The Gleason system is based on low-power microscopic assessment (×4 or ×10) of the cancer architecture. The key principle of the grading is based on the use of two most common cancer grades (out of possible 5), primary plus secondary grade , to produce a GS, which theoretically ranges from 2 to 10. When only a single grade is identified, it is doubled to yield a GS. The terms “pattern” and “grade” have also been retained. Typically, pattern is used to describe one or more of the morphologic variations, while grade is used in a more encompassing way, to include all pattern variations within a certain grade.
In clinical practice, the diagnosis of prostate cancer and its management have also evolved over the last few decades, first by introduction of prostate-specific antigen (PSA) testing in the late 1980s, and the extensive use of RP. Prostate cancer incidence has also changed since the introduction of PSA testing, first demonstrating an increase and then a drop; more recently, mortality, primarily in the Western countries, has also decreased [6]. Thus, in current practice, patients are diagnosed earlier, at a younger age, with smaller cancer volumes and lower stage disease [7]. During the last two decades, the practice of thin-needle prostate biopsies (16–18 gauge) has also taken place, first as sextant (six core) biopsies, and then as systematic and extended prostate biopsies, with at least ten tissue cores sampled from different prostate sites (apex, mid, base). The biopsies are also commonly submitted in a site-specific fashion. In contrast, Gleason developed his system on tissue samples from large-bore biopsies (14 gauge) without a site-specific submission, and on transurethral resection of prostate and prostatectomy specimens. In addition, immunohistochemistry was not available in the era when the system was developed, variants of adenocarcinoma and certain morphologic patterns were not recognized, and the significance of the tertiary grade remained uncertain. Around the turn of the century, it also became evident that there are differences in the application of the Gleason system among pathologists (i.e., interobserver variability), particularly in the evolving needle biopsy practice. Pathologists used the Gleason system based on their own understanding, interpretation, or preference. Thus, it was necessary to establish a consensus and to codify the application of the Gleason system to correspond with the clinical practice in the twenty-first century.
International Society of Urologic Pathology 2005 Modification of the Gleason System
In March 2005, a consensus conference was convened by the International Society of Urologic Pathology (ISUP) in San Antonio, TX, USA, in an effort to standardize and unify the use of the Gleason grading system [4]. Specific areas of the original Gleason System reviewed at the 2005 ISUP conference are illustrated in Table 2.1. A “consensus” was defined when two third of the participants were in agreement on certain questions. This effort resulted in the 2005 ISUP modified Gleason system, which, similar to the original Gleason system , outlined the morphologic patterns 1–5 (shown in Table 2.2), which are accompanied by a diagram for the modified Gleason system (shown with the original Gleason system for comparison in Fig. 2.1a, b). The differences between the original Gleason system and the 2005 ISUP modified Gleason system are summarized in Table 2.3 [4, 8]. The 2005 ISUP modified Gleason system reiterated the following points (Table 2.4):
Table 2.1
Specific areas of the original Gleason grading system reviewed at the 2005 International Society of Urological Pathology (ISUP) conference
1 | General applications of the Gleason grading system |
2 | Defining Gleason patterns 1–5 |
3 | Grading variants and variations of acinar adenocarcinoma of the prostate |
4 | Reporting secondary patterns of lower grade when present to a limited extent |
5 | Reporting secondary patterns of higher grade when present to a limited extent |
6 | Tertiary Gleason patterns |
7 | Percentage of patterns 4–5 |
8 | Radical prostatectomy specimens with separate tumor nodules |
9 | Needle biopsies with different cores showing different grades |
Table 2.2
The architectural patterns 1–5 according to the 2005 International Society of Urologic Pathology modified Gleason system
Gleason | |
|---|---|
Pattern | |
1 | Circumscribed nodule of closely packed, but separate, uniform, rounded to oval, medium-sized acini (larger glands than pattern 3) |
2 | Like pattern 1, fairly circumscribed, but at the edge of the tumor nodule, there may be minimal infiltration; glands are more loosely arranged and not quite as uniform as Gleason pattern 1 |
3 | Discrete glandular units, typically smaller glands than seen in Gleason pattern 1 and 2; infiltrates in and amongst nonneoplastic prostate acini; marked variation in size and shape; smoothly circumscribed small cribriform nodules of tumor |
4 | Fused microacinar glands; ill-defined glands with poorly formed glandular lumina; large, cribriform glands; cribriform glands with an irregular border, hypernephromatoid |
5 | Essentially no glandular differentiation, composed of solid sheets, cords, or single cells; comedocarcinoma with central necrosis surrounded by papillary, cribriform, or solid masses |
Table 2.3
Differences between the original Gleason system and the 2005 International Society of Urologic Pathology (ISUP) modified Gleason system
Original Gleason system | 2005 ISUP modified Gleason system |
|---|---|
Diagnosis of GS < 4 can be made on NB | Diagnosis of GS < 4 on NB specimens rarely, if ever, made |
Cribriform glands with rounded and smooth contours as well as cribriform glands with an irregular outer border are diagnosed as Gleason pattern 3 | Most cribriform glands would be diagnosed as Gleason pattern 4. Only rounded, well-circumscribed glands of the same size as normal ones, would be diagnosed as cribriform pattern |
The same GS is used for NB and RP specimens | Different GS are used for NB and RP specimens |
High-grade tumor of small quantity (< 5 %) on NB should be excluded based on GS (5 % threshold rule) | High-grade tumor of any quantity on NB should be included within the GS |
GS on NB based on the primary and the secondary patterns, with an exclusion of the tertiary one | If tertiary pattern is present on NB, GS is based on the primary pattern and the highest pattern |
GS on RP specimens should be assigned based on the primary and secondary patterns (tertiary should not be included or mentioned) | GS on RP specimens is based on the primary and the secondary patterns; if tertiary, higher pattern is present, it is reported separately as a tertiary one |
Separate or overall GS reported for all cores or tissue fragments on NB specimens | When NB specimens show different grades in separate cores, individual GS should be assigned to intact positive cores; overall GS is optional |
The Gleason grade from the largest tumor nodule on RP should be assigned as GS, even if the second larger nodule is of higher grade | When RP specimens show different grades in separate tumor nodules, a separate GS should be assigned to each nodule, irrespective of the size |
Table 2.4
Reporting recommendations for special Gleason grading scenarios
Scenario | Recommendation |
|---|---|
Only one grade present (e.g., GG 3) | Double that grade (assign GS 3 + 3 = 6) |
Abundant high-grade cancer (e.g., GG 4) with < 5 % lower-grade cancer | Ignore the lower-grade cancer (assign GS 4 + 4 = 8) |
Small focus with mostly GG 4 and few glands of GG 3 | If GG 3 occupies > 5 %, include lower-grade cancer (assign GS 4 + 3 = 7) |
Abundant GG 3 with any extent of GG 4 | Include the higher grade (assign GS 3 + 4 = 7) |
Three grades (e.g., GG 3, 4, and 5) present | Classify as high grade (assign most common plus highest grade) |
NB: multiple cores showing different grades—cores submitted separately and/or with designated location | Assign separate GS to each core |
NB: multiple cores showing different grades—all cores were submitted in one container or cores are fragmented | Assign overall GS for the specimen |
a.
GS represents the sum of the primary (most predominant) Gleason grade and the secondary (second most predominant) Gleason grade. However, in needle biopsies, this principle was modified to include any component of higher grade than the second most predominant grade as the secondary grade. Thus, on needle biopsy the GS is derived based on the primary and the highest (worst) grade.
b.
The reporting of the grade should be accompanied by using the words “pattern” or “grade,” and it is therefore not acceptable to report only “Gleason 3” because it is unclear whether this represents grade (pattern) or score.
c.
GS 1 + 1 = 2 on needle biopsy should rarely, if ever, be reported and should be carefully considered in practice, in any type of specimen. These cancers are extraordinarily rare in needle biopsies, although they can be infrequently seen in transurethral or RP specimens. There is a poor reproducibility even among experts in grading lower-grade tumors. Cancers that are assigned GS 2–4 on needle biopsy correlate poorly with RP GS and these “low” scores may misguide clinicians and misinform patients into considering these tumors as indolent.
d.
Individual cells are not part of Gleason pattern 3.
e.
Most cribriform glands are diagnosed as Gleason pattern 4. Only rare cribriform glands satisfy the stringent diagnostic criteria required for the diagnosis of cribriform pattern 3: rounded, well-circumscribed glands of the same size as the normal glands.
f.
Morphologic variants of acinar adenocarcinoma, such as pseudohyperplastic and foamy adenocarcinoma, should be graded on the basis of the underlying architecture.
g.
A secondary pattern of lower-grade cancer, when it occupies less than 5 % of tumor, should be ignored and not reported as part of the GS, both on needle biopsy and RP.
h.
High-grade tumor of any quantity, even when occupying less than 5 % of the tumor, should always be included and reported within the GS on needle biopsy.
i.
When a tertiary Gleason pattern is present, GS on biopsy should be derived by adding the primary and the highest (worst) pattern, whereas on RP, the tertiary pattern (the least common pattern), should be reported separately if it is of higher grade than the primary and the secondary patterns.
j.
When separate tumor nodules with different Gleason patterns are encountered on RP, they should be scored and reported separately.
k.
It remains optional to include the actual percentage of Gleason patterns 4 or 5 in a report.
l.
For needle biopsies containing different cores with different cancer grades, separate GS should be assigned for individual positive cores, if they are submitted in separate containers or if the cores are in the same container, but have a designated location (for example, if marked by different ink color). An optional, overall GS can be provided at the end of the case for all positive biopsy cores. The overall (global) GS follows the general rule of primary (most predominant) Gleason grade and secondary (second most predominant) Gleason grade [9, 10]. When a container has multiple fragmented cores and it is unclear whether they represent intact cores or multiple cores, an overall score should be provided for all fragments in the container.
Changes and Trends in Practice in Interpreting Gleason Grades 1–5 After the 2005 ISUP Consensus Conference
The 2005 ISUP modified Gleason system was widely promoted and embraced in routine practice after the consensus conference and the subsequent publication, although certain issues remained unresolved. The main trends and changes in the use of individual grades in pathology practice after 2005 were as follows:
Gleason Grade 1
Since the 2005 ISUP consensus conference concluded that Gleason grade 1 tumors should be diagnosed “rarely, if ever,” the use of pattern 1 after 2005 became vanishingly rare. Many uropathology experts maintain that pattern 1 in the original Gleason system likely represented adenosis (atypical adenomatous hyperplasia), a now well-recognized cancer mimicker. At that time, however, immunohistochemistry was not available and thus, adenosis may account for the great majority of cases considered traditionally as Gleason pattern 1. Many of the infrequently published images of Gleason pattern 1 can be critically questioned and accordingly it has been proposed that Gleason pattern 1 is completely abandoned in practice [11].
Gleason Grade 2
Similarly, the appropriateness of using pattern 2 in needle biopsies has also been questioned and pathologists have been advised not to use it in grading cancer on needle biopsies [12]. Cancers assigned GS 2–4 on needle biopsy correlate poorly with GS on RP, which almost always contain higher-grade cancer. Pattern 2 can be seen occasionally in transurethral resection and RP specimens, usually as part of multifocal cancer invariably showing a higher-grade component.
Gleason Grade 3
The general focus of the 2005 modifications pertained primarily to the most prevalent patterns 3 and 4. The 2005 ISUP modified Gleason system restricted the definitions of pattern 3 and broadened the spectrum of pattern 4 cancer [8, 13, 14]. As in the original Gleason system, pattern 3 in the 2005 ISUP modified Gleason system includes discrete well-formed individual glands, infiltrating in and among nonneoplastic prostate acini (Fig. 2.2a). Very small, well-formed glands are still considered Gleason pattern 3; however, in contrast to the original Gleason system , “individual cells” are not. The definition of grade 3, however, also stipulates “marked variation in glandular size and shape,” which, unfortunately, was not well depicted in the 2005 diagram. It is still unclear, for example, which variations in glandular shape should be considered Gleason pattern 3 (Fig. 2.2b). Are individual glands showing branching and forming, for example, X, V, T, and Y glandular shapes (not illustrated in the 2005 diagram) still consistent with pattern 3 or do they represent pattern 4? Indeed, many uropathologists would consider these common morphologies to represent pattern 3, but unfortunately this cannot be reconciled using the 2005 ISUP Gleason diagram .
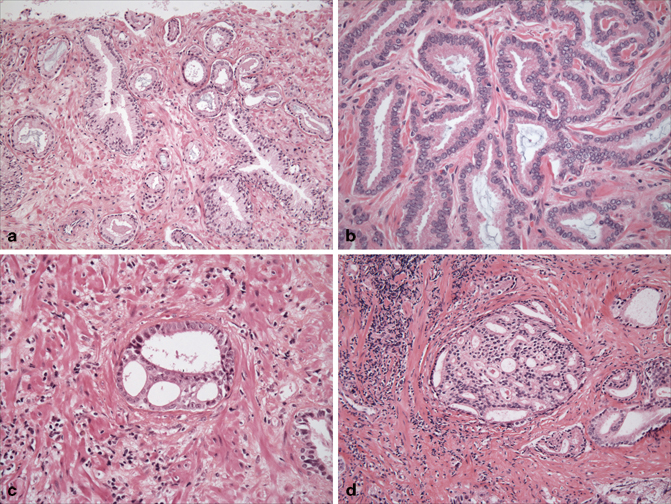
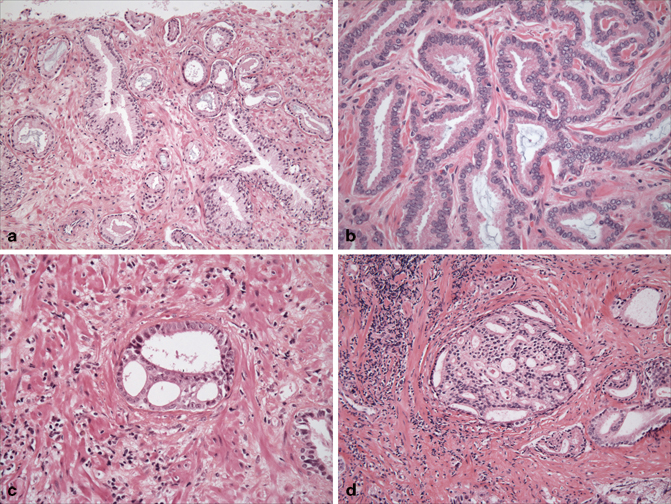
Fig. 2.2
Gleason grade 3 includes discrete infiltrative glands with well-formed lumina (a). Individual glands showing some modifications of size and shape such as branching (not illustrated in the 2005 diagram) are still interpreted as pattern 3, although some may interpret them as pattern 4 (b). Cribriform rounded, well-circumscribed glands of the same size as the normal glands are interpreted as pattern 3 (c). If they are with similar cribriform features but of larger size than a normal gland, they are currently interpreted as pattern 4. Using the original Gleason system, these would have been graded as pattern 3 (d)
More stringent criteria were established by the 2005 ISUP consensus conference concerning cribriform pattern 3 glands. Only rounded, well-circumscribed glands of the same size as the normal glands, with evenly spaced lumina and cellular bridges (Fig. 2.2c) are included as cribriform Gleason pattern 3. In essence, these types of cancers should morphologically resemble cribriform high-grade prostatic intraepithelial neoplasia (HGPIN), but lack basal cells. This definition was in contrast to the original Gleason illustrations of cribriform pattern 3, which included large, cribriform glands with rounded and smooth contours, exceeding the size of the normal glands (Fig. 2.2d). In the current practice, nearly all cribriform glands are being diagnosed as pattern 4 [13].
Gleason Grade 4
The scope of Gleason pattern 4 in the 2005 ISUP modified Gleason system was widened. A consensus was reached that ill-defined glands with poorly formed lumina, a pattern often seen in fused glandular structures, should also be included under Gleason pattern 4. This novel category was not described in the original Gleason system.
Therefore, pattern 4 now includes: (a) fused microacinar glands; (b) ill-defined glands with poorly formed glandular lumina; (c) large, cribriform glands and cribriform glands with an irregular border, and (d) hypernephromatoid glands:
a.
Fused glandular morphology implies that discrete glandular units are lost or are unrecognizable (unchanged from the original Gleason system) (Fig. 2.3a).
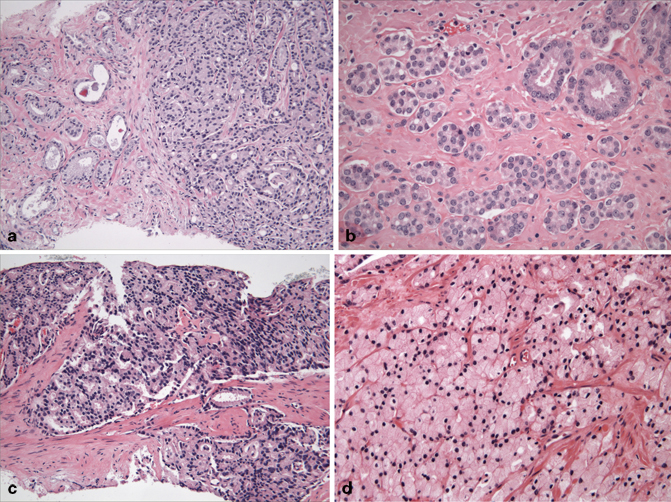
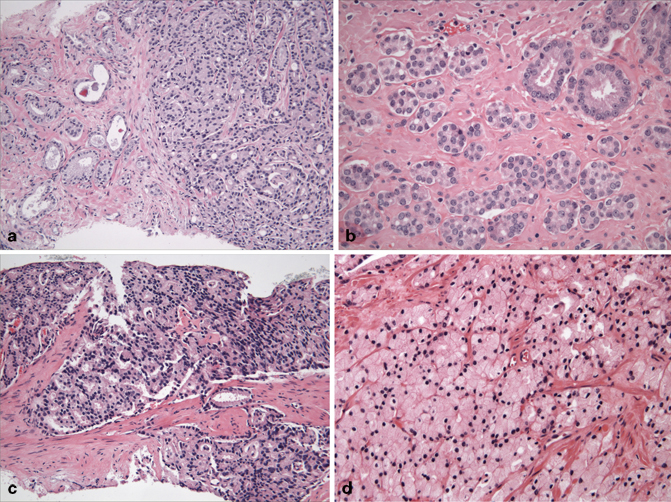
Fig. 2.3
Gleason grade 4 includes glands that are fused (represented on the right; contrast them with the individual glands on the left) (a), glands with ill-formed lumina (contrast them with a couple of individual glands with well-formed lumina in the upper right) (b), large cribriform glands (c), and hypernephromatoid glands (d)
b.
Ill-defined glands with poorly formed glandular lumina, a novel category, is now considered pattern 4 (Fig. 2.3b). The illustrations of this pattern remained sketchy and unclear in the literature, thus creating some confusion and leading to relatively open interpretation of this concept. Distinguishing, for example, between poorly formed glands (pattern 4) and tangentially sectioned glands (pattern 3) seems to be one of the most problematic issues of the current Gleason grading . This essentially requires two-dimensional interpretation of a three-dimensional complex glandular morphology, which can be subjective.
c.
Cribriform glands, as previously outlined, are nearly uniformly diagnosed as Gleason pattern 4 in current practice, independently of the glandular contour (Fig. 2.3c). In a recent study, poor reproducibility was reported among urologic pathologists in defining Gleason pattern 3 cribriform glands; in addition, in 73 % of the cases there was a coexistent Gleason pattern 4 tumor [15]. Therefore, a proposal has been made by Epstein to alter the 2005 ISUP diagram and to delete the cribriform 3 morphology [13, 14].
d.
Hypernephromatoid, an infrequent glandular morphology of fused glands with clear or pale cytoplasm was retained as pattern 4 (Fig. 2.3d) (unchanged from the original Gleason system).
Gleason Grade 5
Pattern 5 remains almost unchanged from the original Gleason system and indicates absence of glandular differentiation, with neoplastic cells forming solid sheets, cords, or single cells (Fig. 2.4a, b). The presence of cords also includes single file cell formation. Solid nests, i.e., solid structures smaller than a “sheet” may potentially pose some problems, as smaller solid units may be interpreted as glands with ill-defined lumina (pattern 4). Comedocarcinoma with central necrosis surrounded by papillary , cribriform, or solid glands also represents pattern 5 (Fig. 2.4c, d).
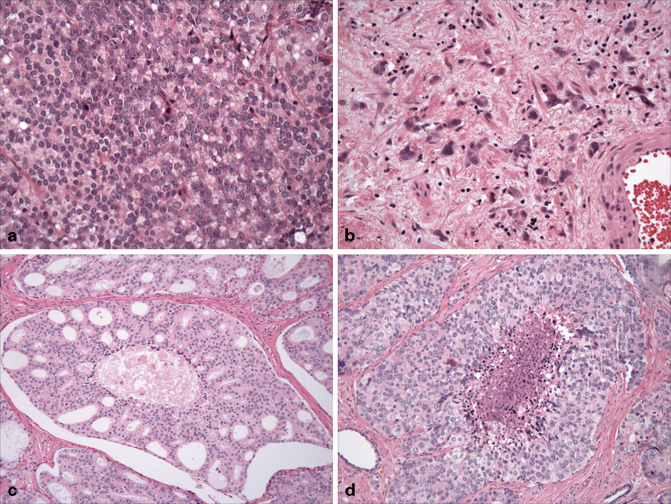
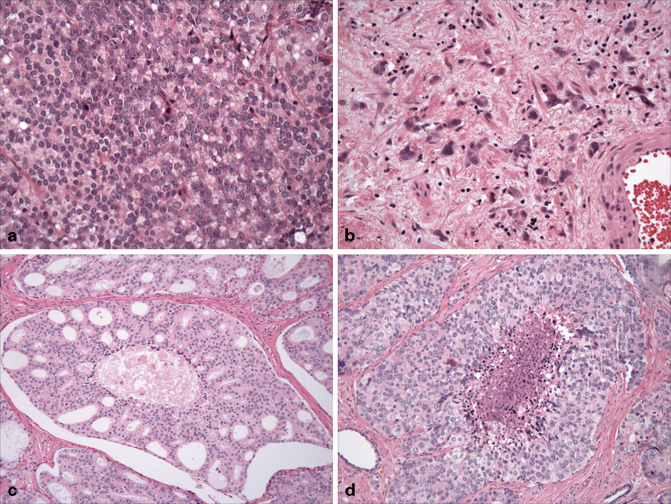
Fig. 2.4
Gleason grade 5 includes sheets of cells (a), single cells and single file cords (b), glands containing comedo-type necrosis surrounded by either cribriform (c), or solid masses (d)
Grading Variants of Prostate Adenocarcinoma in Contemporary Practice
Grading of different variants of prostatic adenocarcinoma is shown in Table 2.5 and illustrated in Fig. 2.5a–g) :
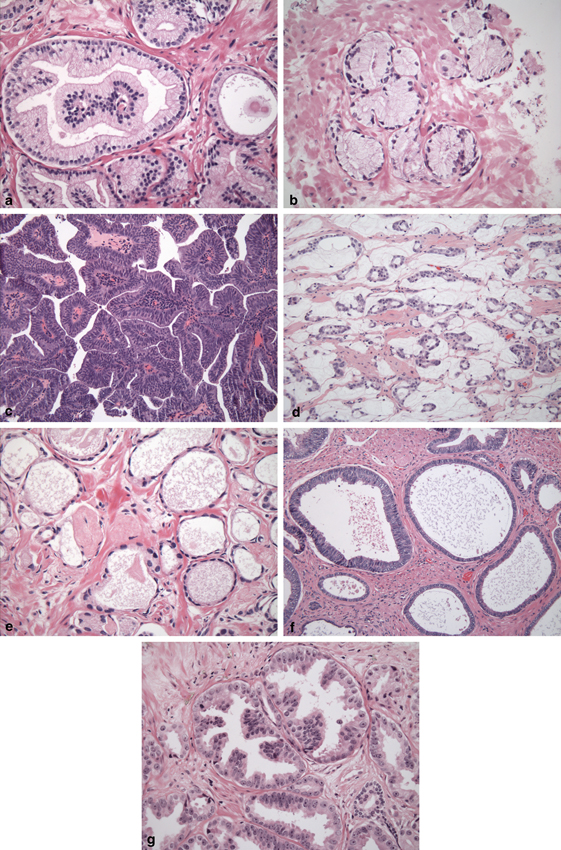
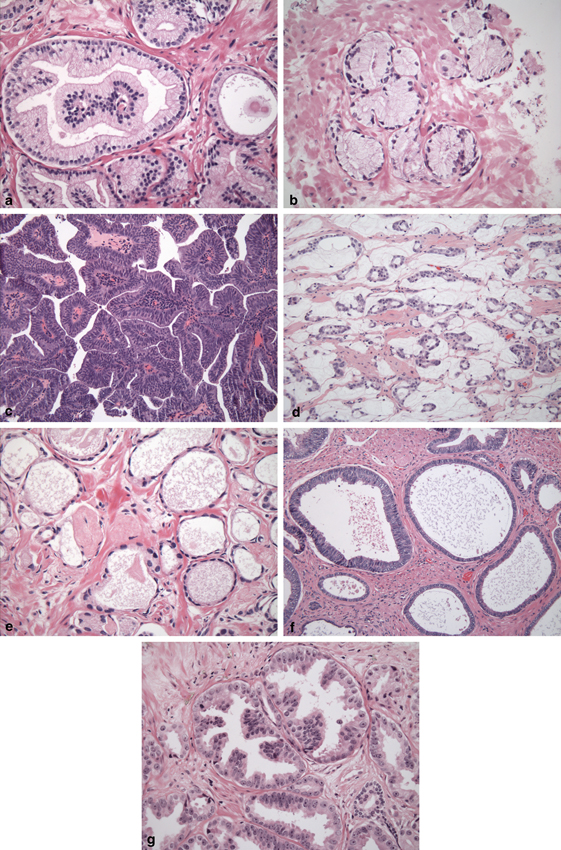
Fig. 2.5
Variants of prostatic carcinoma. Pseudohyperplastic carcinoma should be graded as pattern 3 (a). Foamy (or xanthomatous) carcinoma should be graded as pattern 4 if composed of individual glands (b) or pattern 4 if composed of fused or cribriform glands. Ductal adenocarcinoma is graded as pattern 4 (c); if comedonecrosis is present, it is graded as pattern 5. Colloid (mucinous) adenocarcinoma is graded as pattern 3 if individual discrete glands are floating within mucin (d) or pattern 4 if they appear irregular cribriform or fused (as rare glands on the image). Atrophic cancer is graded as pattern 3; note a collagenous micronodule slightly off to the left of the center (e); cystic and microcystic cancers are also graded as pattern 3 (f). PIN-like adenocarcinoma is graded as pattern 3 (g); if there is glandular fusion, it is graded as pattern 4
Table 2.5
Grading recommendations for prostate adenocarcinoma variants
Variant | Gleason grade |
|---|---|
Pseudohyperplastic | 3 |
Foamy | 3 or 4 (depending on architecture) |
Ductal | 4 or 5 (if comedonecrosis present) |
Mucinous (colloid) | 3 or 4 (extract mucin/grade architecture) |
Atrophic-cystic | 3 |
PIN-like | 3 (rarely 4) |
Small cell (neuroendocrine) | Not graded |
Squamous or adenosquamous | Not graded |
Urothelial carcinomas | Not graded |
Basaloid or adenoid-cystic | Not graded |
Sarcomatoid | Not graded (same grade as 5, glandular component graded separately) |
Pseudohyperplastic Adenocarcinoma
Cancers with pseudohyperplastic features (large individual glands resembling normal glands, but containing cytologically malignant nuclei), should be graded as Gleason grade 3, in large part based on the recognition that they are most often accompanied by more usual Gleason grade 3 adenocarcinoma (Fig. 2.5a) .
Foamy Gland Carcinoma
Although most cases of foamy (or xanthomatous) gland carcinoma would be graded as Gleason grade 3 (Fig. 2.5b), they can also show a higher-grade pattern and should be graded accordingly, usually as Gleason pattern 4.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


