Cytomegalovirus Lymphadenitis
Sa A. Wang, MD
Key Facts
Terminology
Lymphadenitis caused by cytomegalovirus (CMV) infection
Etiology/Pathogenesis
Member of β-herpes viruses
Causes cytopathic changes
Lytic infection: Immediate-early, early, and late viral proteins
Immunocompetent hosts: Often primary infection
Immunocompromised patients: Reactivation
Clinical Issues
Diagnosis of CMV infection
Serology
Shell vial culture
CMV antigenemia assay
Molecular amplification
Treatment: Ganciclovir
Prognosis
In immunocompetent patients: Self-limited
CMV pneumonia in immunocompromised patients has high mortality rate
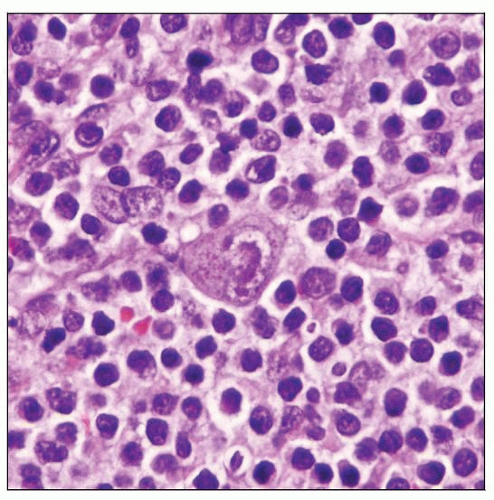
Microscopic Pathology
Follicular hyperplasia can be florid
Paracortical, interfollicular, and subcapsular areas
Immunoblasts, monocytoid B cells
Focal necrosis can be seen
CMV infected cells
Top Differential Diagnoses
Infectious mononucleosis
Other types of viral lymphadenitis
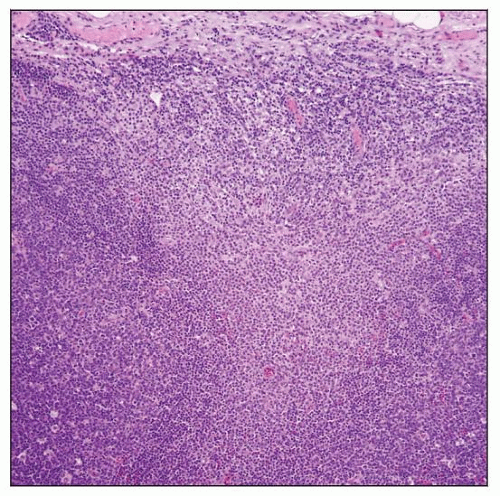 CMV lymphadenitis. This field shows that the sinus is expanded by monocytoid B cells between 2 large, reactive follicles (left and right). |
TERMINOLOGY
Abbreviations
Cytomegalovirus (CMV)
Definitions
Lymphadenitis caused by CMV infection
ETIOLOGY/PATHOGENESIS
CMV
Member of β-herpes virus family
Double-stranded DNA virus with 162 hexagonal protein capsomeres surrounded by lipid membrane
Lytic virus that causes cytopathic effect in vitro and in vivo
Productive (lytic) infection leads to synthesis of immediate-early, early, and late viral proteins
Viral DNA has been detected in monocytes, dendritic cells, megakaryocytes, and myeloid progenitor cells in bone marrow
Virus infects T cells but not B cells
Monocytes and endothelial cells are also commonly infected by CMV
Can be transmitted by a number of means
Person-to person via saliva, respiratory secretions, or sexual fluids
Blood transfusions
Transplacental passage
Immunology
Body produces neutralizing antibodies upon primary infection
Cell-mediated immunity is most important factor in controlling CMV infection
CMV Infection in Immunocompetent Host
Mostly primary infection
CMV Infection in Immunocompromised Patients
Reactivation of CMV, either iatrogenic or secondary to underlying medical conditions
Solid organ or bone marrow transplantation
Acquired immunodeficiency syndrome (AIDS)
CMV Infection in Pregnancy
Maternal primary CMV infection
In utero transmission of CMV, either due to primary CMV infection or reactivation
Can be lethal with damage to central nervous system (CNS)
CLINICAL ISSUES
Epidemiology
Incidence
Infection with CMV is common as determined by presence of serum antibodies
In developed countries, 60-80% of population is infected by adulthood
In developing countries, most children are infected by 3 years of age
> 90% of homosexual men are infected by CMV
Age, geography, cultural and socioeconomic status, and child rearing practices affect prevalence
Age
Congenital
1% of newborns are infected by CMV
Perinatal infection due to
Maternal cervicovaginal secretions during delivery
Breast feeding
Daycare toddlers
Horizontal transmission of virus to both children and adult daycare center workers
Adolescence
Sexual transmission
Immunocompromised patients, all ages
Blood or tissue exposure, all ages
Gender
No sex preference
Ethnicity
No preferences
Presentation
Immunocompetent patients
Asymptomatic or flu-like syndrome
Symptoms similar to infectious mononucleosis-type syndrome, but milder
Fever of unknown origin
Lymphadenopathy, often cervical
Pharyngitis
Hepatosplenomegaly
Blood: Lymphocytosis with atypical lymphocytes
CMV reactivation is common in critically ill immunocompetent patients
Can be associated with prolonged hospitalization
Immunocompromised patients
Organ transplant recipients and patients with immunodeficiency syndromes
Interstitial pneumonitis
Respiratory symptoms, fever, and dyspnea
Can be life-threatening
Gastrointestinal infection
Esophagus: Dysphagia
Upper gastrointestinal tract: Ulcer
Colon: Bloody diarrhea, fever, and abdominal pain
CMV retinitis
Frequent in HIV patients with a CD4 count < 50 cells/µL
Decreased/impaired visual acuity, floaters, and loss of visual fields on 1 side
Can progress to bilateral involvement if untreated
Neurologic manifestations
CMV encephalitis
Guillain-Barré syndrome
Other peripheral neuropathies
CMV hepatitis
Often subclinical
Unexplained fever
Abnormal liver function tests
Portal vein thrombosis (rare)
Pericarditis and myocarditis
Myeloradiculopathy
Disseminated CMV infection is criterion for AIDS
Congenital infection
At birth
Small size for gestational age
Hepatosplenomegaly
Petechiae and purpura of the skin, jaundice
Neurologic involvement: Microcephaly, seizures, and feeding difficulties
Sequelae in children
Sensorineural hearing loss
Chorioretinitis
Microcephaly, seizures, or paresis/paralysis
Mental retardation
Laboratory Tests
Serology
Recent and acute CMV infection
Detection of CMV-specific IgM antibodies
At least 4x increase in CMV-specific IgG titers in specimens obtained at least 2-4 weeks apart
To determine past exposure to CMV infection
If positive for past infection, monitor those at risk for CMV reactivation syndromes
If negative for past infection, monitor for new infection if transplanted with CMV seropositive organ
Early antigen detection (shell vial cultures)
Methods
Centrifugation of clinical samples (e.g., urine, blood) to increase absorption of virus
Infected cell monolayers incubated with monoclonal antibodies specific for CMV
Results typically available within 2-3 days
Accelerates time to diagnosis
CMV antigenemia assays
Methods
Using monoclonal antibodies specific to pp65 lower matrix protein of CMV to detect CMVinfected leukocytes in peripheral blood
Results are reported as number of cells with staining per total number of cells counted
Advantage
Results generally available within 24 hours
Antigenemia appears to correlate with viremia
Molecular methods for detecting CMV
Hybrid Capture System CMV DNA test
Signal amplification method using RNA probe that targets CMV
COBAS Amplicor test
PCR assay that amplifies 365 base pair region of CMV polymerase gene
Nucleic acid sequence-based amplification (NASBA)
Detects both immediate-early gene UL123 (IE1) and late gene expression (pp67)
Utility
Sensitive and specific for organ transplant patients
Not sensitive in detecting acute CMV infection
Other laboratory findings
Heterophile antibody is negative
Hematologic findings: Absolute lymphocytosis and atypical lymphocytes
CD4:CD8 ratio reversed
Increased large granular lymphocytes, NK cells
Viral cultures
CMV grows slowly in cell culture
Not a rapid confirmatory test
Positive result does not confirm active CMV disease
Limited sensitivity
Treatment
Drugs
Antiviral agents have value
Ganciclovir
Foscarnet (Foscavir)
Valganciclovir
Cidofovir (Vistide)
Therapy for bone marrow or solid organ transplant patients
Prophylaxis
Patients who have positive CMV serology
CMV-positive donor with CMV-negative recipient
Preemptive therapy
Patients who have evidence of ongoing viral replication
In HIV(+) or AIDS patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree