Congenital Lesions: Thyroglossal Duct Cysts, Branchial Cleft Anomalies, and Cystic Hygromas
Michael A. Skinner
Congenital anomalies of the neck are manifested clinically as either a subcutaneous nodule or a mass lesion, a skin pit, or a draining sinus. The most common abnormalities resulting from errors in the embryologic development of structures in the head and neck include thyroglossal duct cyst, branchial cleft remnant, and lymphatic malformations. The surgical management of these abnormalities is aimed at complete resection and preventing infections.
Thyroglossal Duct Cyst
Embryology and Anatomy
The thyroglossal duct is a remnant structure resulting from the downward descent of the median thyroid anlage during the 3rd week of gestation. The structure courses inferiorly in the neck from the base of the developing tongue to fuse with the lateral thyroid anlage. During descent, the structure passes through or near the developing hyoid bone, which is an important feature in definitive surgical management. During weeks 5 to 8 of gestation, the thyroglossal duct normally obliterates, leaving only the foramen cecum at the base of the tongue. However, in some cases, there is the residual thyroglossal duct extending inferiorly into the neck (Fig. 1). The structure is lined with secretory epithelium that is activated for unknown reasons to cause the development of a cyst.
Clinical Presentation and Evaluation
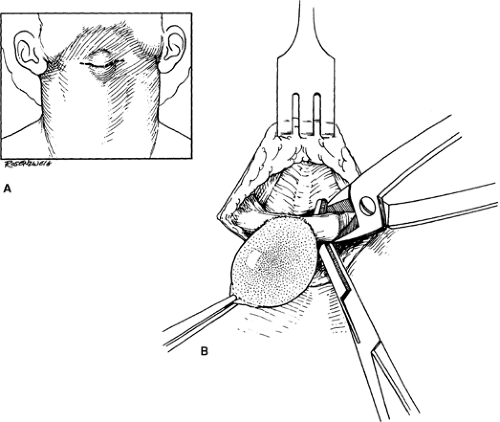
More than half of all thyroglossal duct cysts are diagnosed within the first 10 years of life. The lesions typically present as a painless, asymptomatic cystic nodule in the midline of the neck (Fig. 2). At times, they may be located off the midline by 1 to 2 cm. The lesion is typically inferior to the hyoid bone, and moves with swallowing. The differential diagnosis includes dermoid cyst, enlarged midline lymph node, teratoma, and ectopic thyroid tissue. Owing to its communication with the base of the tongue, thyroglossal duct cysts may initially manifest with the typical signs of infection including swelling, redness, and pain.
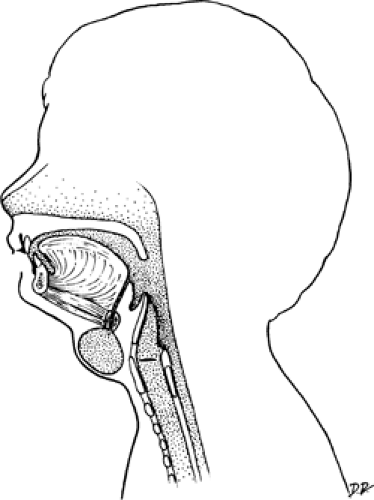 Fig. 2. Thyroglossal duct cyst anterior to the hyoid bone with the thyroglossal duct tract passing through the hyoid bone and extending to the foramen cecum. |
The diagnosis can usually be established from the history and physical examination. It is most important to exclude the presence of remnant ectopic thyroid, which may be the only source of thyroid hormone for the patient. If the presence of a normal thyroid gland can be established on physical examination, no other evaluation is necessary. However, it is usually appropriate to go for an ultrasound study to confirm the presence of normal thyroid gland. It is usually not necessary to obtain a thyroid scintigraphic scan.
Surgical Management and Outcome
When the initial presentation is one of infection, management should consist of needle aspiration of the cyst contents and administration of antibiotics selected to control oral flora. If possible, formal incision and drainage should be avoided since this will complicate definitive surgical treatment. It should be noted that thyroglossal ducts initially presenting with an infection are associated with increased incidence of recurrence after surgical resection. Elective removal of an infected lesion should be performed 6 to 8 weeks after resolution of the acute infection.
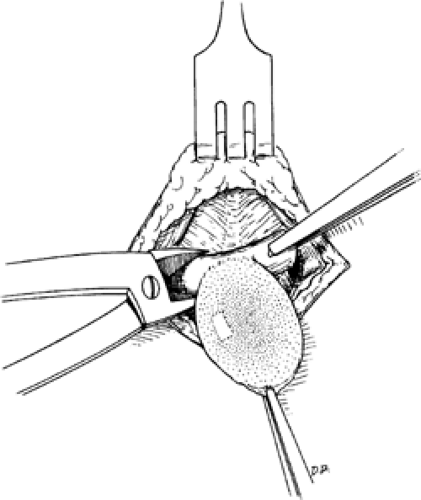
In the uncomplicated case, elective surgical resection with the Sistrunk procedure has been shown to be effective, with a recurrence risk of about 2% to 5%. The procedure can usually be done on an outpatient basis. The patient should be placed in the supine position, with the neck extended. Preoperative antibiotics to cover skin and oral flora should be administered. A transverse incision is made over the palpable cyst, and the cyst is mobilized from the surrounding structures using electrocautery (Fig. 3). The surgeon should resist the temptation to dissect too closely to the duct, as it progresses posteriorly and superiorly to the hyoid bone. Rather, a generous amount of surrounding tissue should be taken in the dissection up to the hyoid bone, to reduce the likelihood of missed accessory ducts with consequent recurrence. Inability to clearly identify a duct extending to the hyoid bone suggests that the diagnosis is a dermoid cyst rather than a thyroglossal duct cyst; these lesions cannot usually be distinguished on preoperative ultrasound study. Electrocautery can be used to divide the muscle inferior and superior on the hyoid bone, and bone cutter can be used to remove a 1- to 1.5-cm section of the hyoid bone (Fig. 4). In younger patients, when the bone is incompletely ossified, the hyoid can be divided using electrocautery. Then, dissection continues posteriorly and superiorly to the base of the time, again leaving a generous amount of tissue around the duct (Fig. 5). Suture ligation and division of the duct at the base of the tongue is then accomplished, and the specimen removed (Fig. 6). In some cases, a gloved hand can be inserted in the mouth to assess progress of the dissection to the base of the tongue. The wound can be closed in layers of absorbable suture. Routine placement of a drain is unnecessary.
The most serious complication is the exceedingly rare incidence of hemorrhage with airway impingement. This can be avoided by careful hemostatic dissection during the operation. Recurrence of thyroglossal duct cyst occurs in 2% to 5% of cases; this usually becomes evident within 1 year of initial resection. These recurrences typically present
with inflammation and infection in the anterior neck; there may be recurrent drainage from the incision site. The recurrence rate is increased in patients who have had a previous infection prior to surgery, or if an insufficient amount of the hyoid bone has been removed. To manage such recurrences, antibiotics should be administered until significant inflammation resolves, and then reoperation must be performed. To prevent another recurrence, reoperation should be performed with an elliptical incision around the previous incision, and removal of inflamed tissue with a generous hyoid bone resection, and wide excision of the midline and geniohyoid muscle.
with inflammation and infection in the anterior neck; there may be recurrent drainage from the incision site. The recurrence rate is increased in patients who have had a previous infection prior to surgery, or if an insufficient amount of the hyoid bone has been removed. To manage such recurrences, antibiotics should be administered until significant inflammation resolves, and then reoperation must be performed. To prevent another recurrence, reoperation should be performed with an elliptical incision around the previous incision, and removal of inflamed tissue with a generous hyoid bone resection, and wide excision of the midline and geniohyoid muscle.
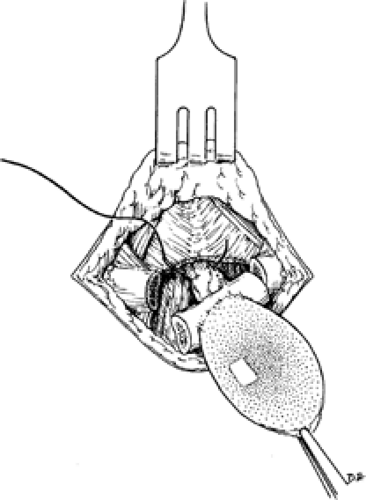 Fig. 5. Dissection proceeds cephalad to the foramen cecum where the tract and investing tissues are suture-ligated. |
Branchial Cleft Anomalies
Embryology and Anatomy
The structures of the face and neck arise from the fourth embryonic pharyngeal or branchial arches, appearing in the 4th and 5th weeks of embryonic development. They consist of bars of mesenchymal tissue separated by deep clefts, known as pharyngeal clefts. This process resembles the development of gills in fish; however, since humans do not possess gills (branchia), it is more correct to use the term “pharyngeal” rather than “branchial” in describing the arches, clefts, and pouches in the human embryo.
What are commonly called branchial anomalies consist of cysts, sinuses, or congenital cartilaginous remnants resulting from
errors in development of the embryonic pharyngeal apparatus. Such lesions represent about 30% of congenital neck masses. It is somewhat misleading to call these branchial cleft anomalies, since in actuality these abnormalities have contributions from branchial clefts, arches, or pouches. When a pharyngeal arch exhibits incomplete obliteration, and communicates with either the skin or mucosa, a sinus results. If there is failure of both the cleft and the pouch to obliterate, there will be a continuous communication between the mucosa and the skin, resulting in a branchial fistula. Finally, when a pharyngeal cleft remnant forms an epidermis-lined cavity without other communication, a cyst will result.
errors in development of the embryonic pharyngeal apparatus. Such lesions represent about 30% of congenital neck masses. It is somewhat misleading to call these branchial cleft anomalies, since in actuality these abnormalities have contributions from branchial clefts, arches, or pouches. When a pharyngeal arch exhibits incomplete obliteration, and communicates with either the skin or mucosa, a sinus results. If there is failure of both the cleft and the pouch to obliterate, there will be a continuous communication between the mucosa and the skin, resulting in a branchial fistula. Finally, when a pharyngeal cleft remnant forms an epidermis-lined cavity without other communication, a cyst will result.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree