Cryptorchidism
Steven S. Shen, MD, PhD
Key Facts
Terminology
Testis present outside scrotum and cannot be moved into scrotum
Clinical Issues
Most common birth defect of male genitalia
1% of infants have incompletely descended testes 12 months after birth
Cryptorchidism increases risk of testicular cancer 4-10x
Most common problem caused by cryptorchidism is infertility
90% can be palpable in inguinal canal (10% in abdomen or nonexistent, truly hidden, or anorchia)
Macroscopic Features
Abnormal location and usually smaller-sized testis than normal or contralateral testis
Microscopic Pathology
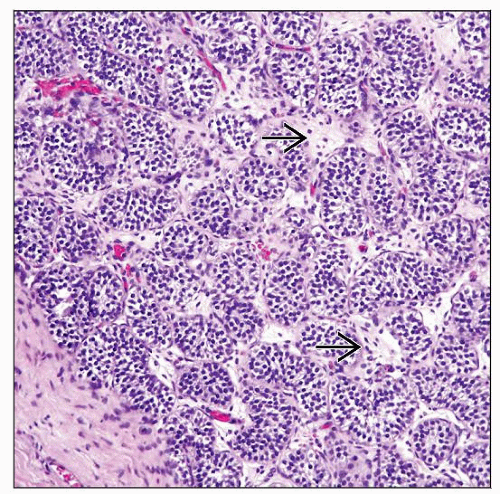
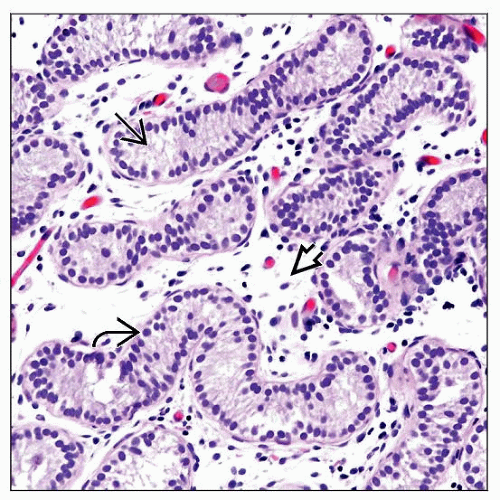
Type I (slight alterations): Tubular fertility index > 50; mean tubular diameter decreased by < 10%
Type II (marked germinal hypoplasia): Tubular fertility index 30-50; mean tubular diameter 10-30% below normal
Type III (severe germinal hypoplasia): Tubular fertility index < 30; mean tubular diameter > 30% below normal
Testicular parenchyma can be hypoplastic or dysgenetic
TERMINOLOGY
Synonyms
Undescended testis
Definitions
Greek word “crypto” (meaning hidden) and “orchid” (meaning testicle)
1 or both testes present outside scrotum with failure to descend into scrotum (empty scrotum)
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
Idiopathic
Anomalies in anatomic development
Defect in fetal androgens or excess maternal estrogen
Possible common genetic abnormality causing undescended testis and predisposing to carcinoma of testis
Associated with congenital malformation syndromes such as Prader-Willi syndrome, Noonan syndrome, and cloacal exstrophy
Acquired Cryptorchidism
Postoperative trapped testis
Spontaneous ascent (idiopathic)
CLINICAL ISSUES
Epidemiology
Incidence
Most common birth defect of male genitalia
3% of full-term newborns have an undescended testis
1% of infants have incompletely descended testes 12 months after birth
More common in premature infants (30% of boys born at 30 weeks gestational age)
True cryptorchidism accounts for 25% of cases of empty scrotum
Presentation
No particular symptoms; empty scrotal sac usually detected by parents
About 2/3 unilateral and 1/3 bilateral
90% may be palpable in inguinal canal (10% in abdomen or nonexistent, truly hidden, or anorchia)
May be found anywhere along “path of descent” from retroperitoneum to inguinal ring
Rarely located outside of “path of descent” (ectopic), such as in the perineum, opposite scrotum or femoral canal, under the skin, or outside the inguinal canal
Natural History
Predisposition to testicular germ cell neoplasia
Cryptorchidism increases risk of testicular cancer by 4-10x
Most common tumor in undescended testis is seminoma
Contralateral testis is primary site in 20% of cases
Orchiopexy facilitates self-examination and may decrease risk of germ cell tumor
Infertility
Most common problem caused by cryptorchidism
Tubular fertility index (number of germ cells per cross-sectioned tubule) is most important factor
75-85% of cryptorchid males have sperm count below normal
Location and size of cryptorchid testis have no influence on fertility
Torsion
Psychological
Treatment
May receive hormone injection (β-hCG or testosterone) to try bringing testicle into scrotum
If medical treatment is unsuccessful, early orchiopexy (˜ 1 year of age) should be performed to prevent irreversible damage to testicle
Prognosis
Most will descend into scrotum without any intervention during 1st year of life
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree