Learning Outcomes
After completing this chapter, you will be able to
 Describe the purpose of various types of communications that occur within pharmacy practice settings, including the role of the pharmacy technician.
Describe the purpose of various types of communications that occur within pharmacy practice settings, including the role of the pharmacy technician.
 Distinguish between questions that may be answered by a technician and those that should be answered only by a pharmacist
Distinguish between questions that may be answered by a technician and those that should be answered only by a pharmacist
 List the basic elements of verbal and nonverbal communications.
List the basic elements of verbal and nonverbal communications.
 Given a specific patient encounter scenario, compare and contrast effective and ineffective communication skills.
Given a specific patient encounter scenario, compare and contrast effective and ineffective communication skills.
 Describe how to vary communication techniques to improve success when working with special patient populations.
Describe how to vary communication techniques to improve success when working with special patient populations.
 Identify the types of health care professionals with whom a pharmacy technician may communicate, as well as effective strategies for those communications.
Identify the types of health care professionals with whom a pharmacy technician may communicate, as well as effective strategies for those communications.
 Describe the types of behaviors that should be demonstrated by pharmacy technicians to promote effective working relationships with other health care team members.
Describe the types of behaviors that should be demonstrated by pharmacy technicians to promote effective working relationships with other health care team members.
Key Terms
| body language | Body movements or mannerisms that can be interpreted as conveying one’s feelings or psychological state of mind |
| closed-ended questions | Questions that can be answered by a simple “yes” or “no.” |
| communication | The transfer of information, knowledge, facts, wishes, or emotions from one source to another |
| empathy | A sharing of or identification with another’s feelings or state of mind without actually going through the same experience; the ability to view feelings from the patient’s perspective, communicating acceptance or understanding. |
The Role of the Pharmacy Technician on the Patient Care Team
The Importance of Effective Communication Skills
Effective Communication Skills
The Basic Elements of Communication
Communication Strategies for Special Patient Populations
Communicating with Other Health Care Professionals |
|
While performing their daily job responsibilities, pharmacy technicians must interact and communicate with many individuals. To facilitate successful communication, effective relationships must be established with patients, consumers, pharmacists, fellow technicians, and other health care professionals. Thus, it is important for pharmacy technicians to develop effective communication skills in order to help strengthen professional relationships and to ensure appropriate information exchange. These skills will help the pharmacy technician better assist the pharmacist in providing patient-centered care and managing pharmacy operations.
The purpose of this chapter is to help the pharmacy technician develop effective communication skills to enhance his or her value as a member of the pharmacy patient care team.
The Role of the Pharmacy Technician on the Patient Care Team
As pharmacists have expanded their roles in the provision of patient-centered care, the roles of pharmacy technicians have concurrently evolved. A pharmacy technician is defined as “[an] individual working in a pharmacy who, under the supervision of a licensed pharmacist, assists in pharmacy activities that do not require the professional judgment of a pharmacist.”1 As integral members of the pharmacy care team, pharmacy technicians work together with pharmacists to help ensure optimal and safe use of medications by patients and to help promote successful health outcomes.2 This is accomplished through a synergistic application of knowledge, skills, abilities, and responsibilities. As described in Chapter 1, pharmacy technicians help the pharmacist with prescription preparation and distribution, with maintaining medication inventories, and with managing and administering pharmacy operations, and they also serve in other vital capacities within various pharmacy practice settings. These roles and responsibilities are not limited to interactions with pharmacists and other pharmacy technicians but also include other health care professionals and patients/caregivers as recipients of the health care–related services provided.
Whether pharmacy technicians are engaged in traditional roles or in more contemporary ones, the use of effective communication skills can play a major role in furthering successful versus unsuccessful encounters and greatly affect their related outcomes.
The Importance of Effective Communication Skills
Effective communication skills are essential if pharmacy technicians are to sustain successful interactions within the scope of their responsibilities. Strong communication skills help avoid misunderstandings and interpersonal conflicts and play a major role in ensuring patient safety. Miscommunications could also result in problems related to inventory control, financial and legal liability, licensure maintenance, breakdowns in organizational relationships, and potential loss of employment, so it is imperative that the value of effective communication by all members of the pharmacy patient care team be realized.
 Effective communication strategies can help to prevent medication errors and improve the quality of patient care.
Effective communication strategies can help to prevent medication errors and improve the quality of patient care.
Effective Communication Skills
Communication occurs when one individual conveys information to another individual or group of individuals. The goal of effective communication is to ensure that the recipient party hears the same message, both in content and intent, as the deliverer, and that the intended result of that message is achieved. However, because there may be situations when the best communication efforts don’t yield the intended result, it is important to develop strategies for identifying when this occurs.
The other important aspect of communication is listening. If the recipient of the message does not give the individual who is conveying information his or her full attention, he or she may misunderstand the message or fail to hear it in its entirety. Even under the best of circumstances, many things can go wrong with the communication process, in part because each individual processes information in his or her own unique way. The information is received and, in combination with the circumstances surrounding the reasons for the encounter, the recipient of the message draws his or her own conclusions. Consider the following scenario:
A patient arrives at the pharmacy counter with a new prescription. After handing the prescription to the pharmacy technician, the patient is informed that the prescription will not be ready for at least an hour. The patient responds, “That’s ridiculous! It can’t take that long to take a few pills from a container and put them in a bottle. I want my prescription filled right now, or I’m taking it to another pharmacy where people know what they are doing!”
How should the pharmacy technician respond to this patient? How has the technician delivered the message about the prescription waiting time? How has the patient received the message given? What other factors need to be considered in this encounter? Specific information has been shared, but there is probably much information that has not been communicated that could play a significant role in the outcome of this encounter. In fact, each individual’s views in these types of circumstances are based on different information. To improve communication, these different perspectives will be further explored.
The Patient’s Perspective A patient is an individual who is receiving medical or health treatment. Regardless of the pharmacy practice setting, patients come into contact with pharmacists and pharmacy technicians in association with seeking or receiving health care–related services or information. Patients do not want to be viewed as objects, but rather as individuals who need the services that are being provided. A patient’s underlying feelings and concerns about health conditions can produce behaviors that are challenging to deal with. Examples of health-related personal issues that patients may experience are listed in box 8–1.
Regardless of outward behaviors, patients need to feel that care and understanding is being extended to them. Even in circumstances when the correct words are spoken, unintentional confrontations can occur when underlying issues are present. This may be especially true when patients are facing acute illness, hospitalization, or other potentially debilitating circumstances. Viewing patients as objects instead of individuals with legitimate needs can get in the way of delivering patient-centered care (described below) by causing providers to mentally assign negative value to them (e.g., as unworthy, irrelevant, or unimportant).3–4 It is important to show an active interest in the patient’s concerns, to be attentive to emotional signals, to listen well, to exhibit sensitivity, to anticipate needs, and to meet expectations.5 In addition, professional behavior should be exhibited by the health care professional at all times. Anything less will prevent high-quality care from being given.
In the scenario above, what was the patient’s view of the circumstances? The patient had given the technician a new prescription. The medication could have been prescribed for an acute or new chronic health problem that is causing major stress for the patient. In addition, the patient could have been influenced by past experiences encountered at a pharmacy. Collectively, these feelings may have produced an unwelcome emotional response that was then directed at the pharmacy technician. In the patient’s view, the length of time to fill the prescription was potentially connected to the level of competence of the pharmacist and pharmacy services being provided. The patient lacks more specific information about the circumstances necessitating the waiting time for the prescription. Was there more specific information that the pharmacy technician could have shared to address the situation? Were there additional questions the pharmacy technician could have asked the patient to help clarify the patient’s concerns? If so, how could these things have been accomplished to improve communication and increase the likelihood that the patient would allow the prescription to be filled—and return in the future for additional medications?
Box 8–1. Patient Perspective: Examples of Health-Related Personal Issues
| Anger | Compromised coping skills | Grief | Loss of power |
| Anxiety | Denial | Health care insurance | Mental changes |
| Concern about body changes | Fear | Isolation | Social support availability |
| Concern about possible death | Financial worries | Loss | Spirituality |
The Pharmacist’s Perspective. Pharmacists are involved in providing patient-centered care, previously referred to as “pharmaceutical care.” As defined, it is the “responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life.”6 Patientcentered care focuses on the patient’s role and responsibility in his or her medication-taking and health-related behaviors. The pharmacist is responsible for ensuring that the patient will not be harmed by any given medication and for verifying that the patient understands how the medication should be used in order to prevent harm and achieve therapeutic goals. To achieve these goals, an important requirement is that the pharmacist must be able to develop the needed relationships with the patient and other health care professionals to provide the specified care.
It is important for patients to feel that health professionals care for them and are willing to address their needs. Pharmacists can accomplish this by communicating with patients in a manner that expresses and demonstrates a caring attitude in the degree, the method, and the expertise of the response. Of course, pharmacists cannot make patients take medication properly, but they can create supportive conditions under which patients can be encouraged to be successful.
But pharmacists are human beings just as patients are, and pharmacists do not want to be viewed as objects any more than the patients do. Pharmacists can struggle with their own personal lives. Pharmacy practice settings can be very stressful, and not all patient-related encounters are friendly or enjoyable. However, health care providers are expected to manage personal feelings while recognizing and considering the feelings of their patients. High-quality service is provided when better understanding of patient needs and feelings are achieved. When the goals of communication are clear, they help shape the responses—and, ultimately, the outcomes—of the encounters. The pharmacist does not carry these responsibilities alone. All members of the pharmacy team are accountable to the patient.
The Pharmacy Technician’s Perspective. Pharmacy technicians also play an important role in the patient’s safe use of medications and positive medication-related outcomes. This encounter may be in person, by telephone, or by another communication means. The first impression that the individual will have of the pharmacy and its staff and services may be the one provided by the technician. Thus, the importance of professionalism— appropriate appearance, behavior, knowledge, and responses—in a technician cannot be overemphasized. For example, if the pharmacy technician greets the patient by his or her first name instead of more formally without being asked to do so, this may be viewed by the patient as disrespectful. If the technician is engaging in a personal mobile phone call that causes an inappropriate wait for the patient, this could be viewed as unprofessional or disrespectful. Furthermore, inattention to personal hygiene, the wearing of inappropriate apparel (e.g., low-cut blouses or torn pants), the lack of a visible professional identification badge, and use of foul language, a loud voice, or belittling tones can undermine the relationships between patients and pharmacy personnel.
 Often, the pharmacy technician is the first person the patient (and, in some cases, other health care providers) encounter in the pharmacy setting.
Often, the pharmacy technician is the first person the patient (and, in some cases, other health care providers) encounter in the pharmacy setting.
RX for Success
Professional behavior should be exhibited by the pharmacy technician at all times to ensure the provision of high-quality patient care.
Returning to our scenario: the pharmacy technician had information impacting the wait time of which the patient was unaware (e.g., the number of prescriptions awaiting processing, the number of telephone calls being received, personnel availability issues, employee personal problems, and so forth). Raising the patient’s awareness of these situations may not be easy, practical, or appropriate. Emotionally charged circumstances can be stressful and challenging and may feel somewhat threatening. Just like the pharmacist, the pharmacy technician may not have control over the circumstances facing the patient, but the technician’s response to those circumstances is very much under his or her control. Remember that when the goals of the communications are clear, they help shape the responses—and, ultimately, the outcomes—of the encounters. The priority should be the well-being of the patient.
Using the previous scenario, how could the pharmacy technician have answered the patient to address the stated concern?
A patient arrives at the pharmacy counter with a new prescription. After handing the prescription to the pharmacy technician, the patient is informed that the prescription will not be ready for at least an hour. The patient responds, “That’s ridiculous! It can’t take that long to take a few pills from a container and put them in a bottle. I want my prescription filled right now, or I’m taking it to another pharmacy where people know what they are doing!”
“I can appreciate your concern about the waiting time. It may seem somewhat excessive. There have been several patients who arrived before you with complicated medication needs requiring discussions with their health care providers. Our goal is to ensure that every patient receives individualized care from our pharmacists, so it may take a little longer to complete a prescription than you may be used to. But please be assured that we value you as our patient and want to ensure that your medication and health care needs are met as safely and efficiently as possible. Maintaining our patients’ good health is our first concern!”
Later in the chapter, we will revisit this scenario again and use specific concepts of effective communication to address the patient’s concerns.
The Basic Elements of Communication
Interpersonal communication involves a complex array of processes focused on transmitting, receiving, and processing (or interpreting) information. This section will address the areas of verbal, nonverbal, and written interpersonal communication.
Verbal Communication. Verbal communication is the most common form of interpersonal communication. It involves a spoken message delivered from a sender to a recipient.
 One of the most important things to remember about verbal communication is that “once it has been said, it can’t be taken back.”
One of the most important things to remember about verbal communication is that “once it has been said, it can’t be taken back.”
For successful encounters, this key fact should never be forgotten and should always guide the communication. There are four main aspects of verbal communication: the sender, the message, the receiver, and the response.7 A model representing these aspects is shown in figure 8–1.
Sender. To begin the communication, the sender conveys a message to the recipient. The initial sender of the message can be the pharmacist, pharmacy technician, another health care provider, or the patient. The message can be conveyed verbally (by talking), nonverbally (without talking), or both verbally and nonverbally.
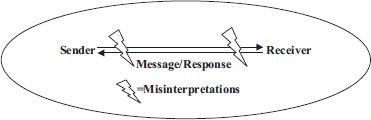
Figure 8–1. The Four Aspects of the Communication Model. Source: Adapted from Reference 7.
Message. The message is the information being conveyed from the sender to the recipient. Some messages are carefully considered before their delivery, whereas others are delivered more impulsively, sometimes as one of the results of an emotional situation. Messages can also be conveyed as sending “mixed signals” or with their real meaning hidden, confusing, or otherwise less than obvious. The vocal tone in which a message is delivered can also play a significant role in how the message is received. In many circumstances, nonverbal messages may also contribute to the wrong message being received by the recipient.
For example, a pharmacy technician in a hospital may call the nursing unit and say, “Hello, Nurse Smith. This is Lois, the pharmacy technician. We have sent the STAT IV [intravenous] solution for Mr. Jones in room 271. Haven’t you gone to the tube station to get it yet?” A variation of the message could be the following: “Hello, Nurse Smith. This is Lois, the pharmacy technician. We’ve sent the STAT IV solution for Mr. Jones in room 271. I’m just calling to make sure you’ve received the IV on time and to see whether there’s anything else we need to send you for the patient.” Clearly, the second message is more patient-centered, and more likely to get a partnership-like response from the nurse.
Receiver. The receiver is the recipient of the message. This being the case, the recipient must interpret the message and decide what its meaning is. The recipient must not only understand what has been said, but also decide whether anything important has been omitted or conveyed with incorrect emphasis. Sometimes the perception of the receiver can be clouded by a personal opinion concerning the message’s sender. The individual may focus on some facts that confirm/reinforce his or her prior perceptions and may disregard or misinterpret facts that change/challenge them. It is important to ensure that the recipient understands the message being verbalized, and to confirm that it is understood as the sender intended it to be. In that way, the conclusion that is reached by the recipient about the message is more likely to be consistent with the intent of the message being sent. Unfortunately, however, individuals process information and interpret it in their own unique ways, something that can lead to misinterpretation and conflict.
In the first message above, there was an implied tone of annoyance in the question. In addition, the nurse may have perceived that the message carried blame and the implication that something the nurse failed to do resulted in the lack of the product’s receipt. This approach was more likely to foster disagreement, denial, and lack of cooperation. In the second message, the technician’s approach was one of assisting and supporting, and voiced a concern aimed at ensuring that all the current needs had been met. The concern was extended on behalf of not only the patient but the nurse as well.
Response. After the recipient of the message interprets its meaning, the response or reaction to the message will indicate whether an understanding was mutual. The recipient will convey this response verbally, nonverbally, or through a combination of both. This is a point at which misunderstandings can be realized and clarifications offered, if needed, to help ensure that the intended message was the one that was received.
In the first message above, a typical response may have been: “Don’t you think I would have looked at the tube station first? You must think I have time to keep looking for something that should have been here already. People in the pharmacy are inconsiderate . . .” The second message may have produced an entirely different response, such as: “I really appreciate your doublechecking to make sure I received the IV. Yes, I’ve got it, and I’ll be able to administer it on time. Thank you for caring enough to check.” The second response reflects the type of response desired when communicating such a message.
Nonverbal Communication
Nonverbal communication is the exchange of messages by means other than speaking. This may include—but is not limited to—appearance and behavior, body language, physical distance, and physical contact. Nonverbal communication is usually interpreted to convey attitudes and emotions, and it can enhance (by adding clarity) or disrupt (by contradicting) verbal communication efforts. Awareness of nonverbal communication can help technicians communicate effectively.
Professional Appearance and Behavior. A pharmacy technician should maintain a professional appearance and behave professionally at all times. As a representative of the pharmacy team, the technician who maintains a professional appearance and behaves professionally helps form positive impressions of the pharmacy operations and services and inspires patient confidence. A professional appearance includes a visible identification badge, good grooming, cleanliness, and socially appropriate clothing. Professional behavior includes displaying a high level of respect to patients, coworkers, and other health care professionals. Jokes or political comments able to be overheard by patients should be avoided. Religious and ethnic comments, even when seemingly innocent, can cause many problems and are never acceptable. Telephone use should be restricted to conducting the business of the pharmacy except during designated breaks. Personal mobile phone calls and texting, except for emergency purposes, should be discouraged, for they can distract the technician from gathering accurate information from patients and can contribute to errors in the medication filling process by decreasing concentration.
Body Language. Body language, or bodily mannerisms that can be interpreted as unconsciously conveying one’s feelings or psychological state of mind, can have a profound impact on how a message is received by the recipient. Facial expressions should correspond to the message being delivered. Pleasant smiles convey positive thoughts or feelings. Expressions representing concern should look different than those depicting humor or amusement. An expression conveying deep thought should accompany a discussion based on problem solving. Inappropriate expressions, such as lack of eye contact, eye rolling, and grimacing, can undermine effective communication, give the wrong impression about the intent of the message, or convey a lack of true interest in the patient.
To foster open communication and trust, the technician should use body postures that convey attention and interest, such as by standing with raised shoulders and head erect, slightly leaning toward the patient and with the arms at the sides, or slightly gesturing in a positive manner. Avoid body postures that may represent a lack of interest in or patience with the patient, such as arms crossed on the chest, hands on the hips, or a back turned to the patient during conversation.
Physical Distance. Physical distance, or the space between two individuals during an activity being carried out between them, may contribute to the success or failure of communication. The technician should determine an appropriate distance to maintain from the patient based on the nature of the encounter. Acceptable distances have been described as 1.5 to 4 feet for personal discussion and 4 to 12 feet for impersonal business.7 The levels of privacy needed to be observed can help guide these distances. When gathering patient-related information that would be considered confidential, closer distances should be observed to protect privacy. When conveying concern for a patient’s circumstances or situation, the distance of separation may reflect a higher level of closeness. When a conversation is ending, the distance between the patient and technician may increase, signaling closure. In addition, observation of the patient’s body language is generally a clue as to whether the correct boundaries have been observed. Physical distance as it pertains to cultural differences will be addressed in a later section of the chapter.
Physical Contact. Physical contact, a situation in which two individuals actually touch, may help to convey caring or understanding. Some patients may appreciate this type of personal expression; others may not. The patient’s comfort with being touched may arise from his or her personal beliefs, cultural norms, or traditions. As with the determination of appropriate physical distance, an observation of the patient’s body language can help to guide a decision as to whether touching is appropriate, and, if so, when to do so. In addition, the technician can ask the patient if he or she desires to be touched. Physical contact as it pertains to cultural differences will be addressed in a later section of the chapter.
Written Communication
Written communication involves the transcribing of information onto paper or another medium for transmission, such as e-mail. Common written communications in pharmacies may include notes/memos, e-mails, shift reports, faxes, reports or documentation forms, entries in want books (inventory control), and prescriptions. As with verbal communication, once a message has been written and delivered to a recipient, it cannot be taken back, so it is very important that the correct message be conveyed to the recipient to elicit the intended response. Every effort must be made to prevent inaccuracies, errors, inappropriate content, and unprofessional attitudes or remarks. Care should be taken to compose clearly written information, spell words correctly, and avoid the use of slang or confusing terminology. In addition, written communications should be composed using a friendly tone, with brevity appropriate to their purpose, at a level for their intended audience, and including salutations/titles as needed.
In contemporary pharmacy practice settings, written communication may be required of the pharmacy technician in various roles and responsibilities. Written communication can be used when the pharmacy technician helps the pharmacist serve patients, engages in activities related to medication distribution and inventory control, and participates in pharmacy practice management and administration. Incorrect written communication in any of the above areas can result in undesirable consequences that can directly affect patient health and well-being, product availability, and overall pharmacy operations and finances.
The Patient Encounter
Pharmacy technicians can encounter patients in many of the pharmacy practice settings in which they are employed. The nature of the patient encounters will be determined by the type of practice environment, the designated role and responsibilities of the technician, the policies and procedures of the practice setting, and the method of interaction used.
Type of Environment. Different levels of pharmacy technician communications can occur in various practice settings. In all settings, technicians will communicate with their coworkers and supervisors. In community and ambulatory care pharmacy settings, common patient-related communications will occur when a new prescription or refill is requested, when patient profile information is gathered, and when a medication is being picked up. Communication also occurs when the technician answers the telephone and responds to questions about pricing, insurance, and product location.
In hospital pharmacy and other institutional care settings, most of the communications occur with other health care professionals rather than with patients. However, effective communication skills between pharmacy technicians and other health care professionals are essential for high-quality patient care and harmonious work environments. As the scope of technician responsibilities grows, the reasons and opportunities for direct patient communication may also increase. Patient and health care professional communications in other types of practice settings are based on the level of available or necessary direct contact.
Purpose of the Encounter. In proper communications, the purpose of the encounter needs to be understood by each individual involved in the communication exchange to establish essential relationships and provide for the exchange of necessary information. For example, when a technician asks a patient a question, such as when completing a patient profile, the purpose is to gather information to initiate a specific action or clarify an issue. In this case, an action would include recording a patient’s allergy in the profile, which might facilitate a patient counseling session by the pharmacist. In a community or mail-order pharmacy setting, a technician may ask the patient for verification of medication insurance coverage or payment for the medications. In a hospital setting, a pharmacy technician may enter a patient’s room to check on the status of an IV fluid or to return unused/expired medications to the pharmacy. If the goal of the communication is to solve a problem, the importance or urgency of the issue must be assessed, and the proper questions asked when gathering information to help ensure that the desired outcome is achieved.
Method of the Encounter. The method of the encounter determines the role that verbal and nonverbal communication factors play in its success. Common methods include face-to-face encounters, telephone encounters, and Internet and other electronic means of communication.
Face-to-Face Encounters. In a face-to-face encounter, both verbal and nonverbal communications are important. How individuals relate to each other during this type of encounter will depend on what was spoken and how, what body movements were used during the conversation, and the environment in which it took place. All conscious and unconscious actions have the potential to impact the intent of the communication and either prevent or cause misunderstandings, so great care should be taken to remain aware of personal behavior.
Telephone Encounters. In telephone encounters, nonverbal communication does not play as significant a role as in verbal communication. Clearly, what was spoken and how it was spoken (e.g., in an enthusiastic, abrupt, or negative tone) can affect how the message is perceived by its recipient. A pleasant tone, for example, helps convey courtesy and caring. A loud or abrupt tone may convey annoyance, impatience, or disrespect, all of which may prompt hostility during the encounter. A pleasant attitude and a smile, even though unseen by an individual on the other side of the telephone, can be very apparent.
At the beginning of a telephone conversation, pharmacy technicians should identify themselves by stating name and title and the name of the pharmacy or pharmacy department. It is also very important to speak clearly and not too rapidly, pronouncing words completely and avoiding the use of slang or potentially confusing terminology.
Internet and Other Electronic Communication Methods. The use of the Internet and fax for communications has greatly expanded in pharmacy practice settings. Evolving uses are for electronic transmittal of prescriptions, medication refill requests, drug information requests and retrieval, product ordering, and other potential time-saving uses. Neither verbal nor nonverbal communication factors play a significant role in these types of encounters, but the principles of effective written communication should be followed.
Internet “etiquette” also dictates that e-mail and business-related messages not be composed of all uppercase letters, to prevent the perception of “shouting” or “scolding.” In addition, when sending a message to a patient or other business-related client, use the business e-mail address or official Web site address so that the recipient knows that the message is legitimate. Never ask patients to provide information over the Internet that could lead to “identity theft” unless it is transmitted through the use of a security-encrypted Web site. When faxing documents, be sure to include a cover sheet to ensure that all information reaches the appropriate person, and follow the Health Insurance Portability and Accountability Act (HIPAA) requirements to maintain the privacy of patient protected health information (PHI). For important documents, use a method of verification of information receipt.
Gathering and Delivering Information. When the intent of the communication effort is to gather information (i.e., by asking a question) or to deliver information (i.e., to answer a question), several key elements must be considered to bring about success.
Approach. When asking a question, a pharmacy technician makes a decision about the best way to approach and conduct a conversation with a patient. He or she makes a behavior choice to use passive, assertive, or aggressive behavior when making the request. Underlying this choice is the desire to avoid conflict and accomplish the goal. Passive behavior, in which an individual does not take an active role or lets others make decisions, is often used to avoid involvement; it can also be used to evade responsibility for something. This behavior is not an effective problem-solving technique and can actually lead to harmful results (e.g., not correcting a patient’s medication adherence problem to avoid conflict). Assertive behavior, in which an individual displays a confident attitude and expression of ideas as well as opinions, is used to directly address an issue, resolve conflict, and actively participate in the conversation to produce a positive outcome. The element of mutual respect is usually present.8 Aggressive behavior, in which an individual displays an overbearing or intimidating attitude, can result in conflict and create a combative atmosphere and a perception of disrespect. This approach usually results in an angry and disruptive encounter.8 An assertive approach to communication and problem solving is superior to an aggressive one, because it promotes and builds the relationships needed for successful patient care and productive work environments.8–9
Asking the Question. In order for the pharmacy technician to receive an accurate and complete answer from the patient, the correct question needs to be asked in a manner likely to gather the most comprehensive level of needed information. This may require determination of the type of question to ask. Two common types of questions are “closed-ended” and “open-ended” questions.
Closed-ended questions are questions that can be answered with a simple “yes” or “no.” An example of a closed-ended question is, “Are you allergic to any medications?” Open-ended questions are questions that require a more elaborate response. An example of an open-ended question is, “What medications are you allergic to?”
 Open-ended questions should be used to gather more indepth answers.
Open-ended questions should be used to gather more indepth answers.
They can help verify or clarify understanding of information by requesting patients to elaborate on the concepts being discussed. A follow-up question may be needed to further elicit important information. If the patient indicates the presence of a medication allergy, an important followup question to ask would be, “Can you describe what happens when you take the medication?” The question, “What else are you allergic to?” would be asked until the patient verifies that no more allergies are present.
Listening. After asking the question, the technician must listen carefully to the answer and observe any nonverbal communication being displayed. Listening helps the technician better understand the patient’s perceptions, sense the patient’s emotions, and hear what the patient is saying. It is important to remember that when an individual is talking, he or she is not also listening. Listening improves not only what is heard, but what will be said in response. By paying attention, with only necessary interruptions to clarify, the patient can feel the satisfaction of being heard and understood. Otherwise, if the technician verbalizes a response that reflects an alternate point of view, the patient may believe that he or she may not have been heard, which can prevent the continuation of constructive dialogue. To understand the needs of others, an individual must listen to what is being said by the other individual in its entirety. Listening also helps determine whether the question was fully understood. Avoid the appearance of “faking” interest. If you are not in a position to help the patient, arrange for someone to help who is better able to do so. It is also essential to not assign a personal value judgment to what is being communicated, for to do so can affect your ability to appropriately address the situation or concern. While listening, also be careful not to craft a mental response before listening to the patient’s complete concern. This will help you keep from developing counterarguments to what has been said, which may foster a breakdown in communication when they are verbalized.
Responding. Strong patient-provider relationships can be built when responses to questions or concerns are addressed in an empathetic manner. Empathy, in which an individual is able to identify with and understand another individual’s feelings or difficulties, helps establish a caring and trusting relationship.8 These types of responses help convey to patients that they have truly been heard and that their feelings are understood and respected. Other effective response types involve restating or paraphrasing the patient’s expressed feelings to ensure complete understanding. These manners of responses help promote open conversation with the patient, particularly when there are potentially emotional issues present.8
Returning to our scenario again, examples of responses follow:
A patient arrives at the pharmacy counter with a new prescription. After handing the prescription to the pharmacy technician, the patient is informed that the prescription will not be ready for at least an hour. The patient responds, “That’s ridiculous! It can’t take that long to take a few pills from a container and put them in a bottle. I want my prescription filled right now, or I’m taking it to another pharmacy where people know what they are doing!”
An empathetic response to the situation could be: “You seem to be concerned about our ability to provide you with the correct medication in a timely manner.”
A restating or paraphrasing response could be: “I understand that you feel that it shouldn’t take that long to fill your prescription.”
Each of the above responses allows the technician to gather more information from the patient in order to get a better understanding of the problem, to open the lines of communication, and to help the patient feel that the technician is listening to his or her expressed concerns. These responses are not given until the patient has finished stating the original concern or issue to be addressed. Counterarguments, meant to contradict or oppose something that an individual has said, should not be mentally rehearsed as responses, because they prevent the use of empathetic or paraphrasing techniques. A counterargument to the above scenario might be: “We know what we’re doing at this pharmacy. It always takes at least an hour to get your medicine. What do you think this is, McDonald’s?”
There are four types of responses that should be avoided because they can be perceived negatively by the patient and produce an undesirable outcome:
A judgmental response to the situation above could be viewed as devaluing the patient’s concern, as in: “You seem to be the only one concerned about our ability to provide you with the correct medication quickly. All our other patients really love us and don’t seem to care about the wait.”
An advice-giving response to the situation could be viewed as evidence that the technician thinks that the patient doesn’t understand, or hasn’t thought through the comments; it might consist of the following statement:“You need to talk to the other patients who are waiting here. They will tell you that we know more about medicine and the prescription-filling process than you do.”
A quizzing response to the situation could be viewed as evidence that the technician thinks that the patient is confused or wrong; for example: “Think back to when you have picked up medication at other pharmacies. I don’t believe that you have gotten it as quickly as we are going to give it to you. ”
A placating response to the situation above could be viewed as condescending, for example: “Oh, you shouldn’t worry so much about the length of time. Just shop around for a while until it is ready, and try not to get yourself so worked up.”
There are times when, despite all best efforts, unmanageable conflict occurs. Personal limits on the extent of involvement should be set and the issue referred to appropriate supervisory personnel.
Verification of Understanding. It is important that an effort is made to verify the patient’s understanding prior to the end of the conversation. In this way, actions can be summarized, agreements reached, or reasonable alternatives suggested.
Honesty and Ethics. When addressing a patient’s question or concern, nothing can destroy confidence or trust in a health care provider or practice setting faster than discovering dishonest and fraudulent answers or practices. Examples of situations in which communications with patients are difficult include incidents of suspected medication-related errors. A health care professional should always put the health of the patient ahead of personal concerns. Suspected errors should be brought to the pharmacist’s attention immediately so that full disclosure and proper management of the patient’s health needs can be undertaken. Cover-ups and related negligent actions have no place in a patient-centered care facility because they can lead to patient harm, legal action against the pharmacy and against pharmacy personnel, and loss of employment.
Confidentiality. Confidentiality and privacy are not only patient rights, but also legal issues. The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that prohibits the disclosure of protected health information (PHI) to anyone without the patient’s permission or outside of the process of providing patient care.
 When gathering information for inclusion in a patient’s profile, every effort should be made to conduct this conversation in a manner that ensures as much privacy as possible.
When gathering information for inclusion in a patient’s profile, every effort should be made to conduct this conversation in a manner that ensures as much privacy as possible.
In addition, patients may ask for certain products that could be considered embarrassing. A patient has a right to expect that the pharmacy technician will exhibit the highest level of discretion in these situations and obey all laws regarding privacy requirements. In situations when a message must be left for a patient on a telephone answering machine, caution must be used by the technician to allow the information to be given without violating the patient’s confidentiality. For a more in-depth discussion of these concepts, please refer to Chapter 2: Pharmacy Law.
Medication Information and Counseling. As described in Chapter 7: Drug Information Resources, numerous questions are posed to pharmacy technicians in every practice setting, and technicians must honor the boundaries of their scope of practice responsibilities. For example, when patients have questions about the dosages, effects, and administration of medications or the choice of medications to treat specific health concerns, those questions should be directed to the pharmacist. A pharmacy technician should ask a patient whether medication counseling is desired by using an open-ended question, such as, “What questions do you have for the pharmacist about your medication?”—but they should not provide the actual counseling. This is true for both over-thecounter (OTC) and complementary and alternative medication (CAM). Pharmacy technicians must be guided by their prevailing state laws, pharmacy practice acts, and organizational policies/procedures as to their roles and responsibilities in the areas of medication information and counseling.
Communication Strategies for Special Patient Populations
Certain situations warrant modification of typical communication strategies to help ensure effective communication.
Angry or Hostile Patients. Patients are often coping with a number of personal issues related to their health concerns. Some patients are better able to cope with these challenges than others. Even with angry or hostile individuals, it is important to show understanding and caring to help ensure effective communication. Communicating with individuals who are angry requires the technician to recognize what may have provoked the conflict, as well as how to address or resolve it. As previously discussed, the technician must actively listen to the patient and observe body language to better understand the individual’s feelings and perceptions. Then, the technician should express an understanding of the problem in a meaningful way, seeking clarification of issues when needed. If possible, the technician should attempt to address or solve the problem, if it is in his or her ability to do so. Issues that are beyond the ability of the technician to address should be directed to the pharmacist or other supervisory personnel for resolution. During conflict resolution, it is important that professional attitudes and self-control be exhibited at all times.
Patients with Terminal Health Conditions. Patients who are facing terminal illness and death need supportive care and unique understanding. Some health care professionals may find it difficult to communicate with patients in this situation without first resolving their own feelings about death and dying. It is important to ask open-ended questions to inquire about the patient’s state of being, to be understanding of his or her feelings, and to respect whatever strategies are being used to cope with their circumstances. Family caregivers may be responsible for patients who are unable to fully care for themselves.10 In this role, caregivers may not only be responsible for administering medications, but also provide physical and emotional support for the patient. These individuals can experience many of the same emotions as the patient, so it is important that expressions of support, care, and understanding be extended to them as well.
Patients with Mental Illness. Communicating with patients with mental health illnesses can be challenging for health care professionals. It is important to ask openended questions to determine their level of understanding of health-related issues. In addition, mistaken belief, labeling, and stereotyping are unacceptable and greatly hinder communication efforts. Genuine interest and concern should be exhibited through the use of patientcentered communication strategies.
Older Adult Patients. Older adults are the fastestgrowing population group and account for the highest percentage of medication use (both prescription and over-the-counter).10 The aging process can present challenges for older adults when it comes to their communication abilities. These challenges can include changes in memory, attention span, perceptions, vision, hearing, speech, and mobility.
Strategies for improving communication in this population include using open-ended questions, information reinforcement materials, materials written in larger type, proper vocal tone and body positioning (avoid shouting), brighter environmental lighting, slower speech, and patience.7–8 It is also important, as it is with patients with mental illness, to avoid mistaken beliefs, labeling, and stereotyping, all of which hinder communication efforts.
Another consideration when communicating with older adults is their increased use of patient caregivers who care for them and assist in the management of their medications and health conditions. Although the use of caregivers may prevent direct communication with the actual patient, it is important that the same level of care and understanding be extended to these individuals as well. They should also be encouraged to ask questions or to facilitate the patient’s ability to ask questions when necessary.
Patients with Low Health Literacy. Current information shows that as much as half the U.S. population lacks the adequate general literacy (i.e., the ability to read and write at a capable level) to effectively carry out their necessary medical treatments and preventive health care plans.11 Individuals with poor general literacy skills have associated poor health literacy skills.11–12 Health literacy, or the ability of an individual to read, understand and act upon health care information, is an important predictor of health care outcomes. It affects how an individual understands wellness and illness, participates in disease prevention, decides health-related treatments, takes medications, and follows self-care instructions.12 Poor health literacy is more prevalent in the poor, minority, older adult, and recent U.S. immigrant populations. The consequences of poor communication in individuals with low health literacy include poor health outcomes (e.g., errors, hospitalization, poor quality of life, and even death).
RX for Success
Technicians who are able to identify patients with these types of special needs and can effectively communicate these concerns with the pharmacist and other health care professionals are invaluable for patient care.



