Fig. 21.1 Muscular anatomy of the face.
Treatment techniques
Botulinum neurotoxin can be reconstituted using non-preserved normal saline (per the manufacturer’s recommendations) or preserved normal saline. The benzyl alcohol preservative has no negative effects on the efficacy of the BoNT and, as a benefit, provides some anesthesia to the patient upon injection (Alam et al., 2002).
The dilution of BoNT varies between injectors but is generally in the 1–5 ml range per 100 U (onabotulinumtoxinA/incobotulinumtoxinA) or 300 U (abobotulinumtoxinA). At our institution, we dilute 100 U onabotulinumtoxinA/incobotulinumtoxinA or 300 U abobotulinumtoxinA with 2.5 ml of preserved normal saline. This yields 4 U/0.1 ml onabotulinumtoxinA/incobotulinumtoxinA and 12 U/0.1 ml abobotulinumtoxinA, effectively standardizing the volume injected across BoNT products. This ensures an appropriate level of dosing irrespective of which BoNT product is chosen.
For a syringe, most injectors chose either a 1 ml tuberculin syringe or an insulin syringe. The 1 ml tuberculin syringe offers flexibility in needle selection for drawing up the product (e.g. an 18- or 25-gauge for a more rapid draw) and for injection (generally a 30- or 32-gauge needle). An insulin syringe offers very good injection control, a fine needle and no product left in the hub.
Ideally, to mitigate bruising, a patient would not be taking any medication to thin the blood: aspirin or other non-steroidal anti-inflammatory drug, fish oil, gingko biloba, warfarin, vitamin E, garlic. In practice, however, it is often inconvenient or medically unwise to discontinue the medications.
In preparation for injection, the patient should be upright on the examination table or chair. The skin is cleansed with alcohol. Although topical anesthetics and ice packs are unnecessary, they can be used preoperatively for patients who experience excessive discomfort.
Many physicians recommend the following after injection:
- contract the treated muscles periodically for 2–3 hours following injection
- do not bend over for 2–3 hours, for example to tie shoes or pick an object off the floor
- do not massage the treated area for 2–3 hours following injection
- do not lie down for 2–4 hours following injection
- limit heavy activity for 2–4 hours.
In practice, there is little evidence to support such recommendations.
Cosmetic uses of botulinum neurotoxin
The first step to achieving desirable results (and pleasing the patient) is a clear understanding of the patient’s reason for presentation, followed by a thorough analysis of the patient’s facial expression and appearance. The primary use of BoNT is to soften or eliminate dynamic rhytids – those wrinkles that deepen with movement – and, less often, for facial sculpting.
A careful analysis of the patient’s face – often conducted with the patient looking into the mirror – is critical. Many, if not most, humans have facial asymmetry. This often goes unnoticed by the patient and is important to identify and to discuss with the patient. The size and strength of the target muscles needs to be assessed since this will have significant bearing on the amount of product needed. Once the patient’s concerns are noted, and the facial analysis completed, a treatment strategy can be discussed.
Dynamic rhytids
Glabella
The glabellar wrinkles – those wrinkles between the eyebrows – are perhaps the most common area for injection of BoNT. The so-called “glabellar complex” or “depressor complex” comprises four muscles that pull the central brow down and in: procerus, orbicularis oculi, corrugator supercilliaris and depressor supercillii. The primary targets for BoNT are procerus and corrugator supercilliaris, but the entire depressor complex will be affected.
Prior to injection, the patient should be asked to frown, which will delineate the target muscles (Fig. 21.2). Procerus is a relatively easily identifiable muscle, the belly becoming more obvious with contraction. The bulk of the muscle generally lies between the brows, just over the nasal root. Landmarks can be of help in identifying the procerus injection site: an “X” is drawn connecting the medial eyebrows and the contralateral medial canthi (Fig. 21.3).
Fig. 21.2 Treatment of the glabellar complex. (a) The glabellar lines at rest. The numbers indicate the approximate units of onabotulinumtoxinA/incobotulinumtoxinA recommended; 20 U onabotulinumtoxinA/incobotulinumtoxinA (60 U abobotulinumtoxinA) were used. (b) Accentuation of the lines with frowning. (c,d) Post-treatment, the lines are diminished and the eyebrows elevated both at rest (c) and with activation (d).
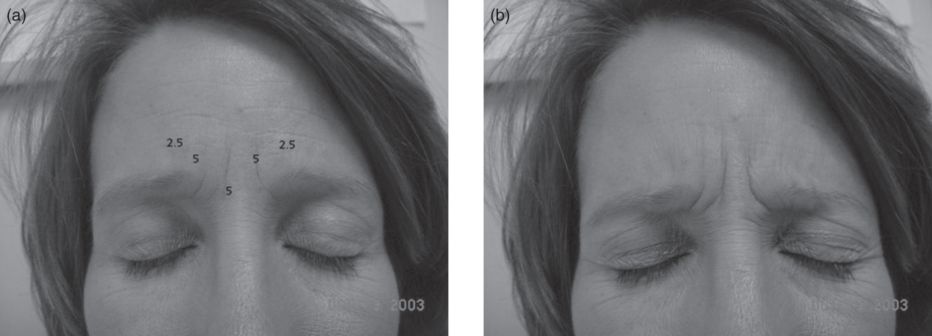
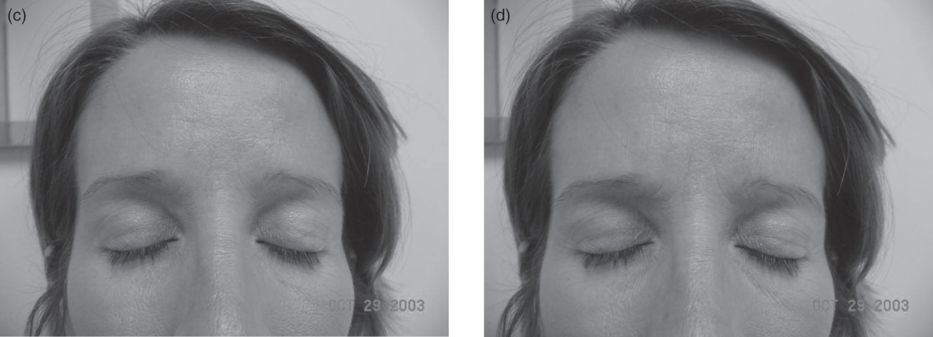
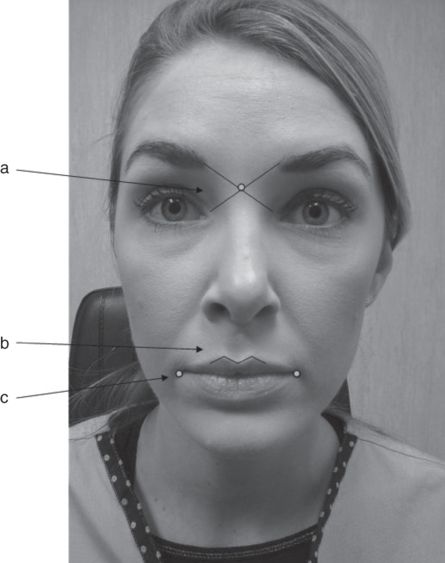
Fig. 21.3 Cosmetic landmarks. An “X” is drawn between the medial border of the eyebrow and the contralateral medial canthus (arrow a). The center of the “X” denotes the procerus muscle. The cupid’s bow of the mouth is normally not injected (arrow b). The oral commissure is a landmark for locating the depressor anguli oris muscle (arrow c).
The corrugators extend superolaterally from the procerus, and their lateral insertion sites can usually be seen as subtle dimples above the brow in the vicinity of the mid-pupillary line. The belly of the muscle generally lies above the medial canthus. The tail (which is often treated) is located approximately 1cm above the supraorbital notch in the midpupillary line. Since the insertion of the corrugators can vary, it is important to identify the muscles themselves, and not just target a region. Furthermore, the injection site should generally be at least 1 cm above the orbital rim in order to avoid blepharoptosis.
Five injections are commonly used to treat the area: belly of procerus, right and left medial corrugator (in the belly), and right and left lateral corrugator (the tail). Altogether 30–40 U onabotulinumtoxinA/incobotulinumtoxinA (90–120 U abobotulinumtoxinA) should be used for this area. Some injectors grip procerus between the thumb and forefinger of the non-dominant hand to stabilize the muscle, distract the patient and improve accuracy. Injections of 5–10 U onabotulinumtoxinA/incobotulinumtoxinA (15–30 U abobotulinumtoxinA) are often used here. Likewise, many injectors will grab the belly of corrugator between non-dominant thumb and forefinger (Fig. 21.4), or they will release the finger and just use the non-dominant thumb on the muscle to stabilize it. Injections of 4–8 U onabotulinumtoxinA/incobotulinumtoxinA (12–24 U abobotulinumtoxinA) are often used in the belly of corrugator, 2–4 U onabotulinumtoxinA/incobotulinumtoxinA (6–12 U abobotulinumtoxinA) in the tail.

Fig. 21.4 The non-dominant thumb and forefinger are used to stabilize the target muscle. The dominant hand injects. Any erythema and distention of the skin depicted here are common following injection and are transient.
Complications can result from excessive dosage or injections placed too inferiorly, particularly in the mid-pupillary line (i.e. the region of the tail of corrugator). This can cause blepharoptosis via inferior migration of BoNT and paralysis of levator palpebrae superioris. To correct the blepharoptosis, patients can be treated with apraclonidine 0.5% eyedrops, which is an alpha-2-adrenergic agonist that causes Müller’s muscle to contract (Wollina and Konrad, 2005).
Forehead
Horizontal lines in the forehead are treated by targeting the frontalis muscle. In many individuals, the central portion of the forehead above the glabellar complex is not covered by frontalis but rather by a membranous galea. In these patients, treatment of this area is not generally helpful. Frontalis is the only elevator of the upper face (brow, eyebrows, skin of the forehead). Therefore, overtreatment or incorrect targeting can lead to brow ptosis, either real or perceived.
To avoid ptosis, injections too close to the orbital rim should be avoided. Injections should be 2–3 cm above the orbital rim, and doses should be low: 2–4 U onabotulinumtoxinA/incobotulinumtoxinA (6–12 U abobotulinumtoxinA) per injection site and a total of 10–20 U onabotulinumtoxinA/incobotulinumtoxinA (30–60 U abobotulinumtoxinA) (women) or 20–30 U onabotulinumtoxinA/incobotulinumtoxinA (60–90 U abobotulinumtoxinA) (men) total for the forehead (Fig. 21.5). Some injectors target the larger wrinkles, while others target the larger bunched muscle above or below the wrinkle. The exact amount of BoNT, as well as its placement, will be determined by the height of the forehead, the bulk of the muscle and the location of the brow at rest.
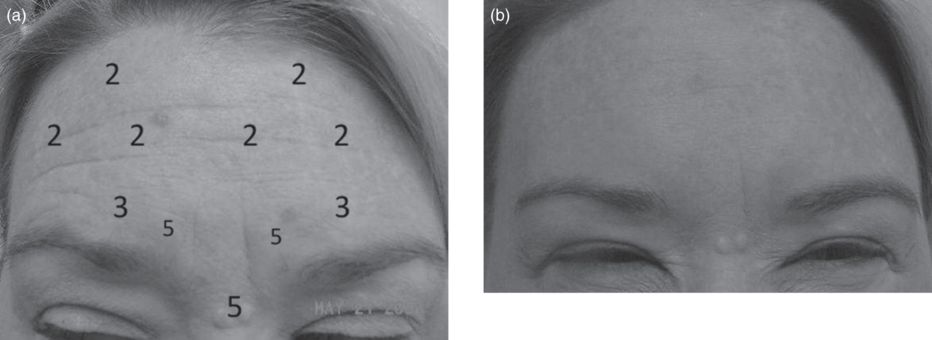
Fig. 21.5 Glabellar complex and forehead. (a) Before injection of 21 U onabotulinumtoxinA/incobotulinumtoxinA into the glabella and 12 U onabotulinumtoxinA/incobotulinumtoxinA into the frontalis. The numbers represent units of onabotulinumtoxinA/incobotulinumtoxinA and the approximate location of the injections. (b) After treatment.
The fibers of frontalis extend laterally to the temple. If not treated adequately, a “Dr. Spock” or “comma” look can develop unilaterally or bilaterally (Fig. 21.6). Fibers of frontalis are paralyzed by 2–4 U onabotulinumtoxinA/incobotulinumtoxinA (6–12 U abobotulinumtoxinA) directed 1–2 cm above the peaked brow. If the superior fibers of frontalis are left intact, wrinkling along the hairline will mar an otherwise smooth forehead; 2 U onabotulinumtoxinA/incobotulinumtoxinA (6 U abobotulinumtoxinA) injected into the active muscle will correct the problem.

Fig. 21.6 Asymmetrically raised eyebrow following forehead injections. An additional injection of 2–3 U onabotulinumtoxinA/incobotulinumtoxinA (6–12 U abobotulinumtoxinA) will return the brow to the desired position.
Eyes
“Crow’s feet” describe the wrinkles at the lateral canthus caused by the contraction of orbicularis oculi and, to a lesser extent, the lip elevators zygomaticus major and minor and risorius. The vertically oriented fibers of orbicularis oculi are the target for BoNT in this region. Injection sites should be above the zygomatic notch to avoid affecting the zygomaticus and risorius muscles, which could cause lip ptosis. Since the fibers of orbicularis oculi are very superficial here, injection is likewise very superficial, just into the subdermal plane. Superficial, somewhat large, vessels are also common in this area; it is prudent to visualize and avoid the vessels in order to reduce bruising. Two to four injection points are often used, with a total of 10–15 U onabotulinumtoxinA/incobotulinumtoxinA (30–45 U abobotulinumtoxinA) injected per canthus (Fig. 21.7). We often use one injection of 8 U onabotulinumtoxinA/incobotulinumtoxinA (24 U abobotulinumtoxinA) at the lateral eyebrow over the zygomaticofrontal suture.
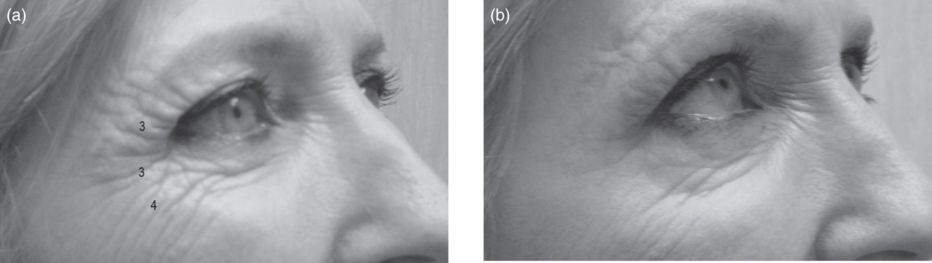
Fig. 21.7 Treatment of crow’s feet. (a) Before treatment with 10 U onabotulinumtoxinA/incobotulinumtoxinA (30 U abobotulinumtoxinA). The numbers represent units of onabotulinumtoxinA/incobotulinumtoxinA used and the approximate location of the injections. (b) After treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


