Data interpretation
 . Learn memorable and reliable methods of interpreting the most common test results.
. Learn memorable and reliable methods of interpreting the most common test results.
 . Learn how to interpret (and act on) drug-specific data.
. Learn how to interpret (and act on) drug-specific data.
 . Use 10 scenarios with worked answers to reinforce these principles.
. Use 10 scenarios with worked answers to reinforce these principles.
Structure of this Section within the PSA
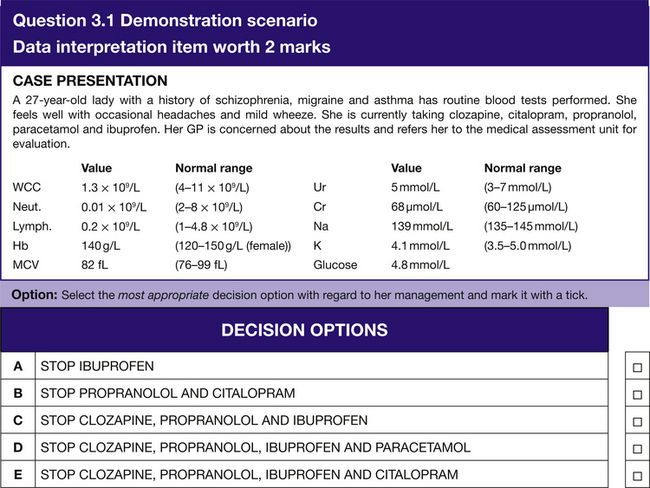
The ‘Data interpretation’ section will have 6 questions with 2 marks available per question, so a possible total of 12 points. The questions will be of the multiple choice style and you will be asked to select the most appropriate answer from a list of five options (A–E). See Question 3.1 for a demonstration scenario.
General Data Interpretation
Blood Tests: Haematology
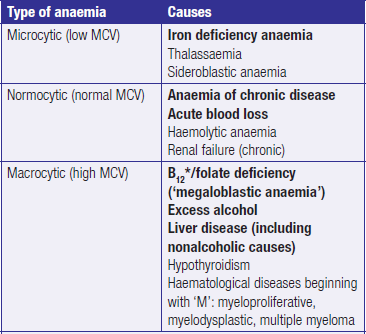
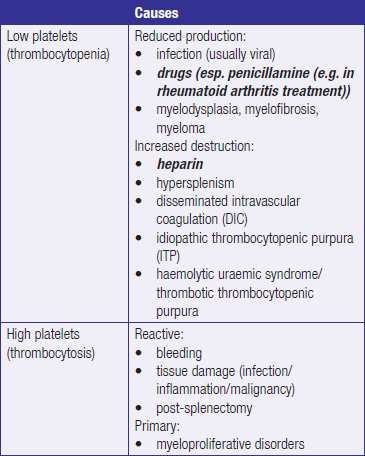
The most important results of a full blood count (FBC) are the haemoglobin, the white cell count (WCC) and the platelets. The most commonly encountered abnormalities are shown in Tables 3.1–3.3.
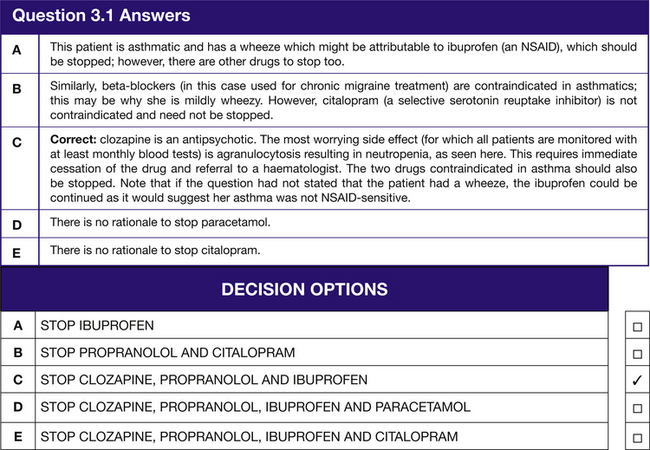
Table 3.2
High and low white blood cells
*Patients undergoing chemotherapy or radiotherapy may become neutropenic (or even pancytopenic) in response to infection (‘neutropenic sepsis’). This carries a much higher mortality rate so they must be given urgent IV broad-spectrum antibiotics (the choice is hospital specific).
Blood Tests: Biochemistry
Urea and electrolytes (U&E)
Sodium (normal range 135–145 mmol/L)
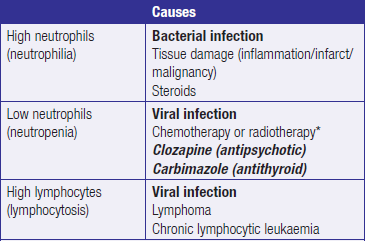
 Hyponatraemia: to help narrow the (wide) differential for hyponatraemia assess the patient’s fluid status (e.g.hypovolaemic/euvolaemic/hypervolaemic) (Table 3.4).
Hyponatraemia: to help narrow the (wide) differential for hyponatraemia assess the patient’s fluid status (e.g.hypovolaemic/euvolaemic/hypervolaemic) (Table 3.4).
Table 3.4
*Causes of SIADH can be remembered with the mnemonic SIADH: Small cell lung tumours, Infection, Abscess, Drugs (especially carbamazepine and antipsychotics), and Head injury.
 Hypernatreamia: causes of this all begin with ‘d’: dehydration; drips (i.e. too much IV saline); drugs (e.g. effervescent tablet preparations or intravenous preparations with a high sodium content); diabetes insipidus (which is effectively the opposite of syndrome of inappropriate anti-diuretic hormone (SIADH).
Hypernatreamia: causes of this all begin with ‘d’: dehydration; drips (i.e. too much IV saline); drugs (e.g. effervescent tablet preparations or intravenous preparations with a high sodium content); diabetes insipidus (which is effectively the opposite of syndrome of inappropriate anti-diuretic hormone (SIADH).
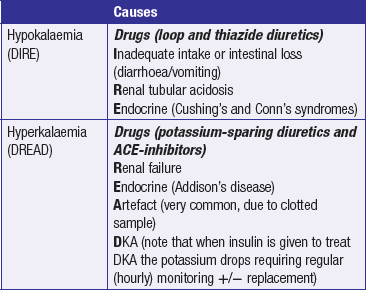
Potassium (normal range 3.5–5.0 mmol/L)
Hypokalaemia and hyperkalaemia are particularly important because they cause fatal cardiac arrhythmias. Their causes may thus be remembered with the mnemonics DIRE and DREAD (Table 3.5).
Liver Function Tests (LFTs)
One can assess the liver by looking at markers of:
LFTs help to narrow the causes of raised bilirubin (which may cause jaundice) (Table 3.7). A raised bilirubin on its own indicates prehepatic jaundice (see later in this chapter) that is rarely due to any liver problem itself (in the same way a raised urea on its own (i.e. prerenal AKI) rarely indicates an intrinsic renal problem); rather, because bilirubin is a breakdown product of haemoglobin, a solitary raised bilirubin usually indicates haemolysis.
Table 3.7
Causes of deranged liver function tests
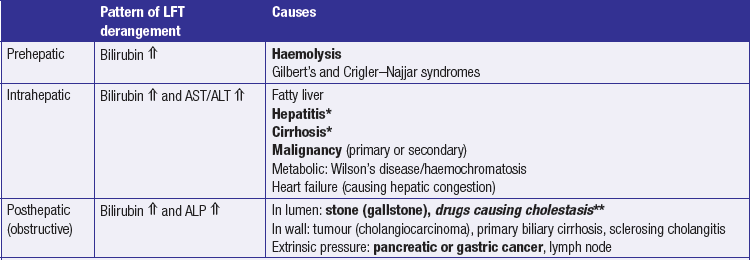
*Hepatitis and cirrhosis may be due to (1) alcohol, (2) viruses (Hepatitis A–E, CMV and EBV), (3) drugs (paracetamol overdose, statins, rifampicin), and (4) autoimmune (primary biliary cirrhosis, primary sclerosing cholangitis and autoimmune hepatitis).
**Flucloxacillin, coamoxiclav, nitrofurantoin, steroids and sulphonylureas.
Thyroid Function Tests (TFT)
TFTs assess the thyroid stimulating hormone (TSH) and T4; Table 3.8 shows the most common abnormal patterns and causes. In the PSA, students may be asked to change a levothyroxine dose according to TFT results for patients with hypothyroidism (Table 3.9). The trick to this is to use the TSH as a guide: target range ~0.5–5 mIU/L and, unless grossly hypo/hyperthyroid, change by the smallest increment offered.
Table 3.8
Abnormal thyroid function tests.
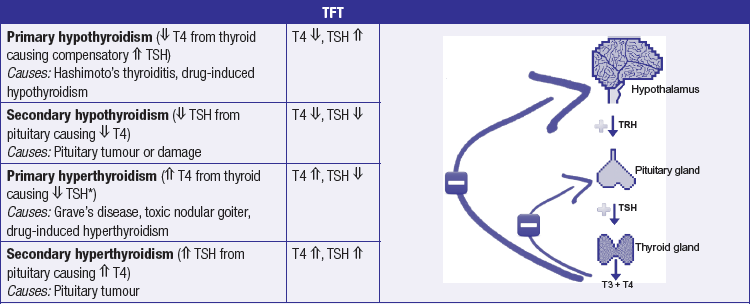
*Through negative feedback from increased T4 levels.
(image at right from GeekyMedics.com, with permission)
Table 3.9
How to interpret and change levothyroxine dose following TFT results
| TSH range (mIU/L) | Change to thyroxine |
| <0.5 | Decrease dose |
| 0.5–5 | Nil action – same dose |
| >5 | Increase dose |
Chest X-Rays
Quality of film
It is important to check that the film is PRIM:
 Projection (e.g. posterioanterior (PA) (normally) or anterioposterior (AP). If AP the heart will appear larger. If no markings then it is PA)
Projection (e.g. posterioanterior (PA) (normally) or anterioposterior (AP). If AP the heart will appear larger. If no markings then it is PA)
 Rotation (e.g. if distance between spinous process and clavicles is equal then no rotation)
Rotation (e.g. if distance between spinous process and clavicles is equal then no rotation)
 Inspiration (e.g. if the seventh anterior (down-sloping) rib transects the diaphragm then adequate)
Inspiration (e.g. if the seventh anterior (down-sloping) rib transects the diaphragm then adequate)
 Markings (if additional markings, e.g. ‘red marks’, then the radiographer has spotted an abnormality).
Markings (if additional markings, e.g. ‘red marks’, then the radiographer has spotted an abnormality).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree