Chapter 37 See Chapter 70, Immunizations and Biologicals, for discussion of the immune system.
Disease-Modifying Antirheumatic Medications and Immune Modulators
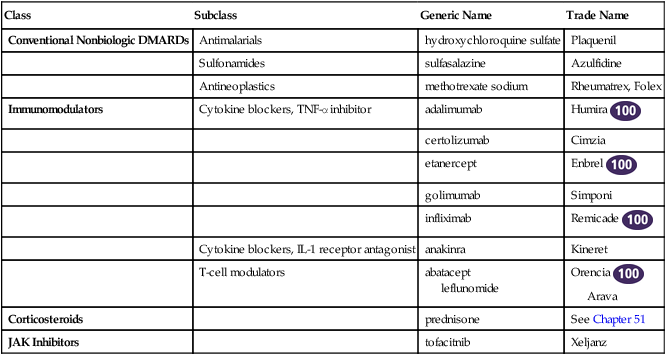
Class
Subclass
Generic Name
Trade Name
Conventional Nonbiologic DMARDs
Antimalarials
hydroxychloroquine sulfate
Plaquenil
Sulfonamides
sulfasalazine
Azulfidine
Antineoplastics
methotrexate sodium
Rheumatrex, Folex
Immunomodulators
Cytokine blockers, TNF-α inhibitor
adalimumab
Humira ![]()
certolizumab
Cimzia
etanercept
Enbrel ![]()
golimumab
Simponi
infliximab
Remicade ![]()
Cytokine blockers, IL-1 receptor antagonist
anakinra
Kineret
T-cell modulators
abatacept
leflunomide
Orencia ![]()
Arava
Corticosteroids
prednisone
See Chapter 51
JAK Inhibitors
tofacitnib
Xeljanz
Therapeutic Overview
Anatomy and Physiology
Mechanism of Action
Conventional DMARDs
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree