27 Disaster Epidemiology and Surveillance
I Overview
Disaster epidemiology and surveillance are rooted in epidemiologic principles that apply to other diseases, but unique challenges and concerns need to be considered in the context of disaster epidemiology. Investigators use disaster epidemiology to assess the short-term and long-term health effects of disasters. In addition, disaster epidemiology is important in allowing epidemiologists to understand how to prevent deaths, injuries, and disease spread in disaster situations. Despite advances in disaster epidemiology, however, there is still a need to refine the approaches to surveillance and epidemiology in disaster situations, as Noji1 stated in 1992.
A Burden of Disaster
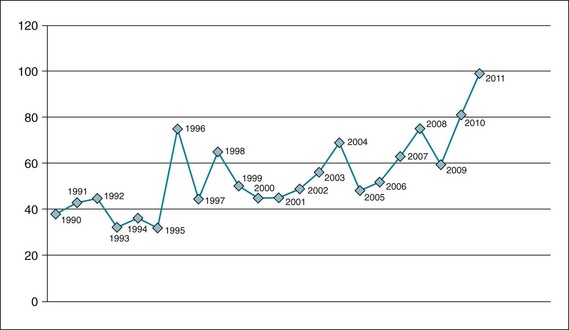
The World Health Organization (WHO) reports that 385 natural disasters killed more than 297,000 people in 2010. An additional 217 million people were affected by the disasters, at a cost equivalent to $123.9 billion in economic damages.2 In the United States, there has been a steady increase in the number of official disaster “declarations” from 1990 to 2011, with 100 declarations in 2011 (Fig. 27-1).
II Definitions and Objectives
The main objectives of disaster epidemiology are as follows:
 Prevent or reduce the number of deaths, illnesses, and injuries caused by disasters.
Prevent or reduce the number of deaths, illnesses, and injuries caused by disasters.
 Provide timely and accurate health information for decision makers.
Provide timely and accurate health information for decision makers.
 Improve prevention and mitigation strategies for future disasters by collecting information for future response preparation.
Improve prevention and mitigation strategies for future disasters by collecting information for future response preparation.
As with other types of epidemiology, disaster epidemiology focuses on identifying disease and injury patterns and risk factors to the population and community affected by the disaster. This information serves as the basis for developing prevention and mitigation strategies that are driven by three contexts of disasters: time, place, and person. For example, hurricane season on the U.S. East Coast, as well as in the Caribbean, is June 1 through November 30.3 In addition, the geographic area generally at risk is defined. Although people who live on or near the coast are at increased risk of injury or death during a hurricane, evacuation from the hurricane zone minimizes or eliminates this risk. In contrast, the usual season for flu occurrence is over the winter months in the United States, and flu risk is related to exposure, immunization status, and other factors such as age; generally, elderly and very young populations, people with chronic illness or immunocompromise, and pregnant women are at increased risks for complications and mortality, depending on the flu strain that is active in a given year.4 Prevention strategies would focus on immunization of highest-risk populations, and depending on the severity of an outbreak, isolation of people who have contracted flu or who have been exposed and are likely to expose others to risk.
A Descriptive Epidemiology
After the World Trade Center disaster on 9/11, responders to the scene were exposed to various types of particulate matter, as well as larger pieces of debris, some of which fell from the collapsing towers. Other responders have complained of resulting respiratory problems. The epidemiology of the health aftermath of the disaster continues to emerge; longitudinal surveys are providing information on various health outcomes. A study of 2960 disaster workers found that 70% did not meet criteria for posttraumatic stress disorder (PTSD), but at 6 years after the event, 4.2% of nonrescue disaster workers still exhibited symptoms of PTSD or partial PTSD. Risk factors for ongoing PTSD included major depressive disorder 1 to 2 years after the event, history of trauma, and extent of occupational exposure.5 Asthma rates are increased in the disaster responders as well, with a lifetime prevalence by 2007 that was almost twice (19% vs. 10%) that of the general population.6 On a larger scale, the World Trade Center Health Registry at the New York City Department of Health and Mental Hygiene will provide a 20-year follow-up through periodic contact with the enrollees7 (Box 27-1).
Box 27-1 World Trade Center Health Registry Projects
 Posttraumatic stress disorder (PTSD) among police
Posttraumatic stress disorder (PTSD) among police
 Unmet mental health care needs
Unmet mental health care needs
 Health of Staten Island landfill and barge recovery workers
Health of Staten Island landfill and barge recovery workers
 Respiratory and behavioral health of children
Respiratory and behavioral health of children
 Impact of 9/11 injuries on long-term enrollee health
Impact of 9/11 injuries on long-term enrollee health
 Coexistence, or comorbidity, of respiratory and mental health conditions experienced by many enrollees
Coexistence, or comorbidity, of respiratory and mental health conditions experienced by many enrollees
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree