Elevated blood pressure (BP) is one of the most common and important risk factors for cardiovascular (CV) and renal diseases. Worldwide, nearly 1 billion individuals (˜26% of adults) have hypertension (
1). Elevated BP is responsible for about 54% of strokes and 47% of ischemic heart disease events (
2) and for nearly 7.5 million deaths per year (
3). Consequently, elevated BP is considered the leading global cause of preventable deaths (
3), not only in high-income countries but also in low- and middle-income countries as well.
In the United States, about 31% of adults (nearly 68 million adults) have hypertension, defined as having a systolic BP (SBP) of 140 mm Hg or higher, a diastolic BP (DBP) of 90 mm Hg or higher, or treatment with antihypertensive drugs (
4). Additionally, at least as many US residents have prehypertension, defined as an SBP of 120 to 139 mm Hg or DBP of 80 to 89 mm Hg, without medication (
5). Unfortunately, control rates remain low at about 50% (
4,
5).
In all but a few isolated societies, SBP gradually increases with age (
6), and as a result, most adults develop hypertension in their lifetime. According to data from the Framingham Heart Study, roughly 90% of US adults will develop hypertension in their lifetime (
7). Both men and women are affected by elevated BP; and African-Americans, on average, have higher BP and a higher prevalence of hypertension than non-African-Americans (
5). African-Americans also have an increased risk of BP-related diseases, particularly stroke and kidney disease.
BP is a strong, independent, and etiologically relevant risk factor for CV and renal diseases (
8). The relationship between BP and the risk of CV disease is direct and progressive: as BP rises, so does the risk of CV disease throughout the range of BP including prehypertensive and hypertensive BP (
9). It has been estimated that nearly a third of BP-related deaths from coronary heart disease (CHD) occur in individuals with BP in the nonhypertensive range (
10). Correspondingly, prehypertensive individuals not only have a high likelihood of developing hypertension but also have an increased risk of CV disease compared with persons with normal BP (SBP <120 mm Hg and DBP <80 mm Hg) (
11).
Elevated BP results from environmental factors, genetic factors, and interactions among these factors. Of the environmental factors that influence BP (diet, physical inactivity, toxins, and psychosocial factors), dietary factors likely have a predominant role. Reducing weight and decreasing dietary sodium intake lower BP, as does increased potassium intake. For persons who drink alcohol excessively, limiting alcohol consumption to moderate levels also reduces BP. Since 1997, consumption of a diet similar to the ones tested in the Dietary Approaches to Stop Hypertension (DASH) and Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart) has emerged as an effective strategy to lower BP (
12).
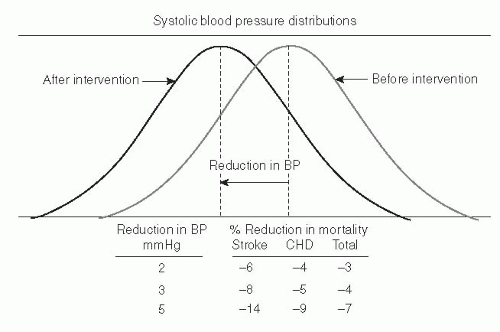
Dietary changes that lower BP can prevent nonhypertensive individuals from developing hypertension and reduce their risk of BP-related CV disease. In fact, even minor reductions in BP across an entire population could have a tremendous, beneficial public health impact. For example, it has been estimated that an 8% reduction in stroke mortality and a 5% reduction in mortality from CHD could result from just a 3 mm Hg reduction in SBP (
Fig. 66.1) (
13). Dietary changes can serve as first-line therapy, before antihypertensive medication, for treating uncomplicated stage I hypertension (SBP 140 to 159 mm Hg or DBP 90 to 99 mm Hg). Among hypertensive individuals who are already taking medication, dietary changes, particularly reduced sodium intake, can further lower BP and make it possible to reduce the number and dose of antihypertensive medications. In general, BP reductions from dietary changes are greater in hypertensive than in nonhypertensive individuals.
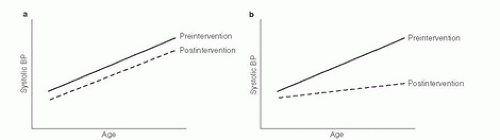
Although there is ample evidence that dietary changes lower BP, there are fewer data on whether dietary changes can reduce the age-related rise in SBP, which is approximately 0.6 mm Hg per year in adults (
14). Trials of dietary changes are often less than 3 years in duration and therefore are not of sufficient duration to answer that question. Hence, whether the BP reductions observed in these trials have merely shifted the age-related rise in BP curve downward, without a change in slope (
Fig. 66.2A), or have actually reduced its slope (see
Fig. 66.2B) cannot be determined from short-term trials (
15). Nonetheless, migration studies, ecologic studies, and, most recently, observational analyses of trial data (
16) offer some evidence to suggest that dietary factors may indeed reduce the age-associated rise in SBP.
This chapter reviews the evidence on the relationship between diet and BP. The summary of evidence and corresponding recommendations largely reflects existing reviews and consensus statements. (
15,
17,
18).
Table 66.1 provides a summary of this evidence, whereas
Table 66.2 provides a summary of recommendations.