Cystadenoma and Epithelial Stromal Tumor
Gladell P. Paner, MD
Mahul B. Amin, MD
Key Facts
Clinical Issues
Rare, < 25 reported tumors within spectrum of seminal vesicle cystadenoma and epithelial stromal tumors
Obstructive symptoms most common presentation
Cystadenoma and low-grade epithelial stromal tumors have benign course but may recur
2 reports of high-grade epithelial stromal tumors with metastasis
Microscopic Pathology
Cystadenoma
Consists of multiple variably sized cystic and glandular formations lined by single to few layers of bland cuboidal to low columnar epithelial cells
Variable amount of stroma that resembles usual seminal vesicle fibromuscular stroma
Epithelial stromal tumors
Consist of neoplastic proliferation of both glandular and stromal elements
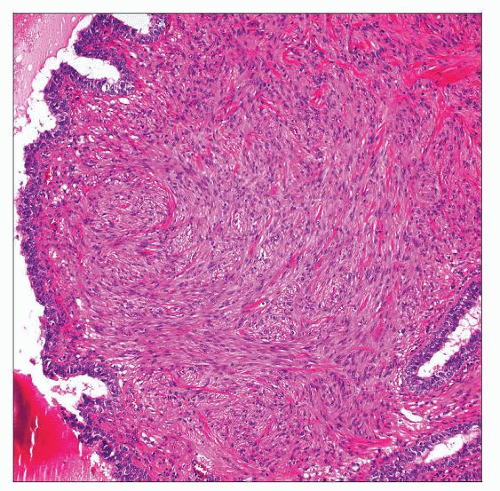
May have broad leaf-like growth consisting of epithelium with investing spindle cell stroma (phyllodes-like growth)
Histologic spectrum of benign to malignant tumors defined by degree of atypicality of stromal component
Includes low-grade fibroadenoma/adenomyoma and high-grade epithelial stromal tumors
High-grade tumors contain frank sarcomatous areas, including marked stromal overgrowth, pleomorphism, frequent mitosis, and necrosis
Ancillary Tests
Epithelial component PSA/PAP(-)
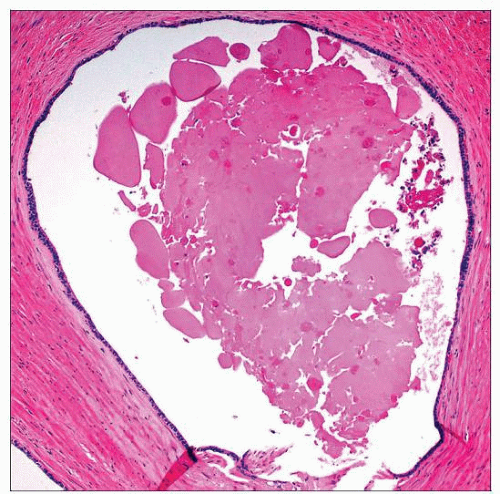 Seminal vesicle cystadenoma consists of cysts lined by single to few layers of epithelial cells and underlying fibromuscular stroma. The cyst lumen contains amorphous eosinophilic material. |
TERMINOLOGY
Synonyms
Cystadenoma
Multilocular cyst
Epithelial stromal tumors
Mesonephric hamartoma, fibroepithelial tumor, cystomyoma, mesenchymoma, phyllodes tumor, cystosarcoma phyllodes, müllerian adenosarcomalike tumor
Definitions
Cystadenoma
Benign cystic epithelial neoplasm of seminal vesicle
Tumor lacking significant stromal proliferation or containing only usual seminal vesicle-type stroma
Epithelial stromal tumor
Seminal vesicle neoplasm with proliferation of both glandular and stromal elements
Considerable overlap in literature with use of terminology regarding cystadenoma and low-grade epithelial stromal tumor
Debatable whether cystadenoma is in same spectrum with low-grade epithelial stromal tumors that lack prominent stromal proliferation
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
No association with ureter or renal developmental anomalies, in contrast to nonneoplastic congenital seminal vesicle cysts, which have such an association
CLINICAL ISSUES
Epidemiology
Incidence
Very rare
Overall, < 25 reported tumors within spectrum of seminal vesicle cystadenoma and epithelial stromal tumors, including malignant cases
Age
Mean: 51 years, range: 33-70 years
Presentation
Obstructive symptoms most common
Acute urinary retention, decreased urine stream, hesitancy, frequency, dysuria, and nocturia
Other symptoms include lower abdominal pain, painful ejaculation, constipation, fever
Few cases are asymptomatic &/or detected as pelvic or rectal mass on physical examination
Laboratory Tests
Normal serum PSA level
Normal serum CA125 level (in contrast to seminal vesicle adenocarcinoma, which may have elevated level)
Treatment
Tumor resection with vesiculectomy, prostatectomy, or cystoprostatectomy
Systemic chemotherapy for malignant epithelial and stromal tumor, particularly if metastatic
Prognosis
Cystadenoma has a benign course but may recur
No metastasis reported in epithelial stromal tumors lacking high-grade features but may recur
2 reports of high-grade epithelial stromal tumors have demonstrated metastasis to lung with subsequent death in 1 patient
IMAGE FINDINGS
General Features
CT and MR show multilocular cystic or solid-cystic pelvic mass centered in region of seminal vesicle between rectum and urinary bladder or prostate
Tumor may appear more solid in malignant cases
Large mass often compresses or displaces urinary bladder and prostate
Imaging may be key to determine origin (seminal vesicle vs. prostate), particularly in biopsy specimens
MACROSCOPIC FEATURES