Patient Story
A 38-year-old man saw a physician for the first time in 10 years after noticing visual loss in his left eye. His history revealed many risk factors for and symptoms of diabetes mellitus (DM). On an undilated funduscopic examination, his physician was able to see some hemorrhages and hard exudates. A fingerstick in the office showed a blood glucose level of 420 mg/dL. He was treated for DM and referred to an ophthalmologist to be evaluated for his diabetic retinopathy (Figure 20-1).
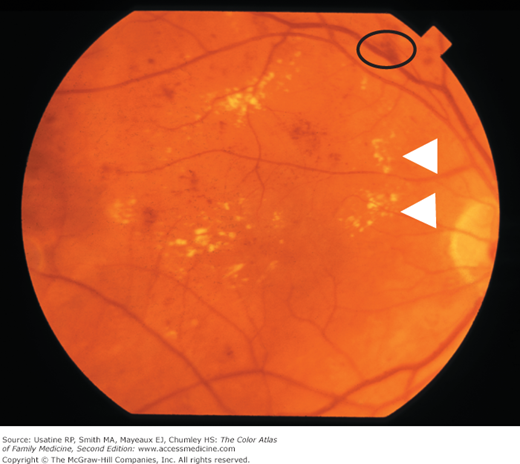
Figure 20-1
Dilated funduscopic photograph demonstrating microaneurysms (small red swellings attached to vessels), which are often the first change in diabetic retinopathy. Also present are flame hemorrhages (black oval) hemorrhages and hard exudates (yellow). Some of the hard exudates are demonstrated with white arrowheads. This case is an example of diabetic nonproliferative retinopathy. (Courtesy of Paul D. Comeau.)
Introduction
Diabetic retinopathy (DR) is a leading cause of blindness in the United States. Nonproliferative DR is characterized by microaneurysms, macular edema, cotton-wool spots, superficial (flame) or deep (dot-blot) hemorrhages, and exudates. Proliferative DR also has neovascularization of the retina, optic nerve head, or iris. Because patients may be asymptomatic until vision loss occurs, screening is indicated in all diabetic patients. Excellent glycemic control lowers a patient’s risk of developing DR.
Epidemiology
- In developed nations, DR is the leading cause of blindness among people younger than age 40 years.1
- In a community-based study, 29% of adults older than age 40 years with DM had DR. Prevalence in black patients was higher than in white patients (38.8% vs. 26.4%).2
- Twenty-one percent of patients have retinopathy at the time type 2 diabetes is diagnosed.3
- More than 60% of patients with type 2 DM have retinopathy within 20 years of diagnosis.3
- After 40 years of type 1 DM, 84% of patients have retinopathy.4
Etiology and Pathophysiology
- Hyperglycemia results in microvascular complications including retinopathy.
- Several biochemical pathways linking hyperglycemia and retinopathy have been proposed.3
- In nonproliferative retinopathy, microaneurysms weaken vessel walls. Vessels then leak fluid, lipids, and blood resulting in macular edema, exudates, and hemorrhages (Figures 20-1 and 20-2).
- Cotton-wool spots result when small vessel occlusion causes focal ischemia to the superficial nerve fiber layer of the retina.
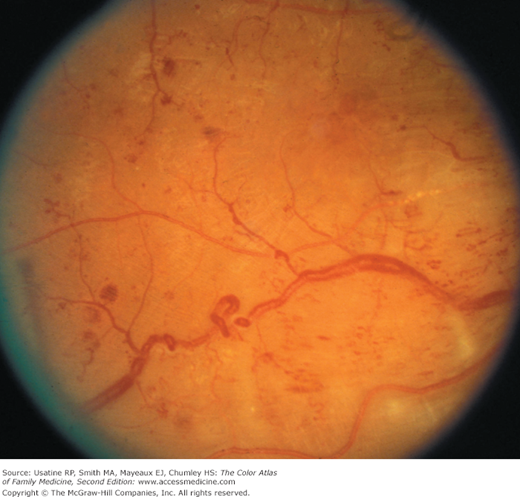
- In proliferative retinopathy, new blood vessels form in response to ischemia (Figure 20-3).
Figure 20-3
Proliferative diabetic retinopathy showing newly developed, porous, friable blood vessels. New vessels can be seen on the optic disc and peripheral retina. Panretinal photocoagulation may help prevent vitreous hemorrhage, retinal detachment, and neovascular glaucoma. (Courtesy of Paul D. Comeau.)
Risk Factors
- In type 1 DM, identified risk factors include: longer diabetes duration, high hemoglobin (Hgb) A1c, hypertension, smoking, and male gender.4,5
- In type 2 DM, identified risk factors include: longer diabetes duration, high HgbA1c, elevated systolic blood pressure, male gender, presence of albuminuria, and pharmacologic therapy.6
Diagnosis
- Gold standard is grading of stereoscopic color fundus photographs in seven standard fields.3
- In comparison with the gold standard, a single monochromatic digital photo through a nondilated eye is sufficient to determine the presence or absence of DR with a sensitivity and specificity of 71% and 96%, respectivey.7 SOR B