Chapter 22 After studying this chapter, the learner will be able to: • List several invasive diagnostic tests. • List several noninvasive diagnostic tests. • List several interventional procedures that incorporate diagnostics. • Describe several aspects of patient care associated with diagnostic testing. Diagnosis of a pathologic disease, anomaly, or traumatic injury is established before a surgical procedure is undertaken. Many modalities and techniques help surgeons assess each individual patient problem, guide them through the surgical procedure, and help them verify the results of surgical intervention. The term diagnosis refers to the art or the act of determining the nature of a patient’s disease. Diagnostic procedures can be classified as follows: • Noninvasive. Noninvasive techniques use equipment placed on or near the patient’s skin but outside body tissues. • Invasive. Invasive techniques use equipment placed into a body cavity or vessel and/or use substances injected into body structures. • Interventional. Interventional techniques involve invasive diagnostics and procedures performed in a specialty department, such as in radiology. 1. Patients should be assessed for their physical condition and any metal implants, pacemakers, infusion pumps, sensitivities, and allergies. 2. Clear instructions should be given verbally and in writing before the test is performed. 3. Preprocedure preparations should be confirmed before the patient begins testing. A timeout process that includes the pertinent patient and procedure information should be conducted by the team. 4. Explanations of procedures should be given to patients to allay fears and ensure their understanding of the value of the procedure in making a diagnosis. Before the procedure begins, an explanation should be given of the equipment being used. 5. Sterile and aseptic techniques of invasive procedures are strictly observed. A mass or entire structure is cut from the body. The advent of fine needle aspiration has decreased the need for full excisional biopsy with the exception of a friable organ or a breast mass. In diagnosing lymphoma, an entire lymph node is necessary for adequate diagnosis. Some excisional biopsies can be performed endoscopically (Fig. 22-1). The specimen is placed in fixative, commonly formalin, for several hours to cause the cells to become firm. The fixed specimen is placed in a machine that removes all of the water from the tissues, replacing it with paraffin. When this process is complete, the specimen is embedded into a block of wax. It is placed in a microtome and is sliced tissue-paper thin and floated in a bath of water. The slices are placed on glass slides, where the paraffin is dissolved with solvent and the water is restored to the tissue on the slide. The slices readily accept dyes and stains used for diagnosis. Permanent section is the best diagnostic biopsy tool. Box 22-1 lists several tissue dyes and stains used in diagnostic procedures. Correct solutions for storage and correct labeling of specimens are critical for accurate diagnosis. Table 22-1 lists types of specimens for pathologic study. TABLE 22-1 Specimen Types and Considerations for Handling • Pathology tissue specimens should not be allowed to dry out. Saline or a solution of aqueous formaldehyde (10% formalin) is commonly used as the fixative until the specimen is processed further in the laboratory. Formalin is flammable and should not be stored in the OR. The formalin is added after the specimen is in the container. Dropping the specimen into a prefilled container can cause a splash. Some pathology laboratories prefer moistening the specimen with sterile normal saline. Check for the preference of the laboratory that will be examining the specimen. Fresh tissue and frozen sections are not placed in preservative solution or saline unless instructed otherwise by the lab personnel. • Stones are placed in a dry container so they will not dissolve. Organs containing stones, such as the gallbladder, may be placed in saline or formalin. • Foreign bodies should be sent for accession according to policy, and a record is kept for legal purposes. The description and the disposition of the object are recorded. A foreign body may be given to the police, surgeon, or patient, depending on legal implications, policy, or the surgeon’s wishes. A chain of specimen custody slip should be signed by all persons handling the specimen. • Forensic evidence, such as bullets or knife blades, should be placed in a dry plastic container. Do not allow the item to contact metallic basins because ballistic evidence could be altered. Chain of custody documentation should accompany the specimen at all times to protect the evidence. • Amputated extremities are wrapped in plastic before sending them to a refrigerator in the laboratory or morgue. Avoid placing the amputated limb in the patient’s field of vision. Most patients needing amputation have spinal or epidural anesthesia for the procedure. The sight of the body part may cause emotional distress in the patient. The patient may request that an amputated extremity be sent to a mortuary for preservation for burial with his or her body after death. This request must be noted on the requisition sent to the laboratory. Refer to institutional policy and procedure for the care of amputated limbs. Agents composed of nonmetallic compounds or heavy metallic salts that do not permit passage of radiant energy are radiopaque. When exposed to x-rays, the lumina of body structures filled with these agents appear as dense areas. Radiopaque contrast media frequently used for the procedures to be described are listed in Box 22-2. Some contrast agents are fluorescent dyes. Most contain iodine, either bound or unbound. The contrast media is designated low-osmolarity or high-osmolarity. Low-osmolarity is associated with fewer reactions to contrast.1–2,6,9,10 Few patients have an immediate reaction; however, a small population of patients may react several hours later. Known reactors may be given prednisone and Benadryl several hours before the anticipated use of any contrast agents.9,10 A history of systemic sensitivity to substances that contain iodine, such as shellfish, or other allergies is obtained before these agents are injected.2,8 True shellfish allergies are not related to iodine, but to specific proteins in the fish. True allergy is not a common event.2,5,9 Studies have shown that other allergies, such as milk and egg, both high in protein, may play a role. Precautionary administration of prednisone and Benadryl minimizes the risk. The use of low-osmolarity contrast helps to decrease reactions.9 Iodine allergy information may be unreliable, because studies have shown that immediate reactions to contrast are nonimmunologic in nature.5,9 This means that the adverse reaction is not caused by allergy. The patient’s Ig-E immunoglobulin is not activated. True allergic reactions to any contrast agent ingredient stimulate Ig-E immunoglobulin and the patient can exhibit hives, angioedema, respiratory difficulty, and cardiovascular collapse.1,2,9 The tabletop the patient lies on is made of acrylic or some other radiolucent material (Fig. 22-2). Some operating beds have a Bakelite top that fits over the length of the table and permits insertion of the x-ray cassette at any area. For fluoroscopy with image intensification, the entire top must be radiolucent because the image intensifier is positioned underneath the table. If the entire operating bed is not radiolucent, the foot section can be lowered and a radiolucent extension attached that will accommodate specialized x-ray machinery. Designed primarily for orthopedic procedures, foreign body and calculi localization, and catheter placement, mobile image intensifiers offer the same advantages and disadvantages as do portable x-ray machines. The C-arm, so named because of its shape (see Fig. 13-2), keeps the image intensifier and x-ray tube in alignment; the intensifier is directly under the tube. It can be moved from an anterior to a lateral position. Utility of the mobile C-arm image intensifier is enhanced when the system is capable of making electronic x-rays for permanent records. An additional formatting device is required for this function. Every patient should be taught breast self-examination and practice it every month as a baseline diagnostic test. Early diagnosis is the best chance for a cure. Figure 22-3 depicts the average sizes of masses discovered in patients who do and do not practice breast self-examination. 1. Access to the vessel (either an artery or vein) to be injected with a radiopaque contrast medium may be made by a percutaneous puncture or a cutdown. An IV drip is maintained when the latter approach is used. a. Cannulated needles with or without a radiopaque plastic catheter, similar to those used for IV infusions, may be used for a percutaneous puncture to penetrate an artery or vein. To prevent backflow of blood, cannulated needles have an obturator that remains in place until the contrast medium is injected. Long catheters have a guidewire to assist threading through the vessel. b. A Seldinger (18-gauge) needle has a sharply beveled inner cannula and a blunt outer cannula. The blunt end of the outer cannula prevents trauma to the vessel. After insertion, the inner cannula is replaced with a guidewire and the outer cannula is removed. A 20-cm vessel dilator sheath (which is approximately 8 inches long) is threaded over the guidewire to create a track for a radiopaque catheter. After the dilator sheath is removed, the catheter is positioned and the guidewire is withdrawn. This method is generally preferred for angiography because blood vessels other than the one punctured can be injected with contrast medium.
Diagnostics, specimens, and oncologic considerations
Diagnosing pathology
Patient care considerations for diagnostic procedures
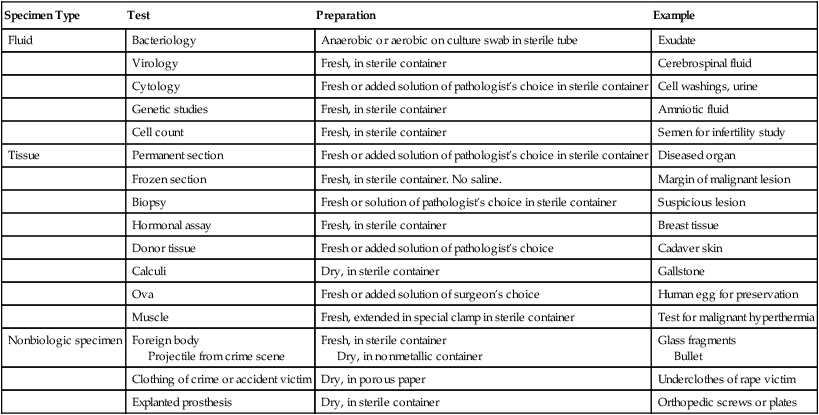
Specimens and pathologic examination
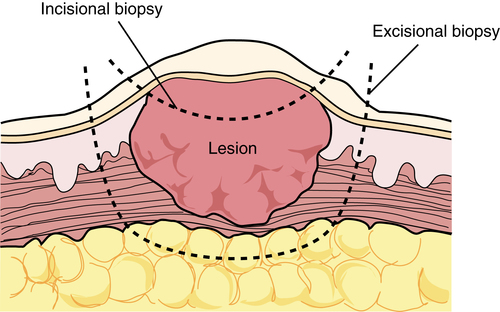
Biopsies
Excisional biopsy
Permanent section
Collecting surgical specimens
Specimen Type
Test
Preparation
Example
Fluid
Bacteriology
Anaerobic or aerobic on culture swab in sterile tube
Exudate
Virology
Fresh, in sterile container
Cerebrospinal fluid
Cytology
Fresh or added solution of pathologist’s choice in sterile container
Cell washings, urine
Genetic studies
Fresh, in sterile container
Amniotic fluid
Cell count
Fresh, in sterile container
Semen for infertility study
Tissue
Permanent section
Fresh or added solution of pathologist’s choice in sterile container
Diseased organ
Frozen section
Fresh, in sterile container. No saline.
Margin of malignant lesion
Biopsy
Fresh or solution of pathologist’s choice in sterile container
Suspicious lesion
Hormonal assay
Fresh, in sterile container
Breast tissue
Donor tissue
Fresh or added solution of pathologist’s choice
Cadaver skin
Calculi
Dry, in sterile container
Gallstone
Ova
Fresh or added solution of surgeon’s choice
Human egg for preservation
Muscle
Fresh, extended in special clamp in sterile container
Test for malignant hyperthermia
Nonbiologic specimen
Foreign body
Projectile from crime scene
Fresh, in sterile container
Dry, in nonmetallic container
Glass fragments
Bullet
Clothing of crime or accident victim
Dry, in porous paper
Underclothes of rape victim
Explanted prosthesis
Dry, in sterile container
Orthopedic screws or plates
Radiologic examination
Types of radiologic equipment and accessories
Contrast media
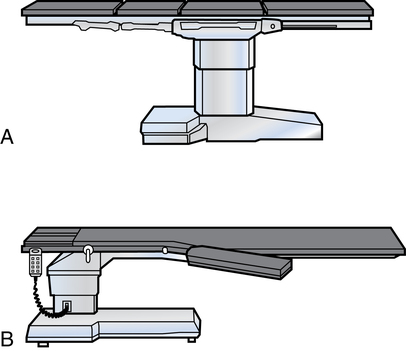
Radiologic table
C-arm image intensifier
Radiologic diagnostic procedures
Chest x-ray
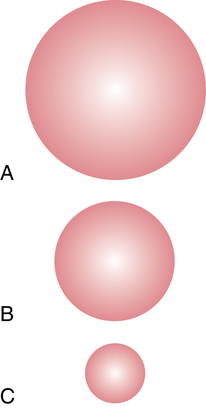
Mammography
Patient teaching.
Angiography and arteriography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Website
Website