Diffuse Large B-cell Lymphoma, Leg Type
Sa A. Wang, MD
Key Facts
Terminology
Primary cutaneous DLBCL composed exclusively of large transformed cells
Clinical Issues
20% of primary cutaneous B-cell lymphomas
Most cases arise in skin of lower leg(s)
˜ 85% of all cases
Subset of cases arise in skin of other sites (trunk, arms, head and neck)
˜ 15% of cases
Single or multiple lesions at time of presentation
Relapse is common; 50% 5-year survival
Treated with systemic R-CHOP
Microscopic Pathology
Diffuse pattern of involvement in dermis
Monotonous sheets of large immunoblasts or centroblasts
Few small reactive T cells in background
No centrocytes (or small B cells) present
No epidermotropism
Ancillary Tests
Pan-B-cell antigens (+), Bcl-2(+), Bcl-6(+)
MUM1(+), FOXP1(+), IgM(+), CD10(−)
Top Differential Diagnoses
Primary cutaneous follicle center lymphoma
Systemic DLBCL involving skin
Plasmablastic lymphoma involving skin
EBV(+) DLBCL of elderly
Monomorphic post-transplant lymphoproliferative disorder
TERMINOLOGY
Abbreviations
Primary cutaneous diffuse large B-cell lymphoma, leg type (PCDLBCL-LT)
Synonyms
Primary cutaneous large B-cell lymphoma, leg type
Primary cutaneous diffuse large B-cell lymphoma
Definitions
Primary cutaneous diffuse large B-cell lymphoma composed exclusively of large transformed B cells
Often occurs in lower leg(s), but can arise at other sites
ETIOLOGY/PATHOGENESIS
Cell of Origin
Peripheral B cell of post-germinal center cell origin
Immunophenotype: IRF-4/MUM1(+), FOXP1(+)
High frequency of somatic mutations of IgH variable (V)-region genes
Possible Role of Antigen Selection
Preferential use of certain IgHV gene segments
Suggests that antigen stimulation may be involved in pathogenesis
Role of Molecular Abnormalities
Number of genetic rearrangements and deletions reported
No abnormality consistently present
CLINICAL ISSUES
Epidemiology
Incidence
Rare
4% of all cutaneous lymphomas
20% of primary cutaneous B-cell lymphomas
Age
Elderly patients; median age: 7th decade
Gender
More common in women
Male to female ratio: 1:1.6; as high as 1:4 in some studies
Site
Most cases arise in skin of lower leg(s): 1 or both legs may be involved
˜ 85% of all cases
Subset of cases arise in skin of other sites (trunk, arms, head and neck)
˜ 15% of cases
Similar morphologic and immunophenotypic characteristics
Single or multiple lesions at time of presentation
Some patients have dissemination at initial diagnosis
Presentation
Red or blue-red cutaneous lesions
Plaque, verrucous plaques, or deep plaques
Nodular, tumoral lesions
Often associated with ulcer
Multiple lesions are common
B symptoms in 10-20% of patients
Treatment
Anthracycline-containing systemic chemotherapy plus rituximab (R-CHOP)
Radiotherapy has role for localized lesions in elderly patients
Prognosis
Relapse is common
40-50% 5-year survival rate
MICROSCOPIC PATHOLOGY
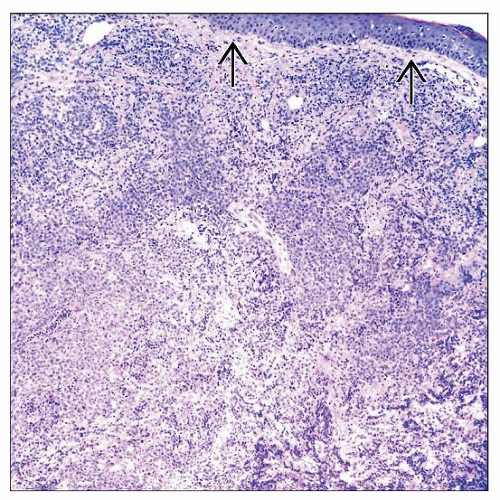
Histologic Features
Diffuse pattern of involvement of dermis
Infiltrate can be deep, often extending into superficial subcutaneous adipose tissue
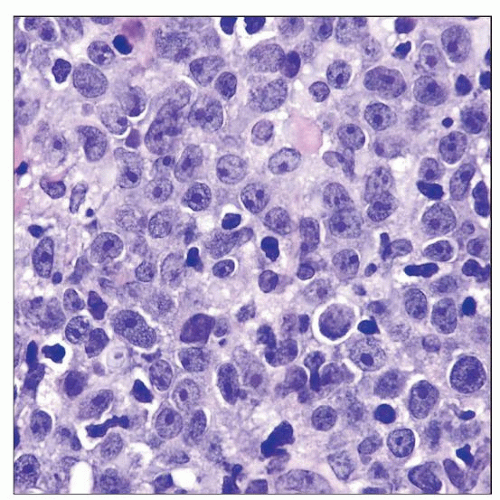
Cohesive, monotonous sheets of atypical-appearing large cells
Centroblasts or immunoblasts
Often very round nuclei
Mitotic figures numerous
Few small reactive T cells in background
No centrocytes (or small B cells) present
No epidermotropism
ANCILLARY TESTS
Immunohistochemistry
Pan-B-cell antigens (+)
Cytoplasmic IgM(+), IgD(+/−)
Bcl-2(+), IRF-4/MUM1(+), FOXP1(+)
Bcl-6(+), CD10(−)
No follicular dendritic cell (FDC) meshworks
CD21(−), CD23(−), CD35(−)
T-cell antigens (−), LMP1(−), HHV8(−)
In Situ Hybridization
FISH often shows rearrangements of MYC, BCL6, or IgH genes
No evidence of IgH-BCL2/t(14;18) or BCL2 rearrangements
EBER(−)
Array CGH
Amplification of 18q21.31-33 involving BCL2 and MALT1 genes
Molecular Genetics
Monoclonal IgH gene rearrangements
No evidence of IgH-BCL2/t(14;18)
Gene Expression Profiling
Profile is consistent with activated B-cell phenotype
DIFFERENTIAL DIAGNOSIS
Primary Cutaneous Follicle Center Cell Lymphoma (PCFCL)
Most PCFCL have follicular pattern and can therefore be distinguished from PCDLBCL-LT
PCFCL cases with diffuse pattern and predominance of large centrocytes or centroblasts are challenging
Used to be designated as diffuse large B-cell lymphoma (DLBCL)
However, clinically they are confined to skin, and prognosis is good
Could lead to over-treatment with multiagent chemotherapy
Sites of skin involvement
Mostly in head and neck, trunk, back, arms
Some cases of PCFCL can present on leg
Patients with PCFCL on leg often have worse prognosis than patients with PCFCL at other sites
Prognosis of PCFCL of leg is similar to, or slightly better than, PCDLBCL-LT
Histologic features of PCFCL
Areas of follicular pattern can be predominant, focal, or absent
Often, perivascular &/or periadnexal pattern in dermis is present
Mixture of centrocytes and centroblasts
Cells can be polylobated or spindle-shaped
Stromal reaction with fibrosis and sclerosis is common
Immunophenotype
CD10(+), Bcl-6(+); Bcl-2 often negative; if positive, often weak and focal
FDC meshwork is present
CD21, CD23, CD35, or other markers
IRF-4/MUM1(−), FOXP1(−)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree