Learning Outcomes
After completing this chapter, you will be able to
 Identify the common drug names for each classification.
Identify the common drug names for each classification.
 Describe the important actions and/or therapeutic uses for the major classes of drugs.
Describe the important actions and/or therapeutic uses for the major classes of drugs.
 Describe the most common or most serious adverse effects for the major classes of drugs.
Describe the most common or most serious adverse effects for the major classes of drugs.
 List special precautions for the major classes of drugs.
List special precautions for the major classes of drugs.
Key Terms
| agranulocytosis | A dramatic decrease in white blood cells. |
| antiproliferative | A substance used to prevent the spread of cells into surrounding tissue. |
| arthralgia | Joint pain. |
| cross-sensitivity | Sensitivity to one substance that predisposes an individual to sensitivity to other substances that are related in chemical structure. |
| expectorate | To cough up or spit. |
| myalgia | Muscle pain. |
Drugs that Affect the Nervous System
Drugs that Affect the Cardiovascular System
Drugs that Affect the Respiratory System
Drugs that Affect the Musculoskeletal System
Drugs that Affect the Endocrine System
Drugs that Affect the Immune System
Drugs that Affect the Gastrointestinal System
Drugs that Affect the Urinary System
Drugs that Affect the Other Body Systems
Section 2: Women’s and Men’s Health
Drugs Related to Women’s Health
Section 4: Hematologic and Oncologic Agents Drugs that Affect the Hematologic System Section 5: Nutritional and Dietary Supplements Herbals and Other Dietary Supplements |
|
A drug can be defined as any substance that, when introduced into the body, alters the body’s function. An ideal drug has several characteristics: effectiveness for its therapeutic use, safety even if large quantities are ingested, and no adverse effects. Unfortunately, the ideal drug does not exist. All drugs have some adverse effects and many drugs are toxic when more than the recommended dose is taken. Therefore, the decision to use any drug therapy is made after weighing the benefits of the drug against the risks involved with its use.
There are many different ways to classify medications. They can be classified by medical conditions, by body organ systems, or by type of action. Drugs often have actions in more than one part of the body and may be mentioned in several areas. The major actions or uses of drugs, their major adverse effects, and important characteristics particular to specific drugs, especially where these characteristics are important in dispensing activities, will be discussed. Many of the drugs discussed are listed in tables with both the generic name and the trade name listed. The United States Adopted Names Council (USAN) has approved stems for generic names that help to classify medications according to their mechanism of action. For example, the medication metoprolol has an -olol ending and is classified as a beta-blocking agent, which is commonly used to treat high blood pressure. Learning to recognize these stems will help in identifying the classifications for different medications.
Section 1: Body Systems
Drugs that Affect the Nervous System
Antiepileptic Agents. There are several types of seizures, and some of the medications discussed here may be used alone to treat one or more types of seizures, whereas others may need to be used in combination with other antiepileptics to control certain types of seizures. Some antiepileptic drugs have other therapeutic uses, such as migraine prevention, psychiatric disorders, a painful facial nerve condition called trigeminal neuralgia, and other types of nerve pain.
Antiepileptic agents, also called anticonvulsants, are used to reduce the frequency of seizures.1 They do this by reducing the excitability of the nerve cells in the brain.2 All antiepileptics have adverse effects, so they are only used when the risk of recurrent seizures is more worrisome than the adverse effects of the drugs. Therapy is usually started with one medication in order to minimize the adverse effects and improve patient compliance.
In approximately 50–70% of patients, seizures can be controlled with one agent.1 Medications should be started with low doses and then titrated up, allowing for the dosage to be individualized for each patient. Once therapy is started, patients need to be monitored for treatment success or failure. Monitoring may include blood levels or the number of seizures and side effects. If therapy is considered a failure, either due to lack of seizure control or adverse effects, the medication may be changed or an additional medication may be added.1
Antiepileptic agents should not be discontinued abruptly.2 Some patients may experience seizures if the medication is suddenly stopped. Ideally, agents should be slowly tapered over one to three months.2
The major drugs used to control seizures are phenytoin (Dilantin), carbamazepine (Tegretol), levetiracetam (Keppra), and divalproex sodium (Depakote). Other drugs available are listed in table 10-1, along with the types of seizures they treat. Older agents require stricter monitoring and are often taken more frequently, reducing patient compliance. Some of these medications are now available as generic formulations. It should be noted that there may be differences in the bioavailability (extent of absorption) of the generics versus brand-name drugs. This may correlate to an increase in adverse effects/toxicities or an increase in seizure frequency. Therefore, patients should be closely monitored when switching between products.2
| Generic Name (Brand Name) | Dosage Forms | FDA Approved Indications |
| Carbamazepine (Tegretol, Tegretol XR) | capsules, suspension, tablets, extended-release | Tonic-clonic, partial seizures |
| Clonazepam (Klonopin) | tablets, oral-disintegrating tablets, wafers | Absence, myoclonic seizures |
| Diazepam (Valium, Diastat) | Injection, rectal gel | Status epilepticus |
| Divalproex sodium (Depakote, Depa-kote ER) | capsules (sprinkle), delayed-release tablets, extended-release tablets | Absence, partial seizures |
| Fosphenytoin (Cerebyx) | injection | Status epilepticus, prevention and treatment of seizures during neurosurgery, short-term administration when unable to take oral phenytoin |
| Gabapentin (Neurontin) | capsules, solution, tablets | Tonic-clonic, partial seizures |
| Lacosamide (Vimpat) | Tablets, injection | Adjunctive to partial |
| Lamotrigine (Lamictal, Lamictal XR) | tablets, oral-disintegrating tablets, extended-release tablets | Partial seizures |
| Levetiracetam (Keppra) | injection, solution, tablets, extended-release tablets | Adjunctive to partial |
| Lorazepam (Ativan) | injection | Status epilepticus |
| Oxcarbazepine (Trileptal) | suspension, tablets | Partial seizures |
| Phenobarbital | Tablets, injection | Generalized tonic-clonic, partial seizures, status epilepticus |
| Phenytoin (Dilantin) | extended-release capsules, chew-tabs, suspension, injection | Generalized tonic-clonic (grand mal), complex partial seizures, prevention and treatment during or following neurosurgery, status epilepticus (IV) |
| Pregabalin (Lyrica) | tablets | Adjunctive to partial |
| Tiagabine (Gabitril) | tablets | Adjunctive to partial |
| Topiramate (Topamax) | capsules (sprinkle), tablets | Adjunctive to tonic-clonic, partial |
| Valproic acid (Depakene), valproate sodium (Depacon) | capsules, syrup, injection | Absence seizures, complex partial, simple |
| Zonisamide (Zonegran) | capsules | Adjunctive to partial |
Status epilepticus is a condition of repetitive seizures with little or no interruption between them. This is a lifethreatening condition that must be treated immediately using IV medications. These agents are generally used only by emergency personnel or in an institutional setting. Injectable forms of the benzodiazepinesdiazepam (Valium) and lorazepam (Ativan) are commonly used initially to stop the repetitive seizure activity. Longer-acting drugs, such as phenytoin (Dilantin) or fosphenytoin (Cerebyx), are given to prevent the recurrence of seizures.2
Phenytoin has been available for many years and effectively prevents many types of seizures. Dosing of phenytoin is complicated, and blood levels are usually measured to ensure that enough phenytoin is present to prevent seizures but not enough to cause side effects. This drug is known to have a narrow therapeutic index, which means small changes in the dose results in large changes in the drug’s effects. Side effects that are dose-related include double vision, loss of muscle coordination, and sedation. Side effects that are common but are not related to the dose are overgrowth of the gums (gingival hypertrophy) and excessive hair growth (hirsutism). Phenytoin also has many drug interactions. Patients should be warned not to take extra doses or other drugs without checking with their doctor or pharmacist first.2
Fosphenytoin (Cerebyx) is an injectable medication that is converted to phenytoin in the body. An advantage of fosphenytoin is that it can be mixed in either normal saline or dextrose, whereas phenytoin IV must be mixed only in normal saline. If phenytoin is mixed with dextrose, a precipitate will form. Fosphenytoin also causes less damage to veins, it can be infused over a shorter period of time, and it causes less hypotension (low blood pressure) compared to phenytoin.2 Fosphenytoin is preferred over phenytoin in many institutions.
Like phenytoin, blood levels of some antiepileptics are measured to ensure that the dose is producing therapeutic blood levels but not levels high enough to result in adverse effects. Newer agents do not need this additional monitoring. Liver function and blood cell counts must be monitored with several of the antiepileptic drugs. Carbamazepine (Tegretol) can cause a rare, serious adverse effect called pancytopenia, which is a depression of the production of all types of blood cells (red cells, white cells, and platelets). Liver toxicity is a serious side effect of divalproex sodium (Depakote) use, but is reversible if the drug is stopped. Other side effects of antiepileptic agents may include dizziness, fatigue, nausea, vomiting, headache, weight gain, increased appetite, and hair loss. Phenobarbital is effective against a number of different seizure types, but the adverse effects of phenobarbital, mainly excessive sedation and the potential for dependence and withdrawal symptoms, limits its usefulness today.
 The antiepileptic drugs increase the risk of suicidal thoughts or behavior; therefore, it is important that patients are monitored for unusual changes in mood or behavior. An FDA-approved Medication Guide must be dispensed with all prescriptions for antiepileptic drugs warning patients about this potential risk.
The antiepileptic drugs increase the risk of suicidal thoughts or behavior; therefore, it is important that patients are monitored for unusual changes in mood or behavior. An FDA-approved Medication Guide must be dispensed with all prescriptions for antiepileptic drugs warning patients about this potential risk.
Parkinsonian Agents. Parkinson disease (PD) is a progressive disease, and the goals for treatment are to maintain function and quality of life, as well as to avoid drug-induced complications. Drug therapy is focused on decreasing acetylcholine and increasing dopamine (table 10-2). Drugs affecting dopamine levels include levodopa, dopamine agonists, catechol-O-methyl transferase (COMT) inhibitors, and selegiline. Drugs used to restore the balance between acetylcholine and dopamine include anticholinergics and amantadine.
Table 10–2. Drugs Used to Treat Parkinson Disease
| Classifications and Medications | Available Dosage Forms |
| Anticholinergics | |
| Benztropine (Cogentin) | Tablets, injection |
| Trihexyphenidyl (Ariane) | Tablets, sustained-release capsules |
| Amantadine (Symmetrel) | Tablets, capsules, solution |
| Carbidopa/levodopa products | |
| Carbidopa/levodopa (Sinemet, Sinemet CR) | Tabets, extended-release tablets |
| Carbidopa/levodopa/entacapone (Stalevo) | Tablets |
| MAO-B inhibitors | |
| Rasagiline (Azilect) | Tablets |
| Selegiline (Eldepryl, Zelapar ODT, Emsam patch) | Capsules, oral-disintegrating tablets, transdermal patch |
| COMT inhibitors | |
| Entacapone (Comtan) | Tablets |
| Tolcapone (Tasmar) | Tablets |
| Dopamine agonists | |
| Bromocriptine (Parlodel) | Tablets, capsules |
| Pramipexole (Mirapex) | Tablets, extended-release tablets |
| Ropinirole (Requip) | Tablets, extended-release tablets |
| Apomorphine (Apokyn) | Subcutaneous injection |
The main therapies for PD include levodopa plus carbidopa, dopamine agonists, and the monoamine oxidase (MAO-B) inhibitors.3 The most commonly used treatment is the combination of levodopa and carbidopa. Levodopa is converted to dopamine in the body, but it must move into the brain to be helpful for Parkinson’s treatment. Unfortunately, once it is converted peripherally, only a small amount is able to enter the central nervous system (CNS). The remainder stays in the periphery and causes side effects such as nausea, vomiting, arrhythmias, and orthostatic hypotension.4
Carbidopa is a dopa decarboxylase inhibitor and keeps levodopa from being converted to dopamine in the periphery. By getting the levodopa into the brain for conversion to dopamine, it decreases the side effects in the body and increases its effectiveness for the treatment of PD. Akinesia (loss of normal motor function), tremor, and rigidity often improve with the use of levodopa and carbidopa, but balance and gait (the rate of moving, especially walking) may not. Medication compliance may be an issue with these agents because the tablets need to be taken three or more times a day. An extended-release formulation is also available to decrease the frequency of administration to two or three times a day.
Dopamine agonists are thought to work by binding to and stimulating the dopamine receptors. This class of medications appears to improve movement or motor functions. Pramipexole (Mirapex) and ropinirole (Requip) are indicated for monotherapy or adjunct therapy with levodopa/carbidopa. The most common side effects include depression, confusion, insomnia, anxiety, hypotension, and arrhythmias. These agents are more selective for the dopamine receptors, leading to fewer side effects than some of the other classes. Pramipexole and ropinirole have extended release formulations available for once-a-day dosing.2
Apomorphine (Apokyn) is a dopamine agonist that can be used to treat the “off” periods of movement. It is a subcutaneous injection that is generally given as needed. It is considered adjunct therapy to other agents. In some patients, apomorphine may cause orthostatic hypotension, so patients should receive a test dose and have their blood pressure monitored closely prior to starting therapy. The most common side effects are nausea and vomiting. Patients should be treated with the antiemetic agent trimethobenzamide (Tigan) prior to receiving a dose of apomorphine.2
Anticholinergic agents and MAO-B inhibitors have an important role in PD. Anticholinergic agents are known for their drying effects. Because of these side effects, they have been found to be useful in improving the drooling effects seen in patients as well as some improvement in the tremor of early disease. MAO-B inhibitors may also be used in mild symptoms. Rasagiline (Azilect) has been approved to be used as monotherapy.
The COMT inhibitors are generally considered thirdor fourth-line therapy and should be used as adjunct therapy with levodopa/carbidopa. These agents work by limiting the breakdown of dopamine, thus allowing for a lower dose of levodopa to be used. The combination levodopa/carbidopa/entacapone (Stalevo) was developed to improve patient compliance so patients don’t have to take two separate agents. Tolcapone (Tasmar) can cause severe liver failure, which limits its use.
Alzheimer Disease Agents. Alzheimer disease is a progressive neurodegenerative disorder. Signs and symptoms include memory impairment as well as behavioral changes in social and functional capacities. The main neurotransmitter thought to be associated with the decline in memory function is acetylcholine.6 At this time, there is no cure for Alzheimer disease. Pharmacologic treatments available are not able to reverse the devastating consequences, but may slow the progression of the disease to allow patients to have a better quality of life.7 The two classes of medications available for Alzheimer disease are the cholinesterase inhibitors and the N-methyl-D-aspartate (NMDA) receptor antagonists (table 10-3).
Other agents that may be used are antidepressants and antipsychotic agents. Patients with Alzheimer often experience depression as part of the disease, so the selective serotonin reuptake inhibitors (SSRIs) may be used to help with this.2 The antipsychotic agents haloperidol (Haldol), risperidone (Risperdal), and olanzapine (Zyprexa) may be used to decrease hallucinations, suspiciousness, agitation, and aggression.2
The cholinesterase inhibitors are first-line therapy for mild-to-moderate dementia of Alzheimer disease; in addition, donepezil (Aricept) has been approved for use in severe Alzheimer disease.8 These agents work by preventing the breakdown of acetylcholine. Increasing the amount of acetylcholine in the brain is thought to result in stabilizing or improving of memory function.6 Choosing the best agent for the patient is based on efficacy, adverse effects, available dosage forms, ease of titration, and cost.2
Table 10–3. Alzheimer Disease Agents
| Classifications and Medications | Available Dosage Forms |
| Cholinesterase inhibitors | |
| Donepezil (Aricept) | Tablets, oral disintegrating tablets (ODT) |
| Galantamine (Razadyne) | Tablets, extended release tablets, solution |
| Rivastigmine (Exelon) Tacrine (Cognex) | Capsules, solution, patch Capsules |
| Tacrine (Cognex) | Capsules |
| N-methyl-D-aspartate (NMDA) receptor antagonists | |
| Memantine (Namenda) | Tablets, oral solution |
Adverse effects of these agents include nausea, vomiting, diarrhea, dizziness, and fatigue.8 These effects can be minimized by starting with a low dose and titrating up. Tacrine (Cognex), which was the first available agent, has been associated with liver toxicity. Due to this adverse effect and because it must be given four times a day, it is now a last-line agent in the cholinesterase inhibitor class.8
The titration of these agents should be slow to minimize gastrointestinal adverse effects. Initial doses are low and then gradually increased every four to six weeks until the target dose is achieved. It is important to note that if rivastigmine (Exelon) or galantamine (Razadyne) are stopped for more than a couple of days, the dose needs to be retitrated back to the maintenance dose.8
Rivastigmine (Exelon) is the only agent available as a topical patch. Titration to maintenance dose is still required with this dosage form. The patch is to be changed every twenty-four hours and recommended placement is on the upper or lower back, although the upper arm and chest may be used if the patient is unable to reach the back. Patients or their caregivers need to be counseled that a new patch should not be applied to the same location for at least two weeks.9
The new class that is now available is the NmethylD-aspartate (NMDA) receptor antagonists. The only agent currently approved in this class is memantine (Namenda), and it has been approved for the treatment of moderate to severe Alzheimer disease. NMDA receptors are stimulated by a neurotransmitter known as glutamate, which is thought to play a role in learning and memory.6 In Alzheimer disease, some patients may have excess amounts of glutamate that can overstimulate these NMDA receptors, leading to a dysfunction in the storage of information. Blocking these receptors with memantine will reduce the overstimulation, potentially leading to the normal functioning of the system.6 Memantine may be used as monotherapy or as adjunct therapy with the cholinesterase inhibitors. Adverse effects include constipation, dizziness, fatigue, and headache. Slowly titrating the dose every four weeks should alleviate these adverse effects.10
Multiple Sclerosis Agents. Multiple sclerosis (MS) is a progressive neurological disorder affecting the brain and the spinal cord. Its onset is generally between the ages of eighteen and forty-five and affects women more often than men.11 In MS, the myelin sheath that covers neurons degenerates, causing a disruption of nerve transmission.2 An inflammatory response occurs that forms lesions or plaques. These lesions are found on the nerves in the brain, spinal cord, and the eye. Symptoms may include visual disturbances, muscle spasms, weakness, balance problems, and difficulty with speech, as well as bowel, bladder, and sexual dysfunction.2 The disease is characterized by exacerbations and remissions. Drug therapy is focused on preventing exacerbations and treating the symptoms (table 10-4). Due to the complexity of the disease, symptoms are treated as they appear. Corticosteroids are often used to reduce inflammation in acute exabercations. Muscle relaxers (e.g., baclofen [Lioresal], tizanidine [Zanaflex]) are used to decrease muscle spasms. Urinary antispasmodics (oxybutynin [Ditropan], tolterodine [Detrol]) treat overactive bladder symptoms, and pain is often treated with neuropathic pain medications such as lamotrigine (Lamictal) or gabapentin (Neurontin).
The most common agents used in MS patients are those that are used for the prevention of relapses and disease progression. The agents used for this treatment have become known as the ABC therapy (Avonex, Betaseron, Copaxone).2 Interferon-?-1b (Betaseron) was the first agent available for reducing the relapses of MS. It is a subcutaneous injection given every other day. Studies show that patients treated with this interferon had no significant increases in lesions during treatment time.12
Table 10–4. Multiple Sclerosis Agents
| Medications’ Generic (Brand) Names | Available Dosage Forms | Indications |
| Glatiramer acetate (Copaxone) | Subcutaneous injection | To reduce the frequency of relapses in relapsingremitting MS |
| Interferon–-1a (Avonex) | Intramuscular injection | Treatment of relapsing forms of MS to slow disease progression and prevent exacerbations |
| Interferon-ß-1b (Betaseron) | Subcutaneous injection | Treatment of relapsing forms of MS and to prevent exacerbations |
| Natalizumab (Tysabri) | Intravenous infusion | Treatment of relapsing forms of MS to delay disease progression and prevent exacerbations; used when an inadequate response or intolerance to other agents |
| Mitoxantrone (Novantrone) | Intravenous infusion | To reduce neurologic disability and frequency of relapses in secondary, chronic progressive, relapsing remitting MS |
Interferon-β-1a (Avonex) is an intramuscular injection administered once a week to patients with MS. Studies of this agent have shown a reduction in relapse rates as well as a slowing of disease progression.13 It is unknown how the interferons reduce the relapses of MS. Side effects can be somewhat limiting. The most common side effect seen is flu-like symptoms following the injection. Fever, chills, and muscle aches can occur for up to twenty-four hours after the injection is given. Pre-treatment with acetaminophen (Tylenol) or ibuprofen (Advil) may help to alleviate the flu-like symptoms. Glatiramer acetate (Copaxone) is a daily subcutaneous injection that is thought to help reduce inflammation, demylination, and nerve damage. The side-effect profile is more favorable than for the interferons. Injection-site reaction is the most common side effect seen with glatiramer acetate (Copaxone). Injectionsite reactions are common among all three agents; these include pain, itching, redness, and swelling.2
Drugs to Treat Headaches/Migraines. In 2001, the number one over-the-counter (OTC) recommendations made by pharmacists were for headache products.14 Headache pain can be described as constant, throbbing, dull, or severe, and may be only on one side or throughout the head.12 They may be classified as migraines, tension, cluster, or others. Some criteria used to classify headaches include the number and length of headaches, level of pain, location of the headache, and presence of nausea, vomiting, photophobia, or phonophobia.17 Treatment of headaches includes acute (abortive) therapy, which involves treating the current headache pain, and preventive therapy. Treatments available do not cure chronic headache, but can help to manage the condition. Goals of therapy include17
 Ability to maintain normal activities
Ability to maintain normal activities
 Provide quick relief of headache pain
Provide quick relief of headache pain
 Reduce frequency of attacks
Reduce frequency of attacks
 Minimize the amount of medications needed
Minimize the amount of medications needed
Acute/abortive treatment is used to stop an attack. These medications should be used only two to three times per week. Overuse of these medications can lead to a medication-induced headache. Drug classes used to treat headaches include non-steroidal inflammatory drugs (NSAIDs), triptans, butalbital-containing products, opioids, steroids, and others (table 10-5).
The most common class of medications used for the treatment of migraines is the serotonin 5-HT1 receptor agonists, or the “triptans.” These medications work by binding to vascular 5-HT1 receptors and causing vasoconstriction. Onset of action is generally within thirty minutes to one hour. Most of the drugs in this class are dosed so that if the patient does not have relief after two hours, he/she may repeat the dose. These drugs should not be used to treat more than four headaches per month. Overuse of these products may lead to “rebound” headaches.18
Table 10–5. Drugs Used to Treat Headaches
| Classifications and Medications | Available Dosage Forms |
| Triptans | |
| Almotriptan (Axert) | Tablets |
| Eletriptan (Relpax) | Tablets |
| Frovatriptan (Frova) | Tablets |
| Naratriptan (Amerge) | Tablets |
| Rizatriptan (Maxalt) | Tablets, orally disintegrating tablets |
| Sumatriptan (Imitrex) | Tablets, nasal spray, injection |
| Zolmitriptan (Zomig) | Tablets, orally disintegrating tablets, nasal spray |
| Sumatriptan and naproxen (Treximet) | Tablets |
| Butalbital-containing products | |
| Butalbital and acetaminophen (Phrenilin) | Tablets |
| Butalbital, acetaminophen, caffeine (Fioricet, Esgic, Esgic-Plus | Tablets |
| Butalbital, acetaminophen, caffeine, codeine (Fioricet with | Tablets |
| Butalbital, aspirin, caffeine codeine)(Fiorinal) | Capsules, tablets |
| Butalbital, aspirin, caffeine, codeine (Fiorinal with codeine) | Capsules |
| Ergotamine derivatives | |
| Ergotamine, caffeine (Cafergot, Migergot, Ergomar) | Suppositories, tablets, sublingual tablets |
| Dihydroergotamine (D.H.E. 45,Migranal) | Injection, nasal spray |
Side effects most commonly seen with these agents include asthenia, dizziness, nausea, fatigue, and dry mouth. Some patients using triptans have experienced some cardiac-like symptoms such as chest, jaw, or neck tightness. These occurrences are rare.19 Non-responders to triptans do occur; that is, the medication does not work for some patients. In these patients, it is possible to try another triptan agent before moving on to another class of drugs.20
Butalbital-containing products are often used, but no studies show that they are effective for the treatment of migraines. These agents belong to the barbiturate classification. Its exact mechanism of action is unknown. It is combined with caffeine and either aspirin or acetaminophen and sometimes codeine to enhance its painrelieving capabilities. Butalbital-containing products can cause dependency in patients and may also cause withdrawal symptoms. Side effects include drowsiness, dizziness, GI problems, confusion, and nervousness.21
Ergotamine derivatives work on headaches by constricting peripheral and cranial blood vessels. Dihydroergotamine (DHE) is the drug most commonly used in this class. DHE should not be used with certain drugs, such as the protease inhibitors (discussed later in this chapter). In addition, DHE should not be used within twenty-four hours of triptans.18
There are some OTC agents available for the treatment of headaches; in fact, some brands have started to market their OTC products specifically for “migraines.” These agents often contain ibuprofen, naproxen, or combinations of aspirin, acetaminophen, and caffeine. A review of studies on the use of OTCs for migraine management shows mixed results. Most showed these products to be more effective than placebo without causing serious adverse reactions. The ability to return to normal daily functions two hours after administration increased for those whose migraines were mild to moderate in nature.16
Patients who have recurring migraines (four or more per month), who are not having adequate relief from other agents, or who have headaches that are disabling should consider preventive therapy. Medications used for preventive therapy are taken on a daily basis. Many medications are used as preventive therapy, but the most common are topiramate (Topamax), propranolol (Inderal), amitriptyline (Elavil), and divalproex (Depakote ER).21
Drugs to Treat Neuropathic Pain. Neuropathic pain may be due to the persistent stimulation of nerve fibers, or nerve damage in the central or peripheral nervous system. This overstimulation can cause the patient pain even without the presence of pressure or being touched. Symptoms of neuropathic pain include spontaneous shooting pain, or a burning or tingling sensation. Often patients describe the pain as pins-and-needles sensation. Unlike for pain in the traditional sense, opioid analgesics are not traditionally used first line for the treatment of neuropathic pain.2 Instead, other classes of agents are used (table 10-6).
Table 10–6. Agents to Treat Neuropathic Pain
| Classifications and Medications | Available Dosage Forms |
| Topical agents | |
| Capsaidn (Zostrix) | Lotion, cream, gel, patch, roll-on stick |
| Lidocaine (Lidoderm) | Patch |
| Antidepressants | |
| Amitriptyline (Elavil) | Tablets |
| Duloxetine (Cymbalta) | Capsules |
| Fluoxetine (Prozac) | Tablets, capsules, oral solution |
| Paroxetine (Paxil) | Tablets, oral suspension |
| Venlafaxine (Effexor) | Tablets, capsules |
| Antiepileptics | |
| Carbamazepine (Tegretol) | Tablets, capsules, oral suspension |
| Divalproex, valproic acid (Depakote, Depakene) | Capsules, tablets, syrup |
| Gabapentin (Neurontin) | Tablets, capsules, oral solution |
| Lamotrigine (Lamictal) | Tablets |
| Pregabalin (Lyrica) | Capsules |
| Topiramate (Topamax) | Tablets, capsules |
One of the topical agents used for the treatment of neuropathic pain is capsaicin (Zostrix), which is a substance found in hot peppers. It works by depleting substance P from the nerves, thus stopping the transmission of pain from one nerve to another. Patients may complain of burning at the application site, and it should not be used with heat or heating pads. Onset of pain relief is about two to four weeks. Capsaicin is found in overthe-counter creams.
Lidocaine (Lidoderm) is available in a patch formulation for neuropathic pain due to a condition called postherpetic neuralgia. Lidocaine is an anesthetic and numbs the area where it is applied. The patch should be applied to the site of pain, and up to three patches may be applied at a time. The patch should remain in place for twelve hours and then be removed for twelve hours.22
Antidepressant medications are often used in the treatment of neuropathic pain. Tricyclic antidepressants, such as amitriptyline (Elavil), cause pain inhibition by blocking reuptake of norepinephrine and serotonin. Amitriptyline is prescribed at a lower dose for neuropathic pain than for the treatment of depression. Elderly patients are more prone to adverse effects, which include sedation, sweating, sexual dysfunction, nausea, and vomiting. Used more often in younger patients, these medications are typically given at night because they cause sedation. Other antidepressants include selective serotonin reuptake inhibitors (SSRIs) and serotoninnorepinephrine reuptake inhibitors (SNRIs). These work by blocking serotonin and/or norepinephrine, thus enhancing pain inhibition. Common SSRIs include paroxetine (Paxil) and fluoxetine (Prozac). Common SNRIs used include venlafaxine (Effexor) and duloxetine (Cymbalta). Side effects include headache, nausea, diarrhea, insomnia or somnolence, and sexual side effects. These types of antidepressants are not as effective in treating neuropathic pain as the tricyclic antidepressants. Currently, the only antidepressant FDA approved for the treatment of neuropathic pain is duloxetine.23
Another class of medications commonly used includes antiepileptic agents such as gabapentin (Neurontin), pregabalin (Lyrica), carbamazepine (Tegretol), and divalproex (Depakote). Antiepileptics are effective in treating neuropathic pain by decreasing nerve excitability, thus decreasing pain sensations. Common side effects of these medications include dizziness and headaches. Valproic acid may cause liver injury, so liver function tests should be performed periodically. Pregabalin can cause peripheral edema (ankle and leg swelling), so caution should be used in patients with congestive heart failure and hypertension.2
Drugs to Treat Mood Disorders. The drugs used in the treatment of the mood disorders work by altering the various chemicals, called neurotransmitters, found at the nerve junctions in the brain. Norepinephrine, epinephrine, serotonin, and dopamine are examples of neurotransmitters. The following types of drugs are discussed in this section: antidepressants, anti-anxiety (anxiolytics), antipsychotics, sedatives, hypnotics, and stimulants.
Antidepressants. Antidepressants (table 10-7) are divided into several classes based on their chemical structures and chemical actions in the brain. There are many classes of antidepressants, such as tricyclic antidepressants, monoamine oxidase inhibitors (MAOIs), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs). The most frequently used drugs today are the SSRIs. Several of the drugs, such as bupropion (Wellbutrin), nefazodone (Serzone), trazodone (Desyrel), and mirtazapine (Remeron), do not fit into these classifications. All of the antidepressants are effective treatments for depression, and they are also used to treat other conditions, such as anxiety disorders, obsessive-compulsive disorder, posttraumatic stress disorder, pain, and other conditions. Generally, SSRIs, SNRIs, or bupropion (Wellbutrin) are used as an initial treatment choice. The choice of an agent for a patient is dependent on several factors:2
| Classifications and Medications | Available Dosage Forms |
| Tricyclic antidepressants | |
| Amitriptyline (Elavil) | Tablets |
| Nortriptyline (Pamelor) | Capsules |
| Imipramine (Tofranil, Tofranil-PM) | Tablets, capsules |
| Protriptyline (Vivactil | Tablets |
| Desipramine (Norpramin) | Tablets |
| Clomipramine (Anafranil) | Capsules |
| Doxepin (Sinequan) | Capsules |
| MAO-Is | |
| Phenelzine (Nardil) | Tablets |
| Tranylcypromine (Parnate) | Tablets |
| Isocarboxazid (Marplan) | Tablets |
| SSRIs | |
| Fluoxetine (Prozac, Sarafem) | Capsules, tablets |
| Paroxetine (Paxil) | Tablets |
| Sertraline (Zoloft) | Tablets |
| Citalopram (Celexa) | Tablets |
| Escitalopram (Lexapro) | Tablets |
| Fluvoxamine (Luvox) | Tablets |
| SNRIs | |
| Venlafaxine (Effexor, Effexor XR) | Tablets, extended-release tablets |
| Desvenlafaxine (Pristiq) | Tablets |
| Duloxetine (Cymbalta) | Tablets |
| Misc. agents | |
| Trazodone (Desyrel) | Tablets |
| Nefazodone (Serzone) | Tablets |
| Bupropion (Wellbutrin, Wellbutrin-SR Wellbutrin XL, Zyban) | Tablets, extended-release tablets |
| Mirtazapine (Remeron) | Tablets |
 Symptoms the patient is experiencing
Symptoms the patient is experiencing
 Prior medication use
Prior medication use
 Adverse effects
Adverse effects
 Cost
Cost
A rare adverse effect that may occur with these agents is the serotonin syndrome. Any medication that can increase the serotonin level in the body can cause this syndrome. Symptoms include confusion, agitation, fever, hypertension, tachycardia, seizures, and coma.24 Other medications that may increase serotonin levels include triptans, opioid medications such as meperidine (Demerol), and weight loss medications such as sibutramine (Meridia).
Many medications now contain “black box warnings,” which are strong warnings that need to be considered carefully prior to prescribing the medication to a patient. The patient should be carefully monitored for these potential effects during the time they are on the medication. Antidepressant medications contain a black box warning regarding an increased risk of suicidal ideations and behavior. Patients should be monitored for any change in their behavior, mood, or thought processes. During the initial start of an antidepressant medication, the patient should be seen by a health care professional more often to monitor for these potential changes.2 Antidepressants are usually started at low doses and gradually increased. It may take four to six weeks of therapy or more before a patient will respond fully to antidepressants.2 Caution must be used when discontinuing one antidepressant and starting another so that adverse effects are minimized. Antidepressants should be discontinued over a period of several weeks. During this time the dose should be tapered gradually. Drug interactions are common with most antidepressants. Patients should be warned to check with their doctor or pharmacist before taking other prescription or nonprescription medications.
Tricyclic Antidepressants. Tricyclic antidepressants (TCAs) were the most widely used antidepressants for many years and have the recognizable stem of –triptyline on some of their names. The mechanism of action is unclear, but they are thought to enhance the action of norepinephrine, serotonin, and dopamine in the brain. They are effective but have a number of bothersome side effects that include dry mouth, blurred vision, constipation, difficulty urinating, dizziness upon standing, sedation, and sexual dysfunction. These side effects may be so bothersome that patients stop taking their medication.2
There is also a higher risk of patients with preexisting heart disease to have a higher incidence of cardiovascular events. These agents also tend to be more lethal in overdose situations than other antidepressants.25
Monoamine Oxidase Inhibitors (MAO-I). These drugs are thought to work by preventing the natural breakdown of neurotransmitters. MAO-Is are effective antidepressants, but are not commonly used because they have drug-diet interactions with tyramine-containing foods and many drug-drug interactions. If an interaction occurs, hypertensive crisis, an extreme rise in blood pressure that can be fatal or produce organ damage, can occur. Patients must be fully informed of the foods (e.g., aged cheeses, sausages, and red wine) and medications (e.g., pseudoephedrine in decongestants, meperidine [Demerol]) that must be avoided. The most common side effect of MAO-Is is postural hypotension, which is a drop in blood pressure upon rising (moving from a sitting or lying position to a standing position) that results in dizziness.
RX for Success
Pharmacy technicians should always notify the pharmacist when there is a drug interaction alert. The pharmacist will determine the seriousness of the interaction and decide what action to take for the specific patient
Selective Serotonin Reuptake Inhibitors (SSRIs).
The selective serotonin reuptake inhibitors are FDA approved not only for depression, but also for obsessive compulsive disorder (OCD), anxiety, panic disorders, post-traumatic stress disorder, and to help treat the eating disorder bulimia.2 These drugs gained quick acceptance because the side effect profile is more tolerable when compared with the older classes of antidepressants, and the SSRIs are less dangerous in overdose situations.
The side effects that are common with the SSRIs are headache, nausea, anorexia, diarrhea, anxiety, nervousness, and insomnia. Sexual dysfunction occurs frequently.25 Paroxetine (Paxil), fluoxetine (Prozac), and fluvoxamine (Luvox) have the most drug-drug interactions and should be used with caution in patients taking antiarrhythmic agents, TCAs, and phenytoin (Dilantin).25
Serotonin Norepinephrine Reuptake Inhibitors
(SNRIs). The serotonin norepinephrine reuptake inhibitors are potent inhibitors of the reuptake of serotonin and norepinephrine, but work only weakly on dopamine. Like the SSRIs, these agents are better tolerated than some of the other antidepressant medications. Examples include venlafaxine (Effexor) and duloxetine (Cymbalta). Duloxetine is FDA approved for neuropathic pain as well as for the treatment of fibromyalgia. Side effects are similar to those for the SSRIs, but patients should also be monitored for a potential increase in blood pressure.25
Miscellaneous Agents. Nefazodone (Serzone), trazodone (Desyrel), bupropion (Wellbutrin), and mirtazapine (Remeron) do not fit into the usual classes of antidepressants. Nefazodone and trazodone share some of the adverse effects of the tricyclic antidepressants, such as sedation and postural hypotension, but they are less likely to cause heart rhythm disturbances or anticholinergic effects, such as dry mouth, blurred vision, constipation, and difficulty urinating. Trazodone is more often used as a sedative hypnotic agent than for depression. Nefazodone has a high incidence of liver toxicity and is rarely used at this time. Like the tricyclic antidepressants, bupropion (Wellbutrin) can cause constipation and dry mouth, although it does not cause the weight gain that many of the other agents cause. The most serious adverse reaction of bupropion is that it can lower the seizure threshold. Bupropion is unique in that it also approved for smoking cessation and is marketed under the brand name Zyban. Mirtazapine (Remeron) is not likely to cause heart rhythm disturbances or seizures, but it can cause agranulocytosis, a decreased production of all types of blood cells, and neutropenia, a decreased production of white blood cells.2
Drugs for Bipolar Disorder. Bipolar disorder, also called manic-depressive disorder, is characterized by extreme mood swings. Patients cycle between an agitated or overexcited state and a depressed state. Treatment is focused on treating the manic and depressed states, but there is also a maintenance phase that needs to be treated in hopes of controlling the relapses. Manic episodes have traditionally been treated with lithium, although some of the medications in the antiepileptic and atypical antipsychotic classes may also be used (table 10-8).27 Lithium (Lithobid), olanzapine (Zyprexa), and lamotrigine (Lamictal) are appoved to be used as maintenance drugs to prevent relapses.
Table 10–8. Drugs Used to Treat Bipolar Disorder
| Classifications and Medications | Dosage Forms |
| Lithium carbonate (Lithobid) | Capsules,tablets, controlled-release tablets, syrup |
| Antiepileptics | |
| Carbamazepine (Tegretol) | Capsule, suspension, tablets, extended-release tablets |
| Divalproex sodium (Depakote) | Capsule(sprinkle), injection, delayed-release tablets, extendedrelease tablets |
| Oxcarbazepine (Trileptal) | Suspension, tablets |
| Lamotrigine (Lamictal) | Tablets, oral-disintegrating tablets |
| Atypical antipsychotics | |
| Risperidone (Riserdal) | Injection, solution, tablets, oral-disintegrating tablets |
| Olanzapine (Zyprexa) | Injection, tablet, oral-disintegrating tablets |
| Quetiapine (Seroquel) | Tablets, extended release tablets |
| Ziprasidone (Geodon) | Capsules, injection |
| Aripiprazole (Ability) | Injection, solution, tablets, oral-disintegrating tablets |
The mechanism of action of lithium is unclear. Lithium affects many of the salts in the blood, leading to adverse effects such as increased thirst and urination. Other adverse effects include GI problems, fatigue, and weight gain. Tremors are a common side effect of lithium and may be alleviated with propranolol (Inderal). Lithium also decreases thyroid function in a high percentage of patients and may cause kidney toxicity. The amount of lithium in the blood is measured to ensure that the dose is high enough to be effective but still low enough to avoid adverse effects.2
The antiepileptics are often used in patients with “mixed mania” with better results than lithum. This state is when the patient has both manic and depression symptoms occurring at the same time. The antipsychotic agents are often added to lithium or an antiepileptic agent in severe manic phases, or as adjunct therapy in other manic phases if monotherapy is not working for the patient.28
Anti-Anxiety Agents (Anxiolytics). Drugs used for anxiety (anxiolytics) include the SSRIs, benzodiazepines, SNRIs, TCAs, and buspirone (Buspar). Over the years the first-line agents for the treatment of anxiety have changed. Many years ago barbiturates were the preferred class; these agents are rarely, if ever, used anymore. Since then, the benzodiazepines became first-line agents, but those have also fallen out of favor due to their potential for adverse effects and abuse. Currently, the SSRIs are the preferred first-line agents for anxiety disorders.
Benzodiazepines may be used for anxiety or sleep (table 10-9).2 It should be noted that the characteristic ending to the benzodiazepines used for anxiety is -azepam, whereas those that are used for sleep often end in -azolam. Other uses for the benzodiazepines include muscle spasms and seizures. The most common side effects of the benzodiazepines are drowsiness, confusion, slurred speech, and slowed reactions. These effects are enhanced when drugs such as alcohol or narcotics are used simultaneously. All patients taking benzodiazepines should be warned about possible impairment of driving abilities, ability to operate machinery, and judgment. An auxiliary label should be placed on the prescription vial (See figure 10-1).29
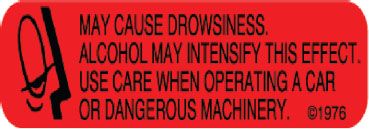
Figure 10-1. An example of a warning label that should be placed on prescription vials containing benzodiazepines.
Withdrawal symptoms can occur when benzodiazepines are taken for a long time and then abruptly stopped. In cases of overdose, a drug called flumazenil (Romazicon) is used as an antidote to reverse some of the effects, such as sedation and respiratory depression.2
Buspirone is chemically different from the benzodiazepines. Its advantage over benzodiazepines is that it is less likely to cause drowsiness and slowed reactions. It also has a low potential for abuse and no withdrawal symptoms. The most common adverse effects seen with this agent are dizziness, nausea, and headaches. Although the benzodiazepines may be used on an as-needed basis for anxiety, it is important to note that buspirone must be taken on a scheduled basis in order to achieve the anti-anxiety effect desired.2
Table 10–9. Agents Used to Treat Anxiety
| Classifications and Medications | Available Dosage Forms |
| Benzodiazepines | |
| Alprazolam (Xanax) | Tablets, intensol solution, extended release tablets, oral-disintegrating tablets |
| Diazepam (Valium) | Injection, intensol solution, solution, tablets |
| Lorazepam (Ativan) | Tablets, injection, intensol solution |
| Clonazepam (Klonopin) | Tablets, oral-disintegrating tablets, wafers |
| Chlordiazepoxide (Librium) | Capsules, injection |
| Clorazepate (Tranxene) | Tablets |
| Non-benzodiazepine | |
| Buspirone (Buspar) | Tablets |
Antipsychotic Agents. Psychosis is a mental disorder in which a person’s capacity to recognize reality is distorted. Schizophrenia is one type of psychosis. Common symptoms include hallucinations (hearing or seeing things that are not real), delusions (fixed beliefs that are false), and thought processes that are not logically connected. Antipsychotic agents are classified as conventional and atypical agents (table 10-10). Although the precise mechanism of action is not known, conventional antipsychotics are thought to act by blocking the action of the neurotransmitter dopamine. The newer agents, classified as atypical or second-generation antipsychotic agents, developed in the 1990s, appear to block not only dopamine, but also serotonin. Orally disintegrating tablets are available for patients who refuse tablets. Fluphenazine decanoate (Prolixin), haloperidol decanoate (Haldol), risperidone (Risperdal Consta), and paliperidone (Invega Sustenna) are available as long-acting injections for patients who may not be compliant with daily medication regimens. The long-acting injections are usually given intramuscularly (IM) every two to four weeks.2
Adverse effects of the antipsychotics differ by classification and potency. The low-potency conventional agents tend to produce more sedation and anticholinergic effects, whereas the high-potency agents produce extrapyramidal effects. Extrapyramidal symptoms (EPS) include abnormal muscle contractions and restlessness. Some muscle contractions can be life-threatening (such as when the throat muscles contract). Anticholinergic side effects include dry mouth, blurred vision, constipation, difficulty urinating, and increased heart rate.30
| Classifications and Medications | Available Dosage Forms |
| Conventional antipsychotics | |
| Chlorpromazine (Thorazine) | Tablets, injection |
| Fluphenazine (Prolixin) | Tablets, injection, liquid, elixir |
| Haloperidol (Haldol) | Tablets, conc. liquid, injection |
| Perphenazine (Trilafon) | Tablets |
| Thioridazine (Mellaril) | Tablets |
| Trifluoperazine (Stelazine) | Tablets |
| Atypical antipsychotics | |
| Aripiprazole (Ability) | Tablets, solution, oral-disintegrating tablets, injection |
| Clozapine (Clozaril) | Tablets |
| Olanzapine (Zyprexa, Zyprexa Zydis) | Tablets, oral-disintegrating tablets, injection |
| Paliperidone (Invega, Invega Sustenna) | Extended-release tablets, long-acting injection |
| Quetiapine (Seroquel) | Tablets, extended-release tablets |
| Risperidone (Risperdal, Risperdal Consta) | Tablets, oral-disintegrating tablets, solution; long-acting injection |
| Ziprasidone (Geodon) | Capsules, injection |
The atypical antipsychotic agents have not been shown to be more effective than the older agents; however, they do tend to have less EPS and may also have some mood stabilizing effects because of their serotonergic effects. Clozapine (Clozaril) was the first agent in this class approved. It has several black box warnings associated with its use, including the potential for agranulocytosis, myocarditis, seizures, and respiratory depression. Patients are required to have their blood drawn every one to four weeks to monitor for a serious condition called agranulocytosis, a decrease in the white blood cell count that could lead to an increase risk of infections and other problems. Newer agents approved after clozapine (Clozaril) do not have this problem.2 The most pronounced adverse effects of the atypical agents is low blood pressure upon standing. Patients should be counseled on rising slowly from a lying or sitting position. Other adverse effects include drowsiness, constipation, weight gain and even increases in cholesterol or glucose levels.30
Sedatives and Hypnotics. Sedative-hypnotic drugs are used for the treatment of sleep disorders (table 10-11). Sedatives are often defined as drugs that reduce anxiety or produce a calming effect. Hypnotic drugs are used to produce sleep or drowsiness. Some drugs have sedative effects at lower doses and hypnotic effects at higher doses.
Hypnotics may be used to treat a variety of sleep problems: difficulty in falling asleep, frequent awakening during the night, early morning awakening, and not feeling rested even after what should be an adequate amount of sleep. Nondrug therapies are usually tried first, such as establishing a regular bedtime and wake-up time and reducing the use of alcohol, caffeine, and nicotine. General guidelines for the use of hypnotics include using the lowest effective dose for the shortest duration possible.31
Hypnotic drugs, like sedatives, include barbiturates, benzodiazepines, and nonbarbiturate, nonbenzodiazepine drugs. Because of their potential for the development of tolerance, fatality in overdose, dependence, withdrawal symptoms, and drug interactions, barbiturates are rarely used as hypnotics.2
Table 10–11. Sedative and Hypnotic Medications
| Classifications and Medications | Available Dosage Forms | Use as Sedative or Hypnotic | |
| Diazepam (Valium) | Injection, intensol solution, solution, tablets | Sedative | |
| Flurazepam (Dalmane) | Capsules | Hypnotic | |
| Midazolam (Versed) | Injection, syrup | Sedative | |
| Temazepam (Restoril) | Capsules | Hypnotic | |
| Triazolam (Halcion) | Tablets | Hypnotic | |
| Estazolam (Prosom) | Tablets | Hypnotic | |
| Quazepam (Doral) | Tablets | Hypnotic | |
| Other agents (nonbenzodiazepines) | |||
| Choral Hydrate | Capsules, syrup, suppository | Sedative | |
| Eszopiclone (Lunesta) | Tablets | Hypnotic | |
| Zaleplon (Sonata) | Capsules | Hypnotic | |
| Zolpidem (Ambien, Ambien CR) | Tablets, extended-release tablets | Hypnotic | |
The effects of some hypnotics carry over into the daytime. This carryover of drowsiness and decreased concentration, called a “hangover effect,” is an important consideration in the use of hypnotics. Elderly patients tend to metabolize drugs at a slower rate, tend to exhibit more confusion and disorientation upon waking, and are at greater risk for falls. Hypnotics with a hangover effect like flurazepam (Dalmane) should be used with caution in these patients. Benzodiazepines that are metabolized and excreted rapidly, such as triazolam (Halcion), are less likely to produce a hangover effect.2 Tolerance, a loss of effectiveness over time, may occur with all benzodiazepines.
Some of the benzodiazepines are used for sedation purposes before procedures in a hospital setting. Injectable forms of midazolam (Versed) and diazepam (Valium) are frequently used for sedation for procedures such as a colonoscopy or minor surgical procedures. Amnesia, or memory loss, is an adverse effect but is desirable when these drugs are used for sedation during painful medical procedures.2
Nonbenzodiazepine hypnotics have the ability to induce sleepiness and/or to reduce the number of nighttime awakenings; that is, they may help the patient fall asleep and/or stay asleep. Zolpidem (Ambien) has the ability to help patients fall asleep and stay asleep for six to eight hours. Zaleplon (Sonata) has a fast onset of action, which allows patients to fall asleep quickly, but because it does not last long, it may not assist patients who tend to wake up in the middle of the night. Eszopiclone (Lunesta) also allows patients to fall asleep quickly, and it increases total sleep time and sleep quality.31
Other classes of medications may also be used as hypnotics because drowsiness is one of their most common side effects. The antihistamine diphenhydramine is found in many over-the-counter (OTC) sleep aids, such as Tylenol PM, which also contains acetaminophen. Although diphenhydramine effectively causes drowsiness, some patients may experience a hangover effect the next day and should use caution. Antidepressants such as amitriptyline and trazodone are sometimes used for patients who have depression and difficulty sleeping.
Drugs to Treat Attention Deficit Hyperactivity Disorder (ADHD). ADHD is a common childhood psychiatric disorder that affects behavioral, social, and emotional function and the development of the child.32 There is no cure and up to 75% of the children still suffer from ADHD into adulthood.33 ADHD is thought to occur due to a deficiency of norepinephrine and dopamine. Norepinephrine is thought to affect attention and mood while dopamine is thought to influence behavior and impulsivity.32 Overall treatment consists of behaviormodification and pharmacotherapy.33
Table 10–12. Agents to Treat ADHD
| Classifications and Medications | Available Dosage Forms |
| Stimulants | |
| Dexmethylphenidate (Focalin) | Tablets, extended-release capsules |
| Dextroamphetamine (Dexedrine) | Tablets, extended-release capsules, solution |
| Lisdexamfetamine (Vyvanse) | Capsules |
| Methylphenidate (Ritalin, Metadate, Methylin, Concerta, Daytrana) | Tablets, extended-release tablets, capsules, patch |
| Mixed amphetamine salts (Adderall, Adderall XR) | Tablets, extended-release capsules |
| Non-stimulants | |
| Atomoxetine (Strattera) | Capsules |
Several classes of medications may be used in the treatment of ADHD. First-line therapy includes the stimulants (table 10-12). If these don’t work or are contraindicated, the patient may be switched to atomoxetine (Strattera), bupropion (Wellbutrin), venlafaxine (Effexor), or other psychotropic medications.2
The stimulants are thought to work by increasing the release of norepinephrine and dopamine and blocking the reuptake of these neurotransmitters. The immediate release agents are typically dosed two to three times a day. Twice daily dosing is given in the morning and at lunch; if dosed three times daily, a dose is also given after school. Doses are given early in the day so the medication does not interfere with sleep at night.32
In recent years, longer-acting formulations have been developed that allow for once-daily dosing. The methylphenidate (Daytrana) patch is worn for nine hours a day and allows for continuous administration of the medication during that time period.32 Lisdexamfetamine (Vyvanse) is a prodrug of dextroamphetamine, meaning that it has no action until it is converted to dextroamphetamine by the liver. By delaying its action, it is possible to lessen adverse effects as well as reduce the potential for abuse and toxicity.33
Adverse effects with the stimulants include headache, decreased appetite, nausea, insomnia, and increased blood pressure or heart rate. With the patch, skin irritation and rash may occur. To help prevent long-term adverse effects in children, “drug holidays” are often done, in which the drugs are not taken on weekends and/or during the summer or other breaks when the child is not in school.32,33
The nonstimulant medication atomoxetine (Strattera) blocks the reuptake of norepinephrine in the brain. It is taken once or twice a day on a regular basis with no “drug holidays.” Atomoxetine has a black box warning regarding the possibility of suicidal ideations and behavior in adolescents. The adverse effects are similar to those of the stimulant medications and it has an additional warning regarding possible increase in liver enzymes.2
Drugs that Affect the Cardiovascular System
Cholesterol-lowering Agents. Cholesterol and triglycerides are the fats implicated in heart disease. Cholesterol is measured as total cholesterol, which is a combination of low density lipoprotein (LDL), the so-called “bad” cholesterol, and high density lipoprotein (HDL), the “good” cholesterol. Ideally, drugs should be able to reduce LDL levels and/or increase HDL levels. Current drugs have differing effects on these various components of blood cholesterol and triglycerides (TG). Drugs are selected based on the type of fats that are elevated as well as the side effect profiles of the drugs.
Initially, high cholesterol is treated with diet and exercise. If these methods fail, drugs often are added (table 10-13). These agents, called antihyperlipidemics, may be used alone or in combinations to lower cholesterol. Some of the agents have been combined into single dosage forms to improve patient compliance. When initiating pharmacologic therapy, the main lipid targeted is LDL. High levels of LDL are a main cause of clogged arteries, also known as coronary artery disease (CAD). Patients should have their cholesterol levels checked after six to twelve weeks, and medication is adjusted if needed. Once patients are stabilized on a lipid regimen, they should continue to have their levels checked every four to six months.34
HMG-CoA Reductase Inhibitors. The HMG-CoA reductase inhibitors, also known as “statins,” prevent the formation of cholesterol from fats in the liver and are often considered first-line therapy for lowering LDL. They decrease LDL and increase HDL, as well as decrease total cholesterol and triglycerides. The most common side effects are muscle and joint pain, headache, and gastrointestinal distress. The most serious effects include abnormalities of liver function tests, although liver damage does not usually occur. A more serious muscle disease, rhabdomyolysis, can occur, usually in patients taking high doses or in combination with the fibrates and possibly other drugs. Pravastatin (Pravachol) is the agent that has the fewest drug-drug interactions associated with its use; the other agents, although differing in potency, are similar with respect to drug interaction potential and adverse effects.2
Table 10–13. Cholesterol Lowering Agents
| Classifications and Medications | Available dosage forms |
| Bile acid sequestrants | |
| Cholestyramine (Questran) | Powder, packets |
| Colestipol (Colestid) | Granules, packets, tablets |
| Colesevelam (Welchol) | Tablets |
| HMG-CoA reductase inhibitors (statins) | |
| Atorvastatin (Lipitor) | Tablets |
| Fluvastatin (Lescol) | Capsules, extended-release tablets |
| Lovastatin (Mevacor) | Tablets |
| Pravastatin (Pravachol) | Tablets |
| Simvastatin (Zocor) | Tablets |
| Rosuvastatin (Crestor) | Tablets |
| Fibrates | |
| Gemfibrozil (Lopid) | tablets |
| Fenofibrate, fenofibric acid (Antara, Fenoglide, Lofibra, Lipofen, Triglide, Trilipix,Tricor) | Tablets, capsules |
| Misc. and combination agents | |
| Amlodipine/atorvastatin (Caduet) | Tablets |
| Ezetimibe (Zetia) | Tablets |
| Ezetimibe/Simvastatin (Vytorin) | Tablets |
| Niacin/lovastatin (Advicor) | Tablets |
| Niacin/simvastatin (Simcor) | Tablets |
| Nicotinic acid (Niacin, Niaspan) | Tablets, capsules, sustained-release capsules |
| Omega-3 fatty acids (Lovaza) | Capsules |
Bile Acid Sequestrants. Bile aids the absorption of fats in the intestines. The bile secreted into the intestine is reabsorbed back into the blood. The body uses cholesterol to make more bile, which is then bound and excreted; this cycle leads to a decrease in LDL and total cholesterol. Bile acid sequestrants bind the bile in the intestines and prevent it from being reabsorbed. Instead, it is excreted in the feces. The most common side effects with these drugs are constipation, aggravation of hemorrhoids, abdominal cramping, gas, nausea, vomiting, diarrhea, and heartburn.
Tablet forms of these drugs are available, but for convenience, these drugs are also available as powders to be mixed in juice or water. If enough fluid is not given with the bile acid sequestrants, they can form a solid mass in the esophagus or the intestines, resulting in blockage of these parts of the digestive tract. Patients often complain that these formulations are not very palatable and are gritty when in liquid.
In the same way that these drugs bind bile acids, they can also bind other medications. Other drugs should be taken one hour before or four to six hours after the bile acid sequestrants. Because of these drawbacks, the bile acid sequestrants are used infrequently.34
Fibrates. Fibrates lower LDL and raise HDL, and are very useful for their triglyceride-lowering effects. The mechanism of action is unknown. The most common side effects are nausea and other gastrointestinal symptoms, muscle and joint aches, skin rash, fatigue, taste disturbances, and weakness. More serious effects include a possible increased risk of liver cancer, gallstones, and decreased white and/or red blood cells.2
Other Lipid-lowering Agents. Ezetimibe (Zetia) works in the intestines to decrease the absorption of cholesterol. It may be used as monotherapy, but is more often used in conjunction with other cholesterol lowering agents to lower LDL and triglycerides and raise HDL. The most common adverse effects include back and joint pain, GI problems, and an increase in liver function tests and hepatotoxicity.2
Nicotinic acid (Niacin, Niaspan) is a form of vitamin B that reduces serum cholesterol and triglycerides. Another form of this vitamin, nicotinamide (niacinamide), does not affect blood cholesterol levels. Niacin is beneficial in lowering triglyceride (TG) levels, is the best agent available in raising HDL levels, and has a lesser effect on lowering LDL. The most bothersome adverse effect of niacin is a flushing sensation or a feeling of warmth, as well as itching, tingling, or headache. An aspirin tablet thirty minutes before the niacin dose can alleviate this effect. GI upset can also occur. Using a sustained release formulation can also alleviate these bothersome effects. Niacin may also raise blood sugar levels and needs to be used with caution in patients with diabetes. More serious effects include abnormal liver function tests, which tend to occur with high doses and with the sustained-release products.2
Omega-3 fatty acids (Lovaza), commonly found in fish oil, have been shown to reduce triglyceride levels in patients with very high triglycerides in their blood (hypertriglyceridemia). Although there are over-the-counter versions of fish oils available, they are not approved by the FDA and are not standardized to ensure the proper amount of the ingredient is in the product. The most common side effects of the fish oils are fishy taste and fishy burps, GI upset, and increased liver function tests. These agents may also increase bleeding time, so patients who are receiving anticoagulation therapy need to be monitored closely.2
High Blood Pressure Agents (Antihypertensives). There are many classes of drugs used to treat high blood pressure. Diuretics and beta-blockers have been shown in clinical studies to reduce the risk of death from heart attacks and strokes. Angiotensin-converting enzyme inhibitors (ACE inhibitors), angiotensin receptor blockers (ARBs), and calcium channel blockers are other drugs that have advantages in certain types of patients. Central alpha2-agonists, peripheral adrenergic antagonists, and direct vasodilators are other agents that are available, although they are used when the other agents have failed.35
Diuretics. Diuretics decrease blood pressure by decreasing the blood volume. They are commonly called “water pills” and work on the kidneys to increase urinary excretion of sodium, chloride, and water. Since all diuretics increase urination, they should be taken as early in the day as possible so that urination does not interrupt the patient’s sleep.35
There are three types of diuretics used to treat hypertension (table 10-14): thiazides, loop diuretics, and potassium-sparing diuretics. Thiazide diuretics (e.g., hydrochlorothiazide) in low doses are usually effective for high blood pressure. Loop diuretics (e.g., furosemide [Lasix]) are more effective in patients with mild kidney failure. Both the thiazide and loop diuretics can decrease potassium in the body, and patients may need to take potassium supplements. Potassium-sparing diuretics are weak diuretics but are often added to other diuretics (e.g., triamterene/hydrochlorothiazide [Dyazide]) to prevent potassium loss.2
| Classifications and Medications | Available Dosage Forms |
| Thiazide diuretics | |
| Hydrochlorothiazide – HCTZ (Microzide) | Capsules, tablets |
| Chlorothiazide (Diuril) | Injection, suspension, tablets |
| Metolazone (Zaroxolyn) | Tablets |
| Loop diuretics | |
| Furosemide (Lasix) | Injection, solution, tablets |
| Bumetanide (Bumex) | Injection, tablets |
| Torsemide (Demadex) | Injection, tablets |
| Ethacrynic acid (Edecrin) | injection |
| Potassium-sparing diuretics | |
| Eplerenone (Inspra) | Tablets |
| Spironolactone (Aldactone) | Tablets |
| Triamterene (Dyrenium) | Capsules |
| Combination agents | |
| Triamterene/HCTZ (Dyazide, Maxzide) | Tablets, capsules |
| Spironolactone/HCTZ (Aldactazide) | Tablets |
Although the thiazide diuretics are well tolerated by patients, certain precautions should be noted. Blood glucose control in patients with diabetes may be altered by thiazide diuretics. Patients who are taking thiazide diuretics may be more sensitive to sun, so they should be warned to avoid exposure or use sunscreen (See figure 10-2). Patients allergic to sulfonamides may also be allergic to thiazide diuretics.2
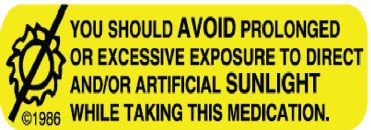
Figure 10-2. A warning label that should be placed on prescription vials containing thiazide diuretics.
Loop diuretics are more potent diuretics and may affect electrolytes such as sodium, potassium, chloride, calcium, and magnesium to a greater degree than the thiazides. Adverse effects are similar to those of the thiazides, including altered blood glucose control in diabetics, sun sensitivity, and allergic reactions in sulfonamide-allergic patients. Ethacrynic acid (Edecrin) does not contain a sulfa group, so it may be used in patients allergic to sulfonamides.35
Potassium-sparing diuretics used alone do not cause potassium loss like the other diuretics. In fact, they may increase potassium levels in patients and should be used with caution in patients using ACE inhibitors, or other medications that may increase potassium levels. Potassium-sparing diuretics are often used with other diuretics to combine the greater potency of a loop or thiazide diuretic with their potassium-sparing effects.2 Some diuretics have been combined with other diuretics or antihypertensive drugs to make convenient dosage forms.
Beta-blockers. Beta-blockers block the action of certain nerves in cardiac muscle, lungs, and the smooth muscles of the blood vessels. There are two types of beta receptors: β1-receptors are found in the heart and kidney, and β2-receptors are found in the lungs, arterioles, pancreas, and liver. When the β1-receptors are stimulated, there is an increase in heart rate and contractility. When the β2-receptors are stimulated, vasodilation and bronchodilation occur. Beta-blockers lower blood pressure by decreasing the volume of blood pumped by each contraction of the heart, thus slowing heart rate; however, they may also cause bronchoconstriction.2
Beta-blockers are further classified as cardioselective if they are more selective for the receptors in the heart (β1), or noncardioselective (β1 and β2). They typically have an –olol ending (table 10-15). Because beta-blockers may constrict the airways, they should be used with caution in patients with asthma or COPD; however, agents that are cardioselective are a better choice for these patients since there should be little to no β2-receptor stimulation. Beta-blockers are first-line drugs for the treatment of hypertension and, like diuretics, have been shown to reduce the risk of death from heart attack or stroke. They may be used in the treatment of other conditions, including angina, abnormal heart rhythms, prevention of heart attack, prevention of migraine headache, and tremor.35
Beta-blockers also block the symptoms of low blood sugar and should be used cautiously in patients with diabetes. Undesirable side effects include central nervous system effects such as dizziness, tiredness, and depression. Some patients may develop tingling, loss of sensation, or intolerance to cold in the hands and feet.2
| Medications | Cardioselective or Nonselective | Available Dosage Forms |
| Atenolol (Tenormin) | Cardioselective | Tablets |
| Bisoprolol (Zebeta) | Cardioselective | Tablets |
| Carvedilol (Coreg) | Nonselective | Tablets |
| Labetalol (Trandate) | Nonselective | Tablets, injection |
| Metoprolol tartrate (Lopressor) | Cardioselective | Injection, tablets |
| Metoprolol sodium succinate (Toprol-XL) | Extended-release tablets | |
| Nadolol (Corgard) | Nonselective | Tablets |
| Nebivolol (Bystolic) | Cardioselective | Tablets |
| Propranolol (Inderal LA) | Nonselective | Solution, extended-release capsules, tablets, injection |
| Sotalol (Betapace) | Nonselective | Tablets |
| Combination agents | ||
| Bisoprolol/HCTZ (Ziac) | Cardioselective | Tablets |
| Metoprolol/HCTZ (Lopressor HCT) | Cardioselective | Tablets |
| Atenolol/chlorthali-done (Tenoretic) | Cardioselective | Tablets |
ACE Inhibitors and Angiotensin Receptor Blockers (ARBs). Angiotensin-converting enzyme inhibitors (ACE inhibitors) prevent the production of certain chemicals in the blood that cause the constriction of blood vessels and retention of sodium and water. By blocking blood vessel constriction and salt and water retention, these drugs can lower blood pressure. Like the betablockers, they have other uses. ACE inhibitors may slow or prevent the development of kidney disease in diabetic patients and increase survival, alleviate symptoms, and decrease hospitalization in patients with heart failure.2 The ACE inhibitors have a –pril ending on the name (table 10-16).
A unique side effect of the ACE inhibitors that may lead to discontinuation of the drug is a bothersome dry cough. Some patients experience dizziness when they begin therapy. ACE inhibitors can also cause skin rashes, abnormal taste in the mouth, and high potassium levels.35
The angiotensin receptor blockers (ARBs) lower blood pressure in the kidneys by blocking the angiotensin II receptors and blood vessel constriction. These agents tend to have a –sartan ending on the generic names. The side effects are similar to those of the ACE inhibitors except there is less incidence of dry cough.2
Table 10–16. ACE Inhibitors and ARBs
| Classifications and Medications | Available Dosage Forms |
| ACE-Inhibitors (ACE-Is) | |
| Benazepril (Lotensin) | Tablets |
| Captopril (Capoten) | Tablets |
| Enalapril, enalaprilat (Vasotec) | Injection, tablets |
| Fosinopril (Monopril) | Tablets |
| Lisinopril (Prinivil, Zestril) | Tablets |
| Moexipril (Univasc) | Tablets |
| Quinapril (Accupril) | Tablets |
| Perindopril (Aceon) | Tablets |
| Ramipril (Altace) | Capsules, tablets |
| Trandolapril (Mavik) | Tablets |
| Angiotensin II receptor blockers (ARBs) | |
| Candesartan (Atacand) | Tablets |
| Eprosartan (Teveten) | Tablets |
| Losarían (Cozaar) | Tablets |
| Irbesartan (Avapro) | Tablets |
| Olmesartan (Benicar) | Tablets |
| Telmisartan (Micardis) | Tablets |
| Valsartan (Diovan) | Tablets |
| Combination products | |
| Amlodipine/olmesartan (Azor) | Tablets |
| Amlodipine/valsartan (Exforge) | Tablets |
| Amlodipine/valsartan/HCTZ (Exforge HCT) | Tablets |
| Benazepril/HCTZ (Lotensin HCT) | Tablets |
| Candesartan/HCTZ (Atacand HCT) | Tablets |
| Enalapril/HCTZ (Vaseretic) | Tablets |
| Eprosartan/HCTZ (Teveten HCT) | Tablets |
| Irbesartan/HCTZ (Avalide) | Tablets |
| Lisinopril/HCTZ (Zestoretic) | Tablets |
| Losartan/HCTZ (Hyzaar) | Tablets |
| Moexipril/HCTZ (Uniretic) | Tablets |
| Olmesartan/HCTZ (Benicar HCT) | Tablets |
| Quinapril/HCTZ (Accuretic) | Tablets |
| Ramipril/HCTZ (Altace HCT) | Tablets |
| Telmisartan/HCTZ (Micardis HCT) | Tablets |
| Trandolapril/verapamil (Tarka) | Tablets |
| Valsartan/HCTZ (Diovan HCT) | Tablets |
Calcium Channel Blockers. The movement of calcium in and out of cells is essential for nerve conduction and muscle contraction. Calcium channel blockers inhibit this movement, resulting in a decreased force of contraction of the heart, blocked contraction of smooth muscle in the blood vessels resulting in dilation of blood vessels, and slowed conduction of nerve impulses throughout the heart resulting in a slowed heart rate. The drugs in this class vary in the selectivity of their actions on heart rate, blood vessel dilation, and heart contraction.2
Calcium channel blockers are used for chest pain (angina pectoris), heart rhythm disturbances, migraine headache, and diseases of the heart muscle. One drug, nimodipine, has a special indication for reducing nerve damage caused by bleeding in the brain, which is called subarachnoid hemorrhage. Nimodipine is not used for hypertension.2
The drugs in this class are listed in table 10-17. In general, these drugs have similar side effects. Drugs such as diltiazem (Cardizem) and verapamil (Calan, Verelan) are more efficacious in patients with arrhythmias, and have constipation and slow heart rate as adverse effects associated with their use. The other calcium channel blockers tend to be used more often for hypertension, and the adverse reactions of these agents include dizziness, headache, constipation, and, occasionally, swelling of the legs or feet.35
The immediate release formulations of this class are indicated for use in patients with chest pain. Many of these agents have sustained-release formulations available which are indicated for the treatment of high blood pressure allowing for once or twice daily dosing, which increases patient compliance.
Vasodilators. The alpha-2 agonists, direct renin inhibitors, and direct vasodilators are other classes of drugs used to treat high blood pressure. They act through various effects on nerve pathways to dilate the blood vessels and reduce blood pressure. Aliskiren (Tekturna) inhibits the enzyme renin, which is produced by the kidney, and can cause the blood vessels to constrict.36 Because these drugs block the ability of blood vessels to constrict, people who take them often get dizzy or feel faint when they stand up after sitting or sit up after lying down, which is referred to as postural hypotension. Because of the high incidence of side effects with the alpha-2 agonists and direct vasoilators, these agents are not often used.
Table 10–17. Calcium Channel Blockers
| Medications | Available Dosage Forms |
| Amlodipine (Norvasc) | Tablets |
| Nifedipine (Procardia, Adalat CC) | Capsules, extended-release tablets |
| Felodipine | Tablets |
| Isradipine (DynaCirc) | Capsules, tablets |
| Nicardipine (Cardene) | Capsules, sustained-release capsules, injection |
| Nislodipine (Sular) | Extended-release tablets |
| Clevidipine (Cleviprex) | Injection |
| Nimodipine (Nimotop) | Capsules |
| Diltiazem (Cardizem, Tiazac) | Extended-release capsules, injection, tablets, extended-release tablets |
| Verapamil (Calan, Verelan) | Sustained-release caplets, extended-release capsules, injection, tablets |
| Combination agents | |
| Amlodipine/atorvastatin (Caduet) | Tablets |
| Amlodipine/benazepril (Lotrel) | Tablets |
| Amlodipine/olmesartan (Azor) | Tablets |
| Amlodipine/valsartan (Exforge) | Tablets |
| Amlodipine/valsartan/HCTZ (Exforge HCT) | Tablets |
| Trandolapril/verapamil (Tarka) | Tablets |
The alpha-2 agonists include clonidine (Catapres) and methyldopa. Common side effects, in addition to postural hypotension, are drowsiness, sedation, dry mouth, and fatigue. Clonidine is available as a patch that is changed weekly. The Catapres-TTS® patch system consists of an active patch containing drug and an inactive overlay; both patches must be dispensed.
The direct vasodilators hydralazine and minoxidil can cause headache, rapid heartbeat, and fluid retention. Minoxidil was found to increase the growth of body hair in patients and is now available as a topical product (Rogaine®) for stimulating hair growth in people with balding or thinning hair.
Nitrates. Angina pectoris is chest pain of short duration that is due to a lack of oxygen in the cardiac muscle cells. The pain subsides when the imbalance between the amount of oxygen needed by the cells and the amount of oxygen supplied to the cells is corrected. The nitrates are the most commonly used medicines for treating angina pectoris. Nitrates increase the amount of oxygen delivered to the heart and decrease the oxygen needs of the heart. They also dilate the arterial and venous blood vessels.2 Nitrates are available in many dosage forms. For acute attacks, sublingual tablets or a translingual (on or under the tongue) spray is used. Nitroglycerin is available as an intravenous infusion. The oral sustained-release tablets and capsules, topical ointment, and transdermal patches are used for prevention of angina. Other classes of drugs that may be used for prevention of angina are the betablockers and the calcium channel blockers, which are discussed in other sections of this chapter. The nitrates available are nitroglycerin, isosorbide dinitrate (Isordil), and isosorbide mononitrate (Ismo, Imdur).2
An important concern in choosing dosage forms and dosage regimens for nitrates is the development of tolerance. After twenty-four hours of continuous therapy, nitrates no longer work. Increasing the dose does not restore efficacy, but a nitrate-free period does. For this reason, nitrates are not usually dosed around the clock. Long-acting tablets and capsules may be given orally once daily or twice daily at 8:00 a.m. and 2:00 p.m. Isosorbide mononitrate regular release is frequently given as two doses seven hours apart during the day. Nitroglycerin patches are often applied in the morning and removed at night. All of these schedules provide a nitrate-free period at night.
Common side effects of nitrates include headaches, postural hypotension, dizziness, or flushing. Headache may be an indicator of the drug’s activity and may be treated with aspirin or acetaminophen.2
Digoxin. As with many cardiac diseases, diet modification is part of the treatment for heart failure. Fluid restriction and a low sodium diet are often prescribed to reduce the amount of fluid retention. Drug therapy includes several types of drugs: ACE inhibitors, diuretics, betablockers, and cardiac glycosides (digoxin). The choice of drugs is based on the severity of disease and the patient’s symptoms.35
The role of digoxin is not well defined presently, but it has been shown to increase the force of heart muscle contraction in selected patients.2 Digoxin acts on both the heart muscle and the nerve conduction system of the heart. It decreases the rate and force of heart muscle contractions, resulting in improved pumping of blood and a slower heart rate.2
Digoxin has a narrow therapeutic index and can have serious toxicities. Therefore, digoxin blood levels are monitored to help ensure safe dosing. Patients and caregivers should be aware of the early symptoms of toxicity: loss of appetite, nausea, vomiting, diarrhea, headache, weakness, confusion, and visual disturbances (particularly blurred vision, yellow or green vision, or a halo effect). An antidote, digoxin immune fab (Digibind, DigiFab), is administered intravenously to treat lifethreatening digoxin intoxication.2
Digoxin is available as an injection, a tablet, and an elixir. The amount absorbed from the different preparations varies, so the dose may need to be adjusted when dosage forms are switched.
Antiarrhythmics. Common arrhythmias (irregular heartbeats or abnormal heart rhythms) include atrial fibrillation, atrial flutter, and premature ventricular contractions. Rare but serious arrhythmias include ventricular tachycardia, ventricular fibrillation, and torsades de pointes. Many of the drugs used to treat arrhythmias can also cause arrhythmias (table 10-18). Common side effects, which may be severe, are GI disturbances such as nausea, vomiting, abdominal pain, and diarrhea. Some beta-blockers, calcium channel blockers, and digoxin are also used to treat arrhythmias.2
Class I antiarrythmic drugs, quinidine and disopyramide (Norpace), are used for both atrial and ventricular arrhythmias. Quinidine is given by IM or IV injection or orally. Disopyramide (Norpace) is given orally. Side effects include dry mouth, difficulty urinating, dizziness, constipation, and blurred vision. The most serious side effects are low blood pressure and heart failure.22
Another subset of class I antiarrhythmics, class IB, includes lidocaine (Xylocaine) and mexilitine (Mexitil). Class IB drugs are useful for ventricular arrhythmias. Lidocaine is given intravenously. Its side effects are related to its effects on the central nervous system: dizziness, confusion, mood changes, hallucination, drowsiness, vision disturbances, muscle twitching, and seizures. The side effects of mexilitine are similar to those of lidocaine.
Flecainide (Tambocor) and propafenone (Rythmol) are class IC antiarrhythmics. These drugs are now used only to treat life-threatening ventricular arrhythmias and some life-threatening atrial arrhythmias. Propafenone is also used to treat atrial fibrillation. Both of these drugs are available only as oral dosage forms and have mild side effects that are similar: dizziness, tremor, and blurred vision.22
Table 10–18. Antiarrhythmic Agents
| Class | Medications | Available Dosage Forms |
| IA | Qulnldlne | Tablets, injection |
| Procalnamlde (Pronestyl, Procanbld) | Tablets, capsules, injection | |
| Dlsopyramlde (Norpace) | Capsules | |
| IB | Lldocalne (Xylocalne) | Injection |
| Mexlletlne (Mexitil) | Capsules | |
| IC | Flecalnlde (Tambocor) | Tablets |
| Propafenone (Rythmol) | Tablets, capsules | |
| Morlclzlne (Ethmozlne) | Tablets | |
| II | Atenolol (Tenormln) | Tablets |
| Esmolol (Brevlbloc) | Injection | |
| Metoprolol (Lopressor, Toprol XL) | Tablets, injection | |
| Propranolol (Inderal) | Tablets, capsules, oral solution, injection | |
| III | Amlodarone (Pacerone) | Tablets, injection |
| Dofetlllde (Tlkosyn) | Capsules | |
| Ibutlllde (Corvert) | Injection | |
| Sotalol (Betapace) | Tablets, injection |
The class III antiarrhythmics include amiodarone (Pacerone) and sotalol (Betapace). They are used to treat ventricular arrhythmias as well as atrial fibrillation. Adverse reactions are common with amiodarone. A unique side effect with amiodarone is a bluegray discoloration of the skin, which is irreversible. Other side effects are visual disturbances, increased sensitivity to sunlight, fatigue, tremor, and changes in thyroid gland function. More serious side effects are microdeposits in the cornea of the eye resulting in visual halos or blurred vision, lung toxicity, and liver toxicity. Amiodarone is available both orally and intravenously, and dosing of both forms involves an initial loading dose followed by a lower maintenance dose. Sotalol is a beta-blocking drug with antiarrhythmic properties similar to those of amiodarone.2
Drugs that Affect the Respiratory System
Two common diseases of the respiratory system are asthma and chronic obstructive pulmonary disease (COPD). Asthma is a condition in which there is a reversible narrowing of the air passages caused by overresponsiveness of the airways to various stimuli and inflammation of the airways. Examples of stimuli that can cause inflammation and airway narrowing include viruses, cold air, exercise, pollens, dust, cigarette smoke, and animal dander. Chronic obstructive pulmonary disease is an irreversible chronic obstruction of the airways. Emphysema and chronic bronchitis are examples of COPD. The symptoms of asthma and COPD are similar: wheezing, difficulty breathing, and coughing. These diseases differ in their cause, development, and reversibility. The agents discussed in this section may be used to treat both asthma and COPD.

Figure 10-3. Three examples of available dosage forms for bronchodilators such as beta2-agonists.
Bronchodilators. Medications that work to open up the airways and make it easier to breathe are called bronchodilators. There are three types of bronchodilators: beta2-agonists, anticholinergics, and methylxanthines (table 10-19).
The beta2-agonists are bronchodilators that act by relaxing the smooth muscles in the bronchial airways. These agents are available in several dosage forms: oral tablets and liquids, inhalers (metered-dose [MDI], HFA, dry powder [DPI]), and solutions for inhalation via a nebulizer machine (see figure 10-3).
Most patients use inhalers or nebulizer forms. By delivering the medication directly to the lungs, the patient is able to feel relief quicker and there is less systemic absorption of the medication, leading to fewer adverse effects. The proper use of inhalers is critical to the success of treatment with these drugs. An important patient counseling point should always include proper use of inhalers.40
Common side effects of beta2-agonists are a rapid heartbeat, tremors, anxiety, and nausea. Most of these side effects will lessen as the body adjusts to the medication. Overuse of beta2-agonists can result in decreased effectiveness of the agents. Beta2-agonists differ in their duration of action. Short-acting beta2-agonists (e.g., albuterol, levalbuterol) work quickly and are used to stop an attack, whereas long-acting beta2-agonists (e.g., salmeterol, formoterol) are used on a daily basis to prevent attacks.
Epinephrine and ephedrine are drugs that produce bronchodilation similar to the beta2 agonists, but they are not specific for the lungs and also affect the heart. This lack of selectivity increases the number of side effects, including an increase in heart rate and blood pressure. Overuse of these products has led to death in some patients. Epinephrine (Primatene Mist) and ephedrine/guaifenesin (Primatene Tablets) are available in overthe-counter formulations but should not be used without medical supervision.41
Table 10–19. Agents to Treat Asthma and COPD Classifications and
| Classifications and Medications | Available Dosage Forms |
| Short-acting bronchodilators | |
| Albuterol (Proventil, Ventolín, ProAir) | Inhaler, nebulizer solution, extended-release tablets, oral liquid |
| Levalbuterol (Xopenex) | Inhaler, nebulizer solution |
| Pirbuterol (Maxair) | Inhaler |
| Metaproterenol (Alupent) | Syrup |
| Long-acting bronchodilators | |
| Salmeterol (Serevent) | Inhaler |
| Formoterol (Foradil) | Inhaler |
| Methylxanthines | |
| Theophylline (Theo-24, Uniphyl, Theochron) | Injection, elixir, extendedrelease capsules/tablets |
| Aminophylline | Injection, tablets |
| Mast cell stabilizers | |
| Cromolyn sodium (Intal) | Inhaler, nebulizer solution |
| Anticholinergics | |
| Ipratropium (Atrovent) | Inhaler, nebulizer solution |
| Tiotropium (Spiriva) | Inhaler |
| Leukotriene modifiers | |
| Zafirlukast (Accolate) | Tablets |
| Montelukast (Singulair) | Chewable tablets, tablets, granules |
| Zileutin (Zyflo, Zyflo CR) | Tablets, extended-release tablets |
| Combination agents | |
| Salmeterol/fluticasone (Advair) | Inhaler |
| Formoterol/budesonide (Symbicort) | Inhaler |
| Ipratropium/albuterol (Combivent, Duoneb) | Inhaler, nebulizer solution |
Anticholinergic drugs (e.g., ipratropium, tiotropium) are also bronchodilators. These drugs also relax the muscles in the airways. The anticholinergic drugs are more useful in COPD than in asthma. They have a longer duration of action than the beta2-agonists, and because of their anticholinergic “drying” effects, they can help to dry the excess mucus production that occurs in patients with COPD. Combined use with a beta2-agonist may increase the benefit. Common side effects include dizziness, headache, nausea, dry mouth, cough, hoarseness, or blurred vision.2
The methylxanthines are another class of bronchodilators. The exact mechanism of action of these drugs is not known but may be related to an anti-inflammatory effect. The most common methylxanthines are theophylline and aminophylline. Aminophylline is a salt of theophylline. If theophylline is substituted for aminophylline, the dose should be 80% of the aminophylline dose.18
Theophylline has a high incidence of side effects that often occur at therapeutic doses. Nausea and vomiting are common. Other side effects include irritability, restlessness, headache, insomnia, muscle twitching, and rapid heartbeat. Age, diet, smoking, other medications, and illnesses are all factors that can change the amount of theophylline a patient needs to achieve and maintain therapeutic blood concentrations. Blood levels are measured periodically to ensure that patients achieve and maintain therapeutic concentrations. Due to the monitoring and side effect profile, the xanthines are no longer commonly used.40
Corticosteroids. Corticosteroids are commonly used to suppress inflammation and the immune response, and are useful in a wide spectrum of diseases including asthma, allergic reactions, lupus, ulcerative colitis, psoriasis, rheumatoid arthritis, bursitis, and organ transplantation.
The inhaled route of administration is useful in pulmonary diseases to provide local effects and prevent the numerous side effects these drugs can cause when given orally (table 10-20). Inhaled corticosteroids were previously avoided in children due to reports that they affect growth. More recent studies have disproven this theory, and current guidelines support the use of corticosteroids in children to control asthma. The most common side effects of inhaled corticosteroids include thrush (fungus of the throat and mouth) and hoarseness. These effects can be prevented by using a spacer device with the inhaler and rinsing the mouth with water after use. Ciclosenide (Alvesco) is a new inhaled corticosteroid that is activated by the tissues in the lungs. Since the drug is not active when inhaled, it is thought to reduce the incidence of oral thrush in patients.18 Oral corticosteroids are often used to treat exacerbations and may be required on a regular basis in patients with severe asthma.40
Table 10–20. Oral/Inhaled Corticosteroids
| Medications | Available Dosage Forms | Comments |
| Oral corticosteroids | ||
| Prednisone | Solution, intensol, tablets | Bitter taste |
| Methylpredm-solone (Medrol, Solu-Medrol) | Injection, long-acting injection, tablets, dosepak | |
| Prednisolone (Orapred) | solution, oral-disintegrating tablets, tablets | Orapred liquid must be refrigerated |
| Inhaled corticosteroids | ||
| Beclomethasone (QVAR) | MDI | |
| Budesonide (Pulmicort) | Inhaler (DPI) | |
| Ciclesonide (Alvesco) | MDI | |
| Flunisolide (Aerobid, Aerobid-M) | MDI | M formulation contains menthol as a flavoring agent |
| Mometasone (Asmanex) | DPI | |
| Fluticasone (Flovent HFA, Flovent Diskus) | HFA, DPI | |
| Triamcinolone (Azmacort) | MDI | Has a built-in spacer |
Short-term use of corticosteroids carries little risk of adverse effects, but long-term use is indicated only when the benefits outweigh the risks. Long-term oral corticosteroid use can lead to Cushing syndrome, which is characterized by a rounded, puffy face; thinning of the skin; osteoporosis (bone weakening); muscle loss; and high blood glucose. Therapeutic use of corticosteroids suppresses natural adrenal gland function, which is essential to the body in times of physical stress. The dose of oral corticosteroids must be tapered when they are to be discontinued so that the adrenal gland can recover and begin to secrete natural hormones.40
Other Agents for Treating Asthma. Two other classes of medications that may be used to treat asthma are the leukotriene modifiers and the mast cell stabilizers. The leukotriene modifiers cause the muscles in the bronchioles to relax, and tend to reduce inflammation. These agents are taken orally so they are not used in the treatment of acute exacerbations. Some patients who have difficulty using the inhaled products may prefer these dosage forms, but they are not considered first-line agents in the treatment of asthma. Montelukast (Singulair) is also FDA approved for the treatment of seasonal and perennial (year-round) allergies. Zileutin (Zyflo), which is the oldest agent in this class, has been shown to increase liver enzymes and patients need to be monitored while on this medication.40 The leukotriene modifiers tend to be well tolerated, with headache and GI upset being the main adverse effects noted.
Mast cell stabilizers may reduce the need for the use of beta2-agonists and may reduce asthma symptoms. They work by stabilizing the cell wall of the mast cells. This prevents the release of histamine and other mediators, which can cause bronchoconstriction. Cromolyn (Intal) is not used as much today because it must be taken several times a day, which is associated with poor patient compliance.40
Patients with asthma often use combinations of bronchodilators and corticosteroids. Patients should be able to identify which inhalers are meant to prevent an attack (i.e., “controllers”) and which inhalers are used to treat an acute attack (i.e., “quick-relief”). It is important that the patients are counseled on the importance of using their controller medications on a regular basis. Patients sometimes believe that these agents are not necessary since they don’t feel any different after taking them, but being compliant with these medications will decrease the need for quick-relief medications.
Cough and Cold Products. The common cold remains one of the most bothersome illnesses. More than 120 strains of viruses are responsible for causing the common cold. Most colds are self-limiting and can be self-treated. Treatment is aimed at reducing the symptoms: runny nose, sore throat, and cough. These symptoms are produced by an inflammatory response of the lining of the nose, throat, and lungs to the virus. Each of these symptoms may be treated individually or with combination agents when more than one symptom is present.
 Over-the-counter (OTC) cough and cold products are constantly changing ingredients and formulations. Always check the active ingredients and their strengths on the product to avoid dosing errors and drug duplication.
Over-the-counter (OTC) cough and cold products are constantly changing ingredients and formulations. Always check the active ingredients and their strengths on the product to avoid dosing errors and drug duplication.



