretic, the focus of the assessment is on the patient’s disease or disorder and the symptoms being treated. For example, if the patient has a low urinary output and the osmotic diuretic is given to increase urinary output, review the ratio between intake and output, and symptoms that the patient is experiencing.
Ongoing Assessment
The type of assessment depends on such factors as the reason for the administration of the diuretic, the type of diuretic administered, the route of administration, and the condition of the patient. When the patient is institutionalized, measure and record fluid intake and output and report to the primary health care provider any marked decrease in the output. Report fluid loss as measured by weighing the patient at the same time daily, making certain that the patient is wearing the same amount or type of clothing. Depending on the specific diuretic, frequent serum electrolyte, uric acid, and liver and kidney function tests may be performed during the first few months of therapy and periodically thereafter. When patients take diuretics on an outpatient basis, it is your responsibility to instruct patients or caregivers to do the same activities at home.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Impaired Urinary Elimination related to action of the diuretics causing increased frequency
Impaired Urinary Elimination related to action of the diuretics causing increased frequency
 Risk for Deficient Fluid Volume related to excessive diuresis secondary to administration of a diuretic
Risk for Deficient Fluid Volume related to excessive diuresis secondary to administration of a diuretic
 Risk for Injury related to lightheadedness, dizziness, or cardiac arrhythmias
Risk for Injury related to lightheadedness, dizziness, or cardiac arrhythmias
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient depend on the reason for administration of the diuretic but may include an optimal response to drug therapy, support of patient needs related to adverse drug reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
Diuretics are used to treat many different types of conditions. Therefore, promoting an optimal response to therapy for patients taking diuretics often depends on the specific diuretic and the patient’s condition.
PATIENT WITH EDEMA. Patients with edema caused by HF or other causes are weighed daily or as ordered by the primary health care provider. Weight loss of about 2 lb daily is desirable to maintain fluid loss and prevent dehydration and electrolyte imbalances. Every 8 hours carefully measure and document the fluid intake and output. The critically ill patient or the patient with renal disease may require more frequent measurements of urinary output. The blood pressure, pulse, and respiratory rate are assessed every 4 hours or as ordered by the primary health care provider. An acutely ill patient may require more frequent monitoring of the vital signs.
Areas of edema are examined daily to evaluate the effectiveness of drug therapy. Note the patient’s general appearance and condition daily or more often if the patient is acutely ill.
PATIENT WITH HYPERTENSION. Teach the hypertensive patient how to monitor the blood pressure and pulse rate when receiving a diuretic or a diuretic along with an antihypertensive drug. Vital signs, including respiratory rate, are more frequently monitored when the patient is critically ill or the blood pressure excessively high.
PATIENT WITH INCREASED INTRACRANIAL PRESSURE. Mannitol is administered only by the intravenous (IV) route. Because mannitol solution may crystallize when exposed to low temperatures, inspect the solution before administration. If this happens, return the solution to the pharmacy and request another dose. The rate of administration and concentration of the drug is individualized to maintain a urine flow of at least 30 to 50 mL/hour.
When a patient is receiving the osmotic diuretic mannitol or urea for treatment of increased intracranial pressure caused by cerebral edema, perform neurologic assessments (response of the pupils to light, level of consciousness, or response to a painful stimulus) in addition to vital signs at the time intervals ordered by the primary health care provider.
PATIENT WITH RENAL COMPROMISE. When thiazide diuretics are administered, renal function should be monitored periodically. These drugs may cause azotemia (accumulation of nitrogenous waste in the blood). If nonprotein nitrogen (NPN) or BUN increases, the primary health care provider may consider withholding the drug or discontinuing its use. In addition, serum uric acid concentrations are monitored periodically during treatment with thiazide diuretics, because these drugs may cause an acute attack of gout; therefore, be alert to patient complaints of joint pain or discomfort. Insulin or oral antidiabetic drug dosages may require alterations due to hyperglycemia; therefore, serum glucose concentrations are monitored periodically.
PATIENT AT RISK FOR ELECTROLYTE IMBALANCES. As fluids and electrolytes shift in the body, be alert for imbalances. Signs and symptoms of common imbalances are listed in Display 33.1. One of the primary imbalances to monitor is potassium. Patients who experience cardiac arrhythmias or who are being “digitalized” (initiating digoxin therapy) may be more susceptible to significant potassium loss when taking diuretics. The potassium-sparing diuretics are recommended for these patients.
Display 33.1 Signs and Symptoms of Common Fluid and Electrolyte Imbalances Associated With Diuretic Therapy
Dehydration (Excessive Water Loss)
• Thirst
• Poor skin turgor
• Dry mucous membranes
• Weakness
• Dizziness
• Fever
• Low urine output
Hyponatremia (Excessive Loss of Sodium)
Note: Sodium—normal laboratory values 132–145 mEq/L
• Cold, clammy skin
• Decreased skin turgor
• Confusion
• Hypotension
• Irritability
• Tachycardia
Hypomagnesemia (Low Levels of Magnesium)
Note: Magnesium—normal laboratory values 1.5–2.5 mEq/L or 1.8–3 mg/dL
• Leg and foot cramps
• Hypertension
• Tachycardia
• Neuromuscular irritability
• Tremor
• Hyperactive deep tendon reflexes
• Confusion
• Visual or auditory hallucinations
• Paresthesias
Hypokalemia (Low Blood Potassium)
Note: Potassium—normal laboratory values 3.5–5 mEq/L
• Anorexia
• Nausea
• Vomiting
• Depression
• Confusion
• Cardiac arrhythmias
• Impaired thought processes
• Drowsiness
Hyperkalemia (High Blood Potassium)
• Irritability
• Anxiety
• Confusion
• Nausea
• Diarrhea
• Cardiac arrhythmias
• Abdominal distress
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree